How To Avoid Carer Burnout (Without Dropping Care)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Avoid Carer Burnout
Sometimes in life we find ourselves in a caregiving role.
Maybe we chose it. For example, by becoming a professional carer, or even just by being a parent.
Oftentimes we didn’t. Sometimes because our own parents now need care from us, or because a partner becomes disabled.
Philosophical note: an argument could be made for that latter also having been a pre-emptive choice; we probably at some point said words to the effect of “in sickness and in health”, hopefully with free will, and hopefully meant it. And of course, sometimes we enter into a relationship with someone who is already disabled.
But, we are not a philosophy publication, and will henceforth keep to the practicalities.
First: are you the right person?
Sometimes, a caregiving role might fall upon you unasked-for, and it’s worth considering whether you are really up for it. Are you in a position to be that caregiver? Do you want to be that caregiver?
It may be that you do, and would actively fight off anyone or anything that tried to stop you. If so, great, now you only need to make sure that you are actually in a position to provide the care in question.
It may be that you do want to, but your circumstances don’t allow you to do as good a job of it as you’d like, or it means you have to drop other responsibilities, or you need extra help. We’ll cover these things later.
It may be that you don’t want to, but you feel obliged, or “have to”. If that’s the case, it will be better for everyone if you acknowledge that, and find someone else to do it. Nobody wants to feel a burden, and nobody wants someone providing care to be resentful of that. The result of such is two people being miserable; that’s not good for anyone. Better to give the job to someone who actually wants to (a professional, if necessary).
So, be honest (first with yourself, then with whoever may be necessary) about your own preferences and situation, and take steps to ensure you’re only in a caregiving role that you have the means and the will to provide.
Second: are you out of your depth?
Some people have had a life that’s prepared them for being a carer. Maybe they worked in the caring profession, maybe they have always been the family caregiver for one reason or another.
Yet, even if that describes you… Sometimes someone’s care needs may be beyond your abilities. After all, not all care needs are equal, and someone’s condition can (and more often than not, will) deteriorate.
So, learn. Learn about the person’s condition(s), medications, medical equipment, etc. If you can, take courses and such. The more you invest in your own development in this regard, the more easily you will handle the care, and the less it will take out of you.
And, don’t be afraid to ask for help. Maybe the person knows their condition better than you, and certainly there’s a good chance they know their care needs best. And certainly, there are always professionals that can be contacted to ask for advice.
Sometimes, a team effort may be required, and there’s no shame in that either. Whether it means enlisting help from family/friends or professionals, sometimes “many hands make light work”.
Check out: Caregiver Action Network: Organizations Near Me
A very good resource-hub for help, advice, & community
Third: put your own oxygen mask on first
Like the advice to put on one’s own oxygen mask first before helping others (in the event of a cabin depressurization in an airplane), the rationale is the same here. You can’t help others if you are running on empty yourself.
As a carer, sometimes you may have to put someone else’s needs above yours, both in general and in the moment. But, you do have needs too, and cannot neglect them (for long).
One sleepless night looking after someone else is… a small sacrifice for a loved one, perhaps. But several in a row starts to become unsustainable.
Sometimes it will be necessary to do the best you can, and accept that you cannot do everything all the time.
There’s a saying amongst engineers that applies here too: “if you don’t schedule time for maintenance, your equipment will schedule it for you”.
In other words: if you don’t give your body rest, your body will break down and oblige you to rest. Please be aware this goes for mental effort too; your brain is just another organ.
So, plan ahead, schedule breaks, find someone to take over, set up your cared-for-person with the resources to care for themself as well as possible (do this anyway, of course—independence is generally good so far as it’s possible), and make the time/effort to get you what you need for you. Sleep, distraction, a change of scenery, whatever it may be.
Lastly: what if it’s you?
If you’re reading this and you’re the person who has the higher care needs, then firstly:all strength to you. You have the hardest job here; let’s not forget that.
About that independence: well-intentioned people may forget that, so don’t be afraid to remind them when “I would prefer to do that myself”. Maintaining independence is generally good for the health, even if sometimes it is more work for all concerned than someone else doing it for you. The goal, after all, is your wellbeing, so this shouldn’t be cast aside lightly.
On the flipside: you don’t have to be strong all the time; nobody should.
Being disabled can also be quite isolating (this is probably not a revelation to you), so if you can find community with other people with the same or similar condition(s), even if it’s just online, that can go a very, very long way to making things easier. Both practically, in terms of sharing tips, and psychologically, in terms of just not feeling alone.
See also: How To Beat Loneliness & Isolation
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fast Diet, Fast Exercise, Fast Improvements
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
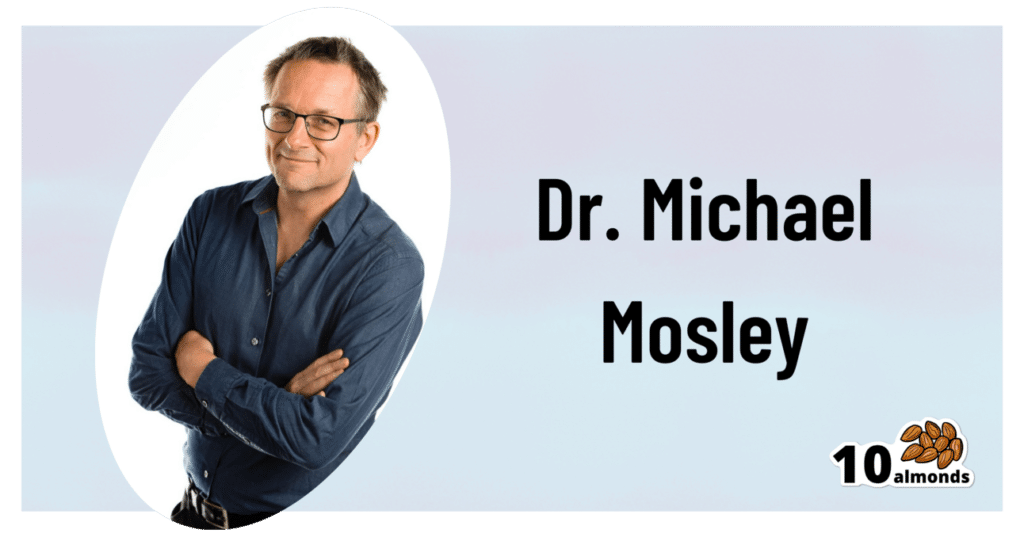
Diet & Exercise, Optimized
This is Dr. Michael Mosley. He originally trained in medicine with the intention of becoming a psychiatrist, but he grew disillusioned with psychiatry as it was practised, and ended up pivoting completely into being a health educator, in which field he won the British Medical Association’s Medical Journalist of the Year Award.
He also died under tragic circumstances very recently (he and his wife were vacationing in Greece, he went missing while out for a short walk on the 5th of June, appears to have got lost, and his body was found 100 yards from a restaurant on the 9th). All strength and comfort to his family; we offer our small tribute here today in his honor.
The “weekend warrior” of fasting
Dr. Mosley was an enjoyer (and proponent) of intermittent fasting, which we’ve written about before:
Fasting Without Crashing? We Sort The Science From The Hype
However, while most attention is generally given to the 16:8 method of intermittent fasting (fast for 16 hours, eat during an 8 hour window, repeat), Dr. Mosley preferred the 5:2 method (which generally means: eat at will for 5 days, then eat a reduced calorie diet for the other 2 days).
Specifically, he advocated putting that cap at 800 kcal for each of the weekend days (doesn’t have to be specifically the weekend).
He also tweaked the “eat at will for 5 days” part, to “eat as much as you like of a low-carb Mediterranean diet for 5 days”:
❝The “New 5:2” approach involves restricting calories to 800 on fasting days, then eating a healthy lower carb, Mediterranean-style diet for the rest of the week.
The beauty of intermittent fasting means that as your insulin sensitivity returns, you will feel fuller for longer on smaller portions. This is why, on non-fasting days, you do not have to count calories, just eat sensible portions. By maintaining a Mediterranean-style diet, you will consume all of the healthy fats, protein, fibre and fresh plant-based food that your body needs.❞
Read more: The Fast 800 | The New 5:2
And about that tweaked Mediterranean Diet? You might also want to check out:
Four Ways To Upgrade The Mediterranean Diet
Knowledge is power
Dr. Mosley encouraged the use of genotyping tests for personal health, not just to know about risk factors, but also to know about things such as, for example, whether you have the gene that makes you unable to gain significant improvements in aerobic fitness by following endurance training programs:
The Real Benefit Of Genetic Testing
On which note, he himself was not a fan of exercise, but recognised its importance, and instead sought to minimize the amount of exercise he needed to do, by practising High Intensity Interval Training. We reviewed a book of his (teamed up with a sports scientist) not long back; here it is:
Fast Exercise: The Simple Secret of High Intensity Training – by Dr. Michael Mosley & Peta Bee
You can also read our own article on the topic, here:
How To Do HIIT (Without Wrecking Your Body)
Just One Thing…
As well as his many educational TV shows, Dr. Mosley was also known for his radio show, “Just One Thing”, and a little while ago we reviewed his book, effectively a compilation of these:
Just One Thing: How Simple Changes Can Transform Your Life – by Dr. Michael Mosley
Enjoy!
Share This Post
-
Testosterone, Tourette’s, and Tickly Throats
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Could you do a series on mens health? Testosterone boosters. Libido? What works what doesnt? Also could you discuss prostate health and what supplements, meds, foods or protocols work to relieve symptoms of bph❞
We could indeed! We’ll be sure to write more, but while you’re waiting, you might like to read our main feature from a while back:
Too Much Or Too Little Testosterone?
…as it does include a lot about the use of a supplement that helps against Benign Prostatic Hyperplasia, with performance comparable to the most common drug prescribed for such.
And since (like that drug) it’s a 5α-reductase inhibitor (meaning it works by blocking the conversion of testosterone to DHT), this means it helps against prostate problems (and also, incidentally, male pattern hair loss) without reducing overall testosterone levels. In fact, because less testosterone will be converted to DHT, you’ll actually (all other things being equal) end up with slightly higher free testosterone levels.
❝My BMI is fine, but my waist is too big. What do I do about that? I am 5′ 5″ tall and 128 pounds and 72 years old.❞
It’s hard to say without knowing about your lifestyle (and hormones, for that matter)! But, extra weight around the middle in particular is often correlated with high levels of cortisol, so you might find this of benefit:
Lower Your Cortisol! (Here’s Why & How)
❝Is there anything special that might help someone with Tourette’s syndrome?❞
There are of course a lot of different manifestations of Tourette’s syndrome, and some people’s tics may be far more problematic to themselves and/or others, while some may be quite mild and just something to work around.
It’s an interesting topic for sure, so we’ll perhaps do a main feature (probably also covering the related-and-sometimes-overlapping OCD umbrella rather than making it hyperspecific to Tourette’s), but meanwhile, you might consider some of these options:
- Deep Brain Stimulation (DBS)
- Medications/ Pharmacology
- Comprehensive Behavioral Intervention for Tics (CBIT)
- Speech Therapies
❝Natural solutions for osteoarthritis. Eg. Rosehip tea, dandelion root tea. Any others??? What foods should I absolutely leave alone?❞
We’ll do a main feature on arthritis (in both its main forms) someday soon, but meanwhile, we recommend eating for good bone/joint health and against inflammation. To that end, you might like these main features we did on those topics:
- We Are Such Stuff As Fish Are Made Of (collagen for bone and joint health)
- The Bare-Bones Truth About Osteoporosis (eating for bone health generally)
- Keep Inflammation At Bay (dietary tips for minimizing inflammation—also, our all-time most popular article to date!)
Of these, probably the last one is the most critical, and also will have the speediest effects if implemented.
We turn the tables and ask you a question!
We’ll then talk about this tomorrow:
Share This Post
-
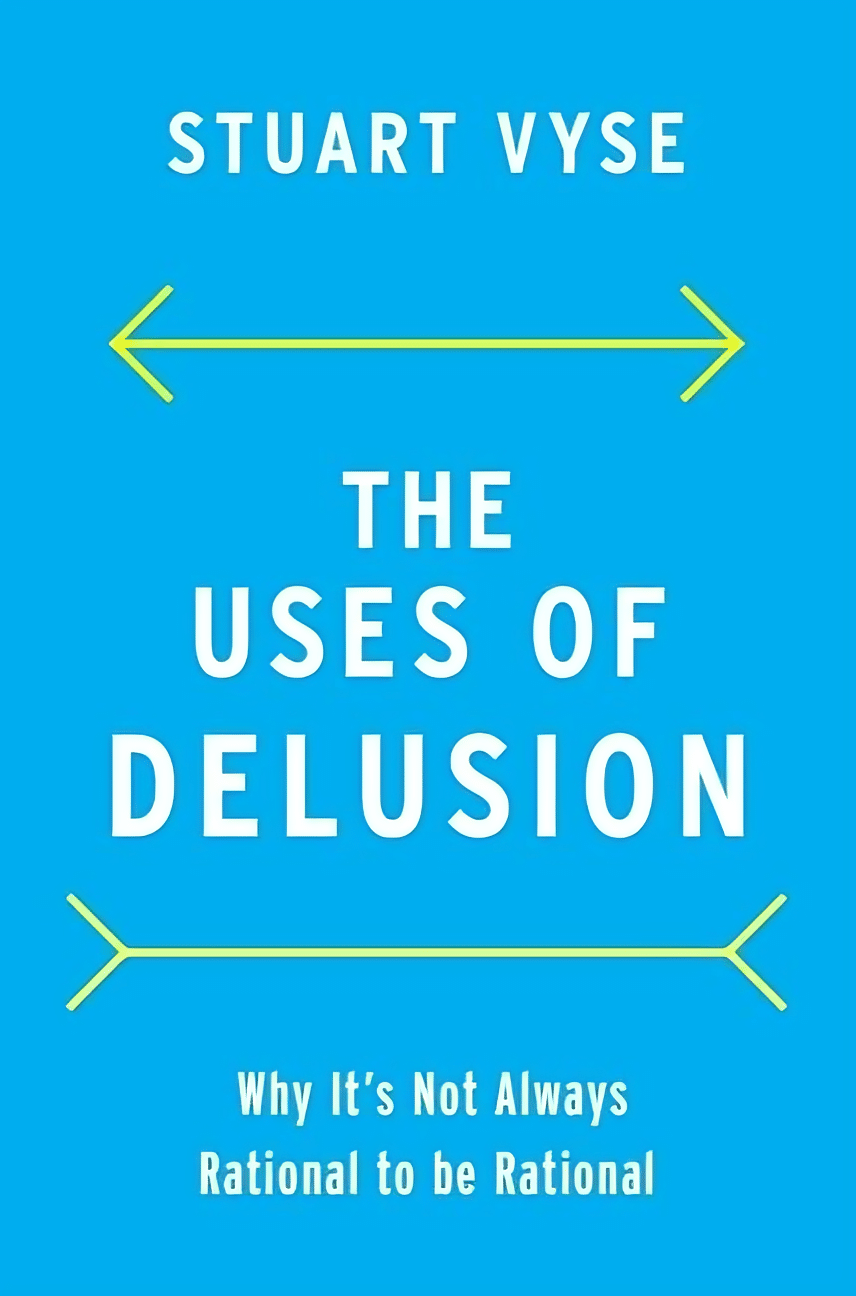
The Uses of Delusion – by Dr. Stuart Vyse
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most of us try to live rational lives. We try to make the best decisions we can based on the information we have… And if we’re thoughtful, we even try to be aware of common logical fallacies, and overcome our personal biases too. But is self-delusion ever useful?
Dr. Stuart Vyse, psychologist and Fellow for the Committee for Skeptical Inquiry, argues that it can be.
From self-fulfilling prophecies of optimism and pessimism, to the role of delusion in love and loss, Dr. Vyse explores what separates useful delusion from dangerous irrationality.
We also read about such questions as (and proposed answers to):
- Why is placebo effect stronger if we attach a ritual to it?
- Why are negative superstitions harder to shake than positive ones?
- Why do we tend to hold to the notion of free will, despite so much evidence for determinism?
The style of the book is conversational, and captivating from the start; a highly compelling read.
Bottom line: if you’ve ever felt yourself wondering if you are deluding yourself and if so, whether that’s useful or counterproductive, this is the book for you!
Click here to check out The Uses of Delusion, and optimize yours!
Share This Post
Related Posts
-
5 Minute Posture Improvement Routine!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
McKay Lang walks us through it:
Step by Step
Breathing exercise:
- Place your hands on your lower abdomen.
- Take three deep breaths, focusing on body tension in the shoulders and neck… And release.
Shoulder squeeze:
- With your hands on your hips, inhale and squeeze your shoulders upwards.
- Hold your breath for 3–4 seconds, then exhale.
- Repeat two more times, holding the squeeze a little longer each time.
Upper shoulder massage:
- Massage your upper shoulder muscles to release tension stored there.
Overhead arm stretch:
- Raise your arms above your head, clasping each elbow with the opposite hand.
- Inhale deeply, stretch upwards, then exhale and release.
- Repeat, alternating elbows.
Neck and head push:
- Place your palms on the back of the head, and push your head into your hands (and vice versa, because of Newton’s Third Law of Motion).
- Do the same sideways (one side and then the other), to engage the other neck muscles.
Cool down:
- Gently unclasp your hands, bring your head upright, and massage your muscles. And breathe.
For variations and a visual demonstration of all, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
6 Ways To Look After Your Back
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cold Weather Health Risks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many Are Cold; Few Are Frozen
Many of those of us in the Northern Hemisphere are getting hit with a cold spell around now. How severe that may be depends on more precisely where we are, but it’s affecting a lot of people. So, with apologies to our readers in Australia, we’re going to do a special on that today.
Acute cold is, for most people, good for the health:
A Cold Shower A Day Keeps The Doctor Away?
Persistent cold, not so much. Let’s look at the risks, and what can be done about them…
Hypothermia
It kills. Don’t let it kill you or your loved ones.
And, this is really important: it doesn’t care whether you’re on a mountain or not.
In other words: a lot of people understand (correctly!) that hypothermia is a big risk to hikers, climbers, and the like. But if the heating goes out in your house and the temperature drops for long enough before the heating is fixed, you can get hypothermia there too just the same if you’re not careful.
How cold is too cold? It doesn’t even have to be sub-zero. According to the CDC, temperatures of 4℃ (40℉) can be low enough to cause hypothermia if other factors combine:
CDC | Prevent Hypothermia & Frostbite ← you can also see the list of symptoms to watch out for, there!
Skin health
Not generally an existential risk, but we may as well stay healthy as not!
Cold air often means dry air, so use a moisturizer with an oil base (if you don’t care for fancy beauty products, ordinary coconut oil is top-tier).
Bonus if you do it after a warming bath/shower!
Heart health
Cold has a vasconstricting effect; that is to say, it causes the body’s vasculature to shrink, increasing localized blood pressure. If it’s a cold shower as above, that can be very invigorating. If it’s a week of sub-zero temperatures, it can become a problem.
❝Shoveling a little snow off your sidewalk may not seem like hard work. However, […] combined with the fact that the exposure to cold air can constrict blood vessels throughout the body, you’re asking your heart to do a lot more work in conditions that are diminishing the heart’s ability to function at its best.❞
Source: Snow shoveling, cold temperatures combine for perfect storm of heart health hazards
If you have a heart condition, please do not shovel snow. Let someone else do it, or stay put.
And if you are normally able to exercise safely? Unless you’re sure your heart is in good order, exercising in the warmth, not the cold, seems to be the best bet.
See also: Heart Attack: His & Hers (Be Prepared!) ← can you remember which symptoms are for which sex? If not, now’s a good time to refresh that knowledge.
Immune health
We recently discussed how cold weather indirectly increases the risk of respiratory viral infection:
The Cold Truth About Respiratory Infections
So, now’s the time to be extra on-guard about that.
See also: Beyond Supplements: The Real Immune-Boosters!
Balance
Icy weather increases the risk of falling. If you think “having a fall” is something that happens to other/older people, please remember that there’s a first time for everything. Some tips:
- Walk across icy patches with small steps in a flat-footed fashion like a penguin.
- It may not be glamorous, but neither is going A-over-T and breaking (or even just spraining) things.
- Use a handrail if available, even if you don’t think you need to.
You can also check out our previous article about falling (avoiding falling, minimizing the damage of falling, etc):
Fall Special: Some Fall-Themed Advice
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Walk across icy patches with small steps in a flat-footed fashion like a penguin.
-
Pinch of Nom – by Kate Allinson & Kay Allinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Home-style recipes”, because guess where most readers live!
And: slimming, because trimming the waistline a little is a goal for many after holiday indulgences.
The key idea here is healthy recipes that “don’t taste like diet food”—often by just switching out a couple of key ingredients, to give a significantly improved nutritional profile while remaining just as tasty, especially when flavors are enhanced with clever spicing and seasoning.
The food is simple to prepare, while being “special” enough that it could be used very credibly for entertaining too. For that matter, a strength of the book is its potential for use as a creative springboard, if you’re so inclined—there are lots of good ideas in here.
The recipes themselves are all you’d expect them to be, and presented clearly in an easy-to-follow manner.
Bottom line: if you’ve ever wanted to cook healthily but you need dinner on the table in the very near future and are stuck for ideas, this book is exactly what you need.
Click here to check out Pinch of Nom, and liven up your healthy cooking!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: