We Are Such Stuff As Fish Are Made Of
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Research Review: Collagen
For something that’s a very popular supplement, not many people understand what collagen is, where it comes from, or what it does.
In a nutshell:
Collagen is a kind of protein. Our bodies make it naturally, and we can also get more in our diet and/or take extra as a supplement.
Our bodies use collagen in connective tissue, skin, tendon, bone, and cartilage. It has many functions, but a broad description would be “holding things together”.
As we get older, our bodies produce less collagen. Signs of this include wrinkles, loss of skin hydration, and joint pain.
Quick test: pinch the skin on the middle of the back of one of your hands, and then watch what happens when you get low. How quickly and easily did your skin returns to its original shape?
If it was pretty much instantanous and flawless, congratulations, you have plenty of collagen (and also elastin). If you didn’t, you are probably low on both!
(they are quite similar proteins and are made from the same base “stuff”, so if you’re low on one, you’ll usually be low on both)
Quick note: A lot of research out there has been funded by beauty companies, so we had our work cut out for us today, and have highlighted where any research may be biased.
More than skin deep
While marketing for collagen is almost exclusively aimed at “reduce wrinkles and other signs of aging”, it does a lot more than that.
You remember we mentioned that many things from the bones outward are held together by collagen? We weren’t kidding…
Read: Osteoporosis, like skin ageing, is caused by collagen loss which is reversible
Taking extra collagen isn’t the only way
We can’t (yet!) completely halt the age-related loss of collagen, but we can slow it, with our lifestyle choices:
- Don’t smoke tobacco
- Drink only in moderation (or not at all)
- Avoid foods with added sugar, and high-processed foods in general
- Wear sunscreen when appropriate
Can I get collagen from food?
Yep! Just as collagen holds our bodies together, it holds the bodies of other animals together. And, just like collagen is found in most parts of our body but most plentifully in our skin and bones, that’s what to eat to get collagen from other animals, e.g:
- Chicken skin
- Fish skin
- Bone broth ← health benefits and recipes at this link!
What about vegans?
Yes, vegans are also held together by collagen! We do not, however, recommend eating their skin or boiling their bones into broth. Ethical considerations aside, cannibalism can give you CJD!
More seriously, if you’re vegan, you can’t get collagen from a plant-based diet, but you can get the stuff your body uses to make collagen. Basically, you want to make sure you get plenty of:
- Protein (beans, pulses, nuts, etc are all fine; it’s hard to go wrong with this)
- Vitamin C
- Vitamin D
- and Zinc
Just be sure to continue to remember to avoid highly-processed foods. So:
- Soy mince/chunks whose ingredients list reads: “soya”? Yes!
- The Incredible Burger or Linda McCartney’s Sausages? Sadly less healthy
Read: Advanced Glycation End Products in Foods and a Practical Guide to Their Reduction in the Diet
Meat-eaters might want to read that one too. By far the worst offenders for AGEs (Advanced Glycation End Products, which can not only cause collagen to stiffen, but also inactivate proteins responsible for collagen repair, along with doing much more serious damage to your body’s natural functions) include:
- Hot dogs
- Bacon
- Fried/roasted/grilled meats
Is it worth it as a supplement?
That depends on you, your age, and your lifestyle, but it’s generally considered safe*
*if you have a seafood allergy, be careful though, as many supplements are from fish or shellfish—you will need to find one that’s free from your allergen
Also, all collagen is animal-derived. So if you’re a vegan, decide for yourself whether this constitutes medicine and if so, whether that makes it ethically permissible to you.
With that out of the way:
What the science says on collagen supplementation
Collagen for skin
Read: Effects of collagen supplementation on skin aging (systematic review and meta-analysis)
The short version is that they selected 19 studies with over a thousand participants in total, and they found:
In the meta-analysis, a grouped analysis of studies showed favorable results of hydrolyzed collagen supplementation compared with placebo in terms of skin hydration, elasticity, and wrinkles.
The findings of improved hydration and elasticity were also confirmed in the subgroup meta-analysis.
Based on results, ingestion of hydrolyzed collagen for 90 days is effective in reducing skin aging, as it reduces wrinkles and improves skin elasticity and hydration.
Caveat: while that systematic review had no conflicts of interests, at least some of the 19 studies will have been funded by beauty companies. Here are two, so that you know what that looks like:
Funded by Quiris to investigate their own supplement, Elasten®:
A Collagen Supplement Improves Skin Hydration, Elasticity, Roughness, and Density
Funded by BioCell to investigate their own supplement, BioCell Collagen:
The Effects of Skin Aging Associated with the Use of BioCell Collagen
A note on funding bias: to be clear, the issue is not that the researchers might be corrupt (though that could happen).
The issue is more that sometimes companies will hire ten labs to do ten research studies… and then pull funding from ones whose results aren’t going the way they’d like.
So the “best” (for them) study is the one that gets published.
Here’s another systematic review—like the one at the top of this section—that found the same, with doses ranging from 2.5g–15g per day for 8 weeks or longer:
Read: Oral Collagen Supplementation: A Systematic Review of Dermatological Applications
Again, some of those studies will have been funded by beauty companies. The general weight of evidence does seem clear and favorable, though.
Collagen for bones
Here, we encountered a lot less in the way of potential bias, because this is simply marketed a lot less. Despite being arguably far more important!
We found a high quality multi-vector randomized controlled study with a sample size of 131 postmenopausal women. They had these women take 5g collagen supplement (or placebo), and studied the results over the course of a year.
They found:
- The intake of the supplement increased bone mineral density (BMD)
- Supplementation was also associated with a favorable shift in bone markers, indicating:
- increased bone formation
- reduced bone degradation
Read: Specific Collagen Peptides Improve Bone Mineral Density and Bone Markers in Postmenopausal Wome
A follow-up study with 31 of these women found that taking 5 grams of collagen daily for a total of 4 years was associated with a progressive increase in BMD.
You might be wondering if collagen also helps against osteoarthritis.
The answer is: yes, it does (at least, it significantly reduces the symptoms)
Read: Effect of collagen supplementation on osteoarthritis symptoms
In summary:
- You need collagen for health skin, bones, joints, and more
- Your body makes collagen from your food
- You can help it by getting plenty of protein, vitamins, and minerals
- You can also help it by not doing the usual Bad Things™ (smoking, drinking, eating processed foods, especially processed meats)
- You can also eat collagen directly in the form of other animals’ skin and bones
- You can also buy collagen supplements (but watch out for allergens)
Want to try collagen supplementation?
We don’t sell it (or anything else), but for your convenience…
Check it out: Hydrolyzed Collagen Peptides (the same as in most of the above studies), 90 days supply at 5g/day
We selected this one because it’s the same kind used in many of the studies, and it doesn’t contain any known allergens.
It’s bovine collagen, meaning it’s from cows, so it’s not vegan, and also some subscribers may want to abstain for religious reasons. We respect that, and/but make our recommendations based solely on the science of health and productivity.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Yoga Nidra Made Easy – by Dr. Uma Dinsmore-Tuli and Nirlipta Tuli
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about yoga before, and about sleep. This one’s different.
It’s about a yogic practice that can be used to promote restful sleep—or just be a non-sleeping exercise that nonetheless promotes relaxation and recuperation.
While yoga nidra is as somatic as it is psychological, its corporeal aspects are all explored in a lying-down-on-one’s-back state. This isn’t a book of stretches and poses and such—those are great, but are simply not needed for this practice.
The authors explain, step-by-step, simply and clearly, how to practice yoga nidra, and get out of it what you want to (there are an assortment of possible outcomes, per your preference; there are options to choose along the way).
A lot of books about yoga, even when written in English, contain a lot of Sanskrit terms. This one doesn’t. And, that difference goes a long way to living up to the title of making this easy, for those of us who regrettably don’t read even transliterated Sanskrit.
Bottom line: if ever you struggle to relax, struggle to sleep, or struggle to find your get-up-and-go, this book provides all you need to engage in this very restorative practice!
Click here to check out Yoga Nidra Made Easy, and learn this restorative tool for yourself!
Share This Post
-
Neuroaffirming care values the strengths and differences of autistic people, those with ADHD or other profiles. Here’s how
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve come a long way in terms of understanding that everyone thinks, interacts and experiences the world differently. In the past, autistic people, people with attention deficit hyperactive disorder (ADHD) and other profiles were categorised by what they struggled with or couldn’t do.
The concept of neurodiversity, developed by autistic activists in the 1990s, is an emerging area. It promotes the idea that different brains (“neurotypes”) are part of the natural variation of being human – just like “biodiversity” – and they are vital for our survival.
This idea is now being applied to research and to care. At the heart of the National Autism Strategy, currently in development, is neurodiversity-affirming (neuroaffirming) care and practice. But what does this look like?
Unsplash Reframing differences
Neurodiversity challenges the traditional medical model of disability, which views neurological differences solely through a lens of deficits and disorders to be treated or cured.
Instead, it reframes it as a different, and equally valuable, way of experiencing and navigating the world. It emphasises the need for brains that are different from what society considers “neurotypical”, based on averages and expectations. The term “neurodivergent” is applied to Autistic people, those with ADHD, dyslexia and other profiles.
Neuroaffirming care can take many forms depending on each person’s needs and context. It involves accepting and valuing different ways of thinking, learning and experiencing the world. Rather than trying to “fix” or change neurodivergent people to fit into a narrow idea of what’s considered “normal” or “better”, neuroaffirming care takes a person-centered, strengths-based approach. It aims to empower and support unique needs and strengths.
Neuroaffirming care can look different in a school or clinical setting. Shutterstock/Inna Reznik Adaptation and strengths
Drawing on the social model of disability, neuroaffirming care acknowledges there is often disability associated with being different, especially in a world not designed for neurodivergent people. This shift focuses away from the person having to adapt towards improving the person-environment fit.
This can include providing accommodations and adapting environments to make them more accessible. More importantly, it promotes “thriving” through greater participation in society and meaningful activities.
At school, at work, in clinic
In educational settings, this might involve using universal design for learning that benefits all learners.
For example, using systematic synthetic phonics to teach reading and spelling for students with dyslexia can benefit all students. It also could mean incorporating augmentative and alternative communication, such as speech-generating devices, into the classroom.
Teachers might allow extra time for tasks, or allow stimming (repetitive movements or noises) for self-regulation and breaks when needed.
In therapy settings, neuroaffirming care may mean a therapist grows their understanding of autistic culture and learns about how positive social identity can impact self-esteem and wellbeing.
They may make efforts to bridge the gap in communication between different neurotypes, known as the double empathy problem. For example, the therapist may avoid relying on body language or facial expressions (often different in autistic people) to interpret how a client is feeling, instead of listening carefully to what the client says.
Affirming therapy approaches with children involve “tuning into” their preferred way of communicating, playing and engaging. This can bring meaningful connection rather than compliance to “neurotypical” ways of playing and relating.
In workplaces, it can involve flexible working arrangements (hours, patterns and locations), allowing different modes of communication (such as written rather than phone calls) and low-sensory workspaces (for example, low-lighting, low-noise office spaces).
In public spaces, it can look like providing a “sensory space”, such as at large concerts, where neurodivergent people can take a break and self-regulate if needed. And staff can be trained to recognise, better understand and assist with hidden disabilities.
Combining lived experience and good practice
Care is neuroaffirmative when it centres “lived experience” in its design and delivery, and positions people with disability as experts.
As a result of being “different”, people in the neurodivergent community experience high rates of bullying and abuse. So neuroaffirming care should be combined with a trauma-informed approach, which acknowledges the need to understand a person’s life experiences to provide effective care.
Culturally responsive care acknowledges limited access to support for culturally and racially marginalised Autistic people and higher rates of LGBTQIA+ identification in the neurodivergent community.
In the workplace, we can acknowledge how difference can fuel ideas. Unsplash/Jason Goodman Authentic selves
The draft National Autism Strategy promotes awareness that our population is neurodiverse. It hopes to foster a more inclusive and understanding society.
It emphasises the societal and public health responsibilities for supporting neurodivergent people via public education, training, policy and legislation. By providing spaces and places where neurodivergent people can be their authentic, unmasked selves, we are laying the foundations for feeling seen, valued, safe and, ultimately, happy and thriving.
The author would like to acknowledge the assistance of psychologist Victoria Gottliebsen in drafting this article. Victoria is a member of the Oversight Council for the National Autism Strategy.
Josephine Barbaro, Associate Professor, Principal Research Fellow, Psychologist, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Can You Reverse Gray Hair? A Dermatologist Explains
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Betteridge’s Law of Headlines states “any headline that ends in a question mark can be answered by the word no“—it’s not really a universal truth, but it’s true surprisingly often, and, as board certified dermatologist “The Beauty MD” Dr. Sam Ellis explains, it’s true in this case.
But, all is not lost.
Physiological Factors
Hair color is initially determined by genes and gene expression, instructing the body to color it with melanin (brown and black) and/or pheomelanin (blonde and red). If and when the body produces less of those pigments, our hair will go gray.
Factors that affect if/when our hair will go gray include:
- Genetics: primary determinant, essentially a programmed change
- Age: related to the above, but critically, the probability of going gray in any given year increases with age
- Ethnicity: the level of melanin in our skin is an indicator of how long we are likely to maintain melanin in our hair. Black people with the darkest skintones will thus generally go gray last, whereas white people with the lightest skintones will generally go gray first, and so on for a spectrum between the two.
- Medical conditions: immune conditions such as vitiligo, thyroid disease, and pernicious anemia promote an earlier loss of pigmentation
- Stress: oxidative stress, mainly, so factors like smoking will cause earlier graying. But yes, also chronic emotional stress does lead to oxidative stress too. Interestingly, this seems to be more about norepinephrine than cortisol, though.
- Nutrient deficiencies: the body can make a lot of things, but it needs the raw ingredients. Not having the right amounts of important vitamins and minerals will result in a loss of pigmentation (amongst other more serious problems). Vitamins B6, B9, and B12 are talked about in the video, as are iron and zinc. Copper is also needed for some hair colors. Selenium is needed for good hair health in general (but not too much, as an excess of selenium paradoxically causes hair loss), and many related things will stop working properly without adequate magnesium. Hair health will also benefit a lot from plenty of vitamin B7.
So, managing the above factors (where possible; obviously some of the above aren’t things we can influence) will result in maintaining one’s hair pigment for longer. As for texture, by the way, the reason gray hair tends to have a rougher texture is not for the lack of pigment itself, but is due to decreased sebum production. Judicious use of exogenous hair oils (e.g. argan oil, coconut oil, or whatever your preference may be) is a fine way to keep your grays conditioned.
However, once your hair has gone gray, there is no definitive treatment with good evidence for reversing that, at present. Dye it if you want to, or don’t. Many people (including this writer, who has just a couple of streaks of gray herself) find gray hair gives a distinguished look, and such harmless signs of age are a privilege not everyone gets to reach, and thus may be reasonably considered a cause for celebration
For more on all of the above, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
Related Posts
-
Managing Sibling Relationships In Adult Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Managing Sibling Relationships In Adult Life
After our previous main feature on estrangement, a subscriber wrote to say:
❝Parent and adult child relationships are so important to maintain as you age, but what about sibling relationships? Adult choices to accept and move on with healthier boundaries is also key for maintaining familial ties.❞
And, this is indeed critical for many of us, if we have siblings!
Writer’s note: I don’t have siblings, but I do happen to have one of Canada’s top psychologists on speed-dial, and she has more knowledge about sibling relationships than I do, not to mention a lifetime of experience both personally and professionally. So, I sought her advice, and she gave me a lot to work with.
Today I bring her ideas, distilled into my writing, for 10almonds’ signature super-digestible bitesize style.
A foundation of support
Starting at the beginning of a sibling story… Sibling relationships are generally beneficial from the get-go.
This is for reasons of mutual support, and an “always there” social presence.
Of course, how positive this experience is may depend on there being a lack of parental favoritism. And certainly, sibling rivalries and conflict can occur at any age, but the stakes are usually lower, early in life.
Growing warmer or colder
Generally speaking, as people age, sibling relationships likely get warmer and less conflictual.
Why? Simply put, we mature and (hopefully!) get more emotionally stable as we go.
However, two things can throw a wrench into the works:
- Long-term rivalries or jealousies (e.g., “who has done better in life”)
- Perceptions of unequal contribution to the family
These can take various forms, but for example if one sibling earns (or otherwise has) much more or much less than another, that can cause resentment on either or both sides:
- Resentment from the side of the sibling with less money: “I’d look after them if our situations were reversed; they can solve my problems easily; why do they resent that and/or ignore my plight?”
- Resentment from the side of the sibling with more money: “I shouldn’t be having to look after my sibling at this age”
It’s ugly and unpleasant. Same goes if the general job of caring for an elderly parent (or parents) falls mostly or entirely on one sibling. This can happen because of being geographically closer or having more time (well… having had more time. Now they don’t, it’s being used for care!).
It can also happen because of being female—daughters are more commonly expected to provide familial support than sons.
And of course, that only gets exacerbated as end-of-life decisions become relevant with regard to parents, and tough decisions may need to be made. And, that’s before looking at conflicts around inheritance.
So, all that seems quite bleak, but it doesn’t have to be like that.
Practical advice
As siblings age, working on communication about feelings is key to keeping siblings close and not devolving into conflict.
Those problems we talked about are far from unique to any set of siblings—they’re just more visible when it’s our own family, that’s all.
So: nothing to be ashamed of, or feel bad about. Just, something to manage—together.
Figure out what everyone involved wants/needs, put them all on the table, and figure out how to:
- Make sure outright needs are met first
- Try to address wants next, where possible
Remember, that if you feel more is being asked of you than you can give (in terms of time, energy, money, whatever), then this discussion is a time to bring that up, and ask for support, e.g.:
“In order to be able to do that, I would need… [description of support]; can you help with that?”
(it might even sometimes be necessary to simply say “No, I can’t do that. Let’s look to see how else we can deal with this” and look for other solutions, brainstorming together)
Some back-and-forth open discussion and even negotiation might be necessary, but it’s so much better than seething quietly from a distance.
The goal here is an outcome where everyone’s needs are met—thus leveraging the biggest strength of having siblings in the first place:
Mutual support, while still being one’s own person. Or, as this writer’s psychology professor friend put it:
❝Circling back to your original intention, this whole discussion adds up to: siblings can be very good or very bad for your life, depending on tons of things that we talked about, especially communication skills, emotional wellness of each person, and the complexity of challenges they face interdependently.❞
Our previous main feature about good communication can help a lot:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How to Fall Back Asleep After Waking Up in the Middle of the Night
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Michael Bruce, the Sleep Doctor, addresses a common concern: waking up in the middle of the night and struggling to fall back asleep.
Understanding the Wake-Up
Firstly, why are we waking up during the night?
Waking up between 2 AM and 3 AM is said to be normal, and linked to your core body temperature. As your body core temperature drops, to trigger melatonin release, and then rises again, you get into a lighter stage of sleep. This lighter stage of sleep makes you more prone to waking up.
Note, there are also some medical conditions (such as sleep apnea) that can cause you to wake up during the night.
But, what can we do about it? Aside from constantly shifting sleeping position (Should I be sleeping on my back? On my left? Right?)
Avoid the Clock
The first step is to resist the urge to check the time. It’s easy to be tempted to have a look at the clock, however, doing so can increase anxiety, making it harder to fall back asleep. As Dr. Bruce says, sleep is like love—the less you chase it, the more it comes.
It may be useful to point your alarm clock (if you still have one of those) the opposite direction to your bed.
Embracing Non-Sleep Deep Rest (NSDR)
Whilst this may not help you fall back asleep, it’s worth pointing out that just lying quietly in the dark without moving still offers rejuvenation. This revujenating stage is called Non-Sleep Deep Rest (otherwise known as NSDR)
If you’re not familiar with NSDR, check out our overview of Andrew Huberman’s opinions on NSDR here.
So, you can reassure yourself that whilst you may not be asleep, you are still resting.
Keep Your Heart Rate Down
To fall back asleep, it’s best if your heart rate is below 60 bpm. So, Dr. Bruce advises avoiding void getting up unnecessarily, as moving around can elevate your heart rate.
On a similar vain, he introduces the 4-7-8 breathing technique, which is designed to lower your heart rate. The technique is simple:
- Breathe in for 4 seconds.
- Hold for 7 seconds.
- Exhale for 8 seconds.
Repeat this cycle gently to calm your body and mind.
As per any of our Video Breakdowns, we only try to capture the most important pieces of information in text; the rest can be garnered from the video itself:
Wishing you a thorough night’s rest!
Do you know any other good videos on sleep? Send them to us via email!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
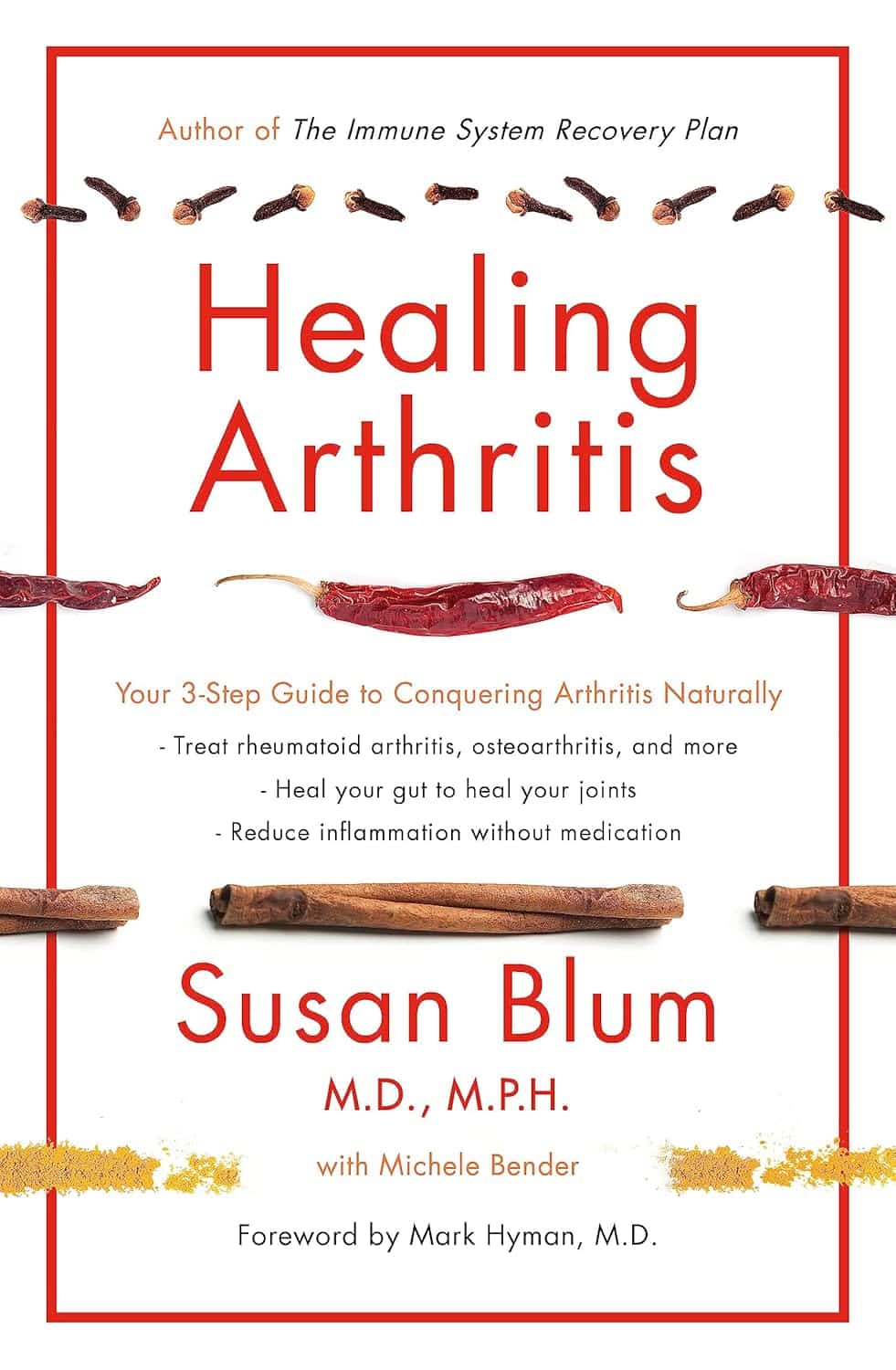
Healing Arthritis – by Dr. Susan Blum
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed another book by this author, her Immune System Recovery Plan, and today it’s more specific: healing arthritis
Of course, not all arthritis is rooted in immune dysfunction, but a) all of it is made worse by immune dysfunction and b) rheumatoid arthritis, which is an autoimmune disease, affects 1% of the population.
This book tackles all kinds of arthritis, by focusing on addressing the underlying causes and treating those, and (whether it was the cause or not) reducing inflammation without medication, because that will always help.
The “3 steps” mentioned in the subtitle are three stages of a plan to improve the gut microbiome in such a way that it not only stops worsening your arthritis, but starts making it better.
The style here is on the hard end of pop-science, so if you want something more conversational/personable, then this won’t be so much for you, but if you just want the information and explanation, then this does it just fine, and it has frequent references to the science to back it up, with a reassuringly extensive bibliography.
Bottom line: if you have arthritis and want a book that will help you to get either symptom-free or as close to that as is possible from your current condition (bearing in mind that arthritis is generally degenerative), then this is a great book for that.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: