How Useful Are Our Dreams
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s In A Dream?
We were recently asked:
❝I have a question or a suggestion for coverage in your “Psychology Sunday”. Dreams: their relevance, meanings ( if any) interpretations? I just wondered what the modern psychological opinions are about dreams in general.❞
~ 10almonds subscriber
There are two main schools of thought, and one main effort to reconcile those two. The third one hasn’t quite caught on so far as to be considered a “school of thought” yet though.
The Top-Down Model (Psychoanalysts)
Psychoanalysts broadly follow the theories of Freud, or at least evolved from there. Freud was demonstrably wrong about very many things. Most of his theories have been debunked and ditched—hence the charitable “or at least evolved from there” phrasing when it comes to modern psychoanalytic schools of thought. Perhaps another day, we’ll go into all the ways Freud went wrong. However, for today, one thing he wasn’t bad at…
According to Freud, our dreams reveal our subconscious desires and fears, sometimes directly and sometimes dressed in metaphor.
Examples of literal representations might be:
- sex dreams (revealing our subconscious desires; perhaps consciously we had not thought about that person that way, or had not considered that sex act desirable)
- getting killed and dying (revealing our subconscious fear of death, not something most people give a lot of conscious thought to most of the time)
Examples of metaphorical representations might be:
- dreams of childhood (revealing our subconscious desires to feel safe and nurtured, or perhaps something else depending on the nature of the dream; maybe a return to innocence, or a clean slate)
- dreams of being pursued (revealing our subconscious fear of bad consequences of our actions/inactions, for example, responsibilities to which we have not attended, debts are a good example for many people; or social contact where the ball was left in our court and we dropped it, that kind of thing)
One can read all kinds of guides to dream symbology, and learn such arcane lore as “if you dream of your teeth crumbling, you have financial worries”, but the truth is that “this thing means that other thing” symbolic equations are not only highly personal, but also incredibly culture-bound.
For example:
- To one person, bees could be a symbol of feeling plagued by uncountable small threats; to another, they could be a symbol of abundance, or of teamwork
- One culture’s “crow as an omen of death” is another culture’s “crow as a symbol of wisdom”
- For that matter, in some cultures, white means purity; in others, it means death.
Even such classically Freudian things as dreaming of one’s mother and/or father (in whatever context) will be strongly informed by one’s own waking-world relationship (or lack thereof) with same. Even in Freud’s own psychoanalysis, the “mother” for the sake of such analysis was the person who nurtured, and the “father” was the person who drew the nurturer’s attention away, so they could be switched gender roles, or even different people entirely than one’s parents.
The only real way to know what, if anything, your dreams are trying to tell you, is to ask yourself. You can do that…
- by reflection and personal interrogation (see for example: The Easiest Way To Take Up Journaling)
- or by externalising parts of your subconscious (as in Internal Family Systems therapy)
- or by talking directly to your subconscious where it is, by means of lucid dreaming.
The idea with lucid dreaming is that since any dream character is a facet of your subconscious generated by your own mind, by talking to that character you can ask questions directly of your subconscious (the popular 2010 movie “Inception” was actually quite accurate in this regard, by the way).
To read more about how to do this kind of self-therapy through lucid dreaming, you might want to check out this book we reviewed previously; it is the go-to book of lucid dreaming enthusiasts, and will honestly give you everything you need in one go:
Lucid Dreaming: A Concise Guide to Awakening in Your Dreams and in Your Life – by Dr. Stephen LaBerge
The Bottom-Up Model (Neuroscientists)
This will take a lot less writing, because it’s practically a null hypothesis (i.e., the simplest default assumption before considering any additional evidence that might support or refute it; usually some variant of “nothing unusual going on here”).
The Bottom-Up model holds that our brains run regular maintenance cycles during REM sleep (a biological equivalent of defragging a computer), and the brain interprets these pieces of information flying by and, because of the mind’s tendency to look for patterns, fills in the rest (much like how modern generative AI can “expand” a source image to create more of the same and fill in the blanks), resulting in the often narratively wacky, but ultimately random, vivid hallucinations that we call dreams.
The Hybrid Model (per Cartwright, 2012)
This is really just one woman’s vision, but it’s an incredibly compelling one, that takes the Bottom-Up model and asks “what if we did all that bio-stuff, and then our subconscious mind influenced the interpretation of the random patterns, to create dreams that are subjectively meaningful, and thus do indeed represent our subconscious?
It’s best explained in her own words, though, so it’s time for another book recommendation (we’ve reviewed this one before, too):
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tasty Tabbouleh with Tahini
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tabbouleh is a salad, but it’s not “just a salad”. It’s a special kind of salad that’s as exciting for the tastebuds as it is healthy for the body and brain. Its core ingredients have been traditional for about a dozen generations, and seasonings are always a personal matter (not to mention that Lebanese tabbouleh-makers centuries ago might not have used miso and nooch, as we will today), but the overall feel of the Gestalt of tabbouleh seasonings remains the same, and this recipe is true to that.
You will need
For the tabbouleh:
- 1 cup bulgur wheat
- 1 cup plum tomatoes, chopped
- 1 cucumber, peeled and chopped (add the peel to a jug of water and put it in the fridge; this will be refreshing cucumber water later!)
- 1 cup chickpeas, cooked without salt
- 1/2 cup parsley, chopped
- 1/2 cup mint, chopped
- 2 spring onions, finely chopped
- 2oz fresh lemon juice
- 1 tsp white miso paste
- 1 tsp garlic powder
- 1 tsp ground cumin
- 1 tsp ground celery seeds
- 1 tsp ground nigella seeds
- 1 tsp ground black pepper
- 1 tsp MSG, or 1/2 tsp low sodium salt (you can find it in supermarkets, the sodium chloride is cut with potassium chloride to make it have less sodium and more potassium)
- 1 tbsp nutritional yeast (nooch), ground (it comes in flakes; you will have to grind it in a spice grinder or with a pestle and mortar)
For the tahini sauce:
- 3 garlic cloves, crushed
- 3 tbsp tahini
- 1 tbsp fresh lemon juice
- 1 tbsp white miso paste
- 1 tsp ground cumin
To serve:
- A generous helping of leafy greens; we recommend collard greens, but whatever works for you is good; just remember that dark green is best. Consider cavolo nero, or even kale if that’s your thing, but to be honest this writer doesn’t love kale
- 1 tsp coarsely ground nigella seeds
- Balsamic vinegar, ideally aged balsamic vinegar (this is thicker and sweeter, but unlike most balsamic vinegar reductions, doesn’t have added sugar).
Method
(we suggest you read everything at least once before doing anything)
1) Rinse the bulgur wheat and then soak it in warm water. There is no need to boil it; the warm water is enough to soften it and you don’t need to cook it (bulgur wheat has already been parboiled before it got to you).
2) While you wait, take a small bowl and mix the rest of the ingredients from the tabbouleh section (so, the lemon juice, miso paste, and all those ground spices and MSG/salt and ground nutritional yeast); you’re making a dressing out of all the ingredients here.
3) When the bulgur wheat is soft (expect it to take under 15 minutes), drain it and put it in a big bowl. Add the tomatoes, cucumber, chickpeas, parsley, mint, and spring onions. This now technically qualifies as tabbouleh already, but we’re not done.
4) Add the dressing to the tabbouleh and mix thoroughly but gently (you don’t want to squash the tomatoes, cucumber, etc). Leave it be for at least 15 minutes while the flavors blend.
5) Take the “For the tahini sauce” ingredients (all of them) and blend them with 4 oz water, until smooth. You’re going to want to drizzle this sauce, so if the consistency is too thick for drizzling, add a little more water and/or lemon juice (per your preference), 1 tbsp at a time.
6) Roughly chop the leafy greens and put them in a bowl big enough for the tabbouleh to join them there. The greens will serve as a bed for the tabbouleh itself.
7) Drizzle the tahini over the tabbouleh, and drizzle a little of the aged balsamic vinegar too.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
Take care!
Share This Post
-
Master Your Core – by Dr. Bohdanna Zazulak
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the category of “washboard abs”, this one isn’t particularly interested in how much or how little fat you have. What it’s more interested in is a strong, resilient, and stable core. Including your abs yes, but also glutes, hips, and back.
Nor is the focus on superhuman feats of strength, though certainly one could use these exercises to work towards that. Rather, here we see importance placed on functional performance, mobility, and stability.
Lest mobility and stability seem at odds with each other, understand:
- By mobility we mean the range of movement we are able to accomplish.
- By stability, we mean that any movement we make is intentional, and not because we lost our balance.
Functional performance, meanwhile, is a function of those two things, plus strength.
How does the book deliver on this?
There are exercises to do. Exercises of the athletic kind you might expect, and also exercises including breathing exercises, which gets quite a bit of attention too. Not just “do abdominal breathing”, but quite an in-depth examination of such. There are also habits to form, and lifestyle tweaks to make.
Of course, you don’t have to do all the things she suggests. The more you do, the better results you are likely to get, but if you adopt even some of the practices she recommends, you’re likely to see some benefits. And, perhaps most importantly, reduce age-related loss of mobility, stability, and strength.
Bottom line: a great all-rounder book of core strength, mobility, and stability.
Click here to check out Master Your Core and enjoy the more robust health that comes with it!
Share This Post
-
The Daily Stoic – by Ryan Holiday & Stephen Hanselman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s this, a philosophy book in a health and productivity newsletter? Well, look at it this way: Aristotle basically wrote the “How To Win Friends And Influence People” of his day, and Plato before him wrote a book about management.
In this (chiefly modern!) book, we see what the later Stoic philosophers had to say about getting the most out of life—which is also what we’re about, here at 10almonds!
We tend to use the word “stoic” in modern English to refer to a person who is resolute in the face of hardship. The traditional meaning does encompass that, but also means a lot more: a whole, rounded, philosophy of life.
Philosophy in general is not an easy thing into which to “dip one’s toe”. No matter where we try to start, it seems, it turns out there were a thousand other things we needed to read first!
This book really gets around that. The format is:
- There’s a theme for each month
- Each month has one lesson per day
- Each daily lesson starts with some words from a renowned stoic philosopher, and then provides commentary on such
- The commentary provides a jumping-off point and serves as a prompt to actually, genuinely, reflect and apply the ideas.
Unlike a lot of “a year of…” day-by-day books, this is not light reading, by the way, and you are getting a weighty tome for your money.
But, the page-length daily lessons are indeed digestible—which, again, is what we like at 10almonds!
Share This Post
Related Posts
-
How To Stay In Shape At 70
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Questions and Answers at 10almonds
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
I have a question: what are the pros and cons of older people (60+) taking creatine every day?
It depends what else you’re doing, as creatine mostly helps the muscles recover after exercise. So:
- iff you’re doing resistance training (such as weights or bodyweight training), or HIIT (High Intensity Interval Training), then creatine monohydrate may help you keep at that and keep doing well.
- if you’re just doing light-to-moderate exercises, you might not get much benefit from creatine!
The topic merits diving deeper though, so we’ll queue that for one of our “Research Review Monday” days!
I wanted to ask if you think marine collagen is decent to take. I’ve heard a lot of bad press about it
We don’t know what you’ve heard, but generally speaking it’s been found to be very beneficial to bones, joints, and skin! We wrote about it quite recently on a “Research Review Monday”:
See: We Are Such Stuff As Fish Are Made Of
Natural alternatives to medication for depression?
Great question! We did a mean feature a while back, but we definitely have much more to say! We’ll do another main feature soon, but in the meantime, here’s what we previously wrote:
See: The Mental Health First-Aid That You’ll Hopefully Never Need
^This covers not just the obvious, but also why the most common advice is not helpful, and practical tips to actually make manageable steps back to wellness, on days when “literally just survive the day” is one’s default goal.
I am now in the “aging” population. A great concern for me is Alzheimers. My father had it and I am so worried. What is the latest research on prevention?
One good thing to note is that while Alzheimer’s has a genetic component, it doesn’t appear to be hereditary per se. Still, good to be on top of these things, and it’s never too early to start with preventive measures!
You might like a main feature we did on this recently:
See: How To Reduce Your Alzheimer’s Risk
Side effects of statins, are they worth it? Depression, are antidepressants worth it?
About statins, that depends a lot on you, your circumstances, and—as it happens—your gender. We covered this in a main feature recently, but a short answer is: for most people, they may not be the best first choice, and could even make things worse. For some people, however, they really are just what’s needed.
- Factors that make them more likely better for you: being a man, or having atherosclerosis
- Factors that make them more likely worse for you: being a woman in general
Check out the main feature we did: Statins: His & Hers?
As for antidepressants? That depends a lot on you, your physiology, your depression, your circumstances, and more. We’ll definitely do a main feature on that sometime soon, as there’s a lot that most people don’t know!
I am interested in the following: Aging, Exercise, Diet, Relationships, Purpose, Lowering Stress
You’re going to love our Psychology Sunday editions of 10almonds!
You may particularly like some of these:
- Seriously Useful Communication Skills! ← this is about relationship stuff
- Lower Your Cortisol! (Here’s Why & How) ← about “the stress hormone”
- How To Set Your Anxiety Aside ← these methods work for stress too
(This coming Psychology Sunday will have a feature specifically on stress, so do make sure to read that when it comes out!)
Hair growth strategies for men combing caffeine and minoxidil?
Well, the strategy for that is to use caffeine and minoxidil! Some more specific tips, though:
- Both of those things need to be massaged (gently!) into your scalp especially around your hairline.
- In the case of caffeine, that boosts hair growth. No extra thought or care needed for that one.
- In the case of minoxidil, it reboots the hair growth cycle, so if you’ve only recently started, don’t be surprised (or worried) if you see more shedding in the first three months. It’s jettisoning your old hairs because new ones were just prompted (by the minoxidil) to start growing behind them. So: it will get briefly worse before it gets better, but then it’ll stay better… provided you keep using it.
- If you’d like other options besides minoxidil, finasteride is a commonly prescribed oral drug that blocks the conversion of testosterone to DHT, which latter is what tells your hairline to recede.
- If you’d like other options besides prescription drugs, saw palmetto performs comparably to finasteride (and works the same way).
- You may also want to consider biotin supplementation if you don’t already enjoy that
- Consider also using a dermaroller on your scalp. If you’re unfamiliar, this is a device that looks like a tiny lawn aerator, with many tiny needles, and you roll it gently across your skin.
- It can be used for promoting hair growth, as well as for reducing wrinkles and (more slowly) healing scars.
- It works by breaking up the sebum that may be blocking new hair growth, and also makes the skin healthier by stimulating production of collagen and elastin (in response to the thousands of microscopic wounds that the needles make).
- Sounds drastic, but it doesn’t hurt and doesn’t leave any visible marks—the needles are that tiny. Still, practise good sterilization and ensure your skin is clean when using it.
See: How To Use A Dermaroller ← also explains more of the science of it
PS: this question was asked in the context of men, but the information goes the same for women suffering from androgenic alepoceia—which is a lot more common than most people think!
How to get to sleep at night as fast and as naturally as possible? Thank you!
We’ll definitely write more on that! You might like these articles we wrote already, meanwhile:
- Beating The Insomnia Blues ← this one is general advice and tips
- Time For Some Pillow Talk ← this one compares and reviews some popular sleep apps
- Insomnia? High Blood Pressure? Try these! ← this one tackles the matter from a dietary angle
Q: How to be your best self after 60: Self motivation / Avoiding or limiting salt, sugar & alcohol: Alternatives / Ways to sneak in more movements/exercise
…and, from a different subscriber…
Q: Inflammation & over 60 weight loss. Thanks!
Here are some of our greatest hits on those topics:
- Where Nutrition Meets Habits ← focusing on food that’s all three of: healthy + easy + cheap
- How To Keep On Keeping On ← exercise tips for when the motivation wanes
- Keep Inflammation At Bay ← science-based tips and advice
Also, while we’ve recommended a couple of books on stopping (or reducing) drinking, we’ve not done a main feature on that, so we definitely will one of these days!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Little Treatments, Big Effects – by Dr. Jessica Schleider
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a clinical psychologist, discusses how mental healthcare has come a very long way, yet still has a long way to go. While advocating for top-down reforms, she does have a stopgap solution:
Find ways to significantly improve people’s mental health in a single-session intervention.
This seems like a tall order, but her method is based on good science, and also, most people will agree from experience that big changes can happen to someone in the space of moments, at pivotal turning points in life—they just have to be the right moments.
Dr. Schleider recommends that therapists train in (and then offer) this method, but she does also give comprehensive advice for self-therapy of this kind too.
These self-therapy directions, ways to induce those life-pivoting moments for the better, are perhaps the greatest value that the book gives us.
Bottom line: if you’d like a lot of the benefits of therapy without getting therapy, this book can definitely point you in the right direction, in a manner that won’t be a drain on your time or your wallet.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
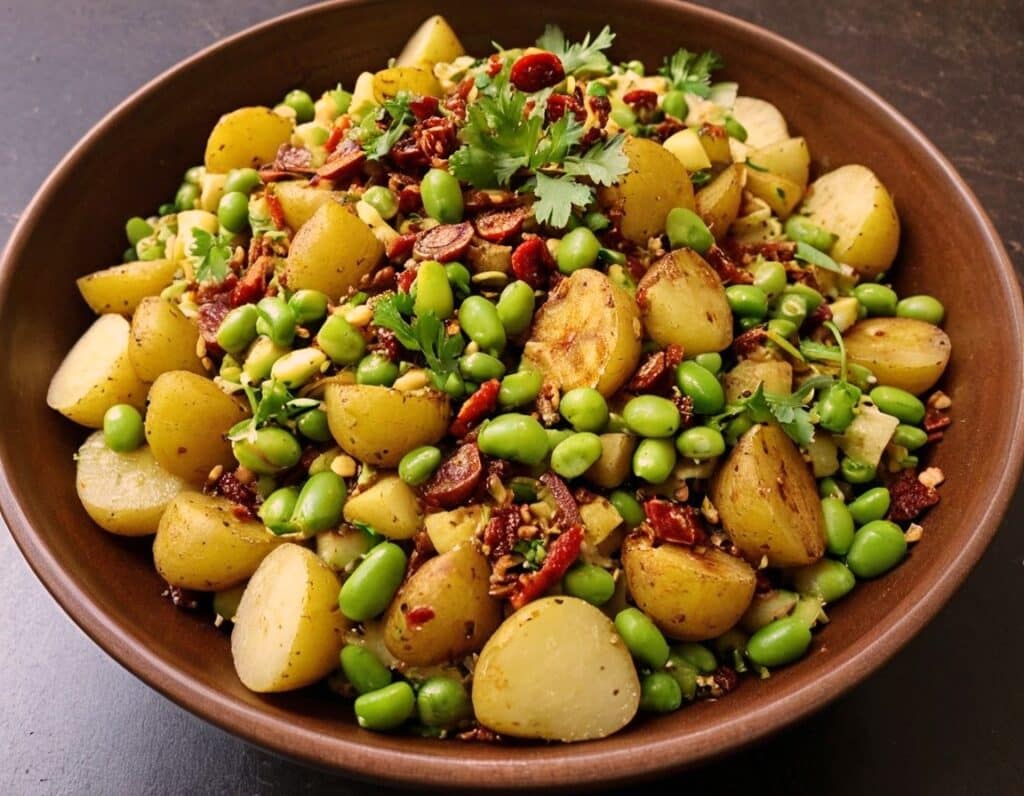
Chaat Masala Spiced Potato Salad With Beans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is an especially gut-healthy dish; the cooked-and-cooled potatoes are not rich with resistant starches (that’s good), the beans bring protein (as well as more fiber and micronutrients), and many of the spices bring their own benefits. A flavorful addition to your table!
You will need
- 1 lb new potatoes, boiled or steamed, with skin on, quartered, cooled ← this is a bit of a “mini recipe”, but we expect you can handle it
- 5 oz blanched broad beans
- 2 oz sun-dried tomatoes, chopped
- ¼ bulb garlic, crushed
- 1 tbsp extra virgin olive oil
- 2 tsp amchoor
- 2 tsp ground cumin
- 2 tsp ground coriander
- 1 tsp ground ginger
- 1 tsp ground asafoetida
- 1 tsp black pepper, coarse ground
- 1 tsp red chili powder
- 1 tsp ground turmeric
- ½ tsp MSG or 1 tsp low-sodium salt
- Juice of ½ lemon
And then…
- To garnish: finely chopped cilantro, or if you have the “cilantro tastes like soap” gene, then substitute with parsley
- To serve: a nice chutney; you can use our Spiced Fruit & Nut Chutney recipe
Method
(we suggest you read everything at least once before doing anything)
1) Mix all the ingredients from the main section, ensuring an even distribution on the spices.
2) Add the garnish, and serve with the chutney. That’s it. There was more work in the prep (and potentially, finding all the ingredients) today.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we scored all five today!
- Lycopene’s Benefits For The Gut, Heart, Brain, & More ← don’t underestimate those sun-dried tomatoes, either!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: