Insomnia? High blood pressure? Try these!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Your Questions, Our Answers!
Q: Recipes for insomnia and high blood pressure and good foods to eat for these conditions?
A: Insomnia can be caused by many things, and consequently can often require a very multi-vector approach to fixing it. But, we’ll start by answering the question you asked (and probably address the rest of dealing with insomnia in another day’s edition!):
- First, you want food that’s easy to digest. Broadly speaking, this means plant-based. If not plant-based, fish (unless you have an allergy, obviously) is generally good and certainly better than white meat, which is better than red meat. In the category of dairy, it depends so much on what it is, that we’re not going to try to break it down here. If in doubt, skip it.
- You also don’t want blood sugar spikes, so it’s good to lay off the added sugar and white flour (or white flour derivatives, like white pasta), especially in your last meal of the day.
- Magnesium supports healthy sleep. A fine option would be our shchi recipe, but using collard greens rather than cabbage. Cabbage is a wonderful food, but collard greens are much higher in magnesium. Remember to add plenty of mushrooms (unless you don’t like them), as they’re typically high in magnesium too.
As for blood pressure, last month we gave tips (and a book recommendation) for heart health. The book, Dr. Monique Tello’s “Healthy Habits for Your Heart: 100 Simple, Effective Ways to Lower Your Blood Pressure and Maintain Your Heart’s Health”, also has recipes!
Here’s one from the “mains” section:
Secret Ingredient Baltimore-Style Salmon Patties with Not-Oily Aioli
❝This is a family favorite, and no one knows that it features puréed pumpkin! Most salmon cake recipes all for eggs and bread crumbs as binders, but puréed pumpkin and grated carrot work just as well, lend a beautiful color, and add plenty of fiber and plant nutrients. Canned salmon is way cheaper than fresh and has just as much omega-3 PUFAs and calcium. Serve this alongside a salad (the Summer Corn, Tomato, Spinach, and Basil Salad would go perfectly) for a well-rounded meal.❞
Serves 4 (1 large patty each)
Secret Ingredient Baltimore-Style Salmon Patties:
- 1 (15-oz) can pink salmon, no salt added
- ½ cup puréed pumpkin
- ½ cup grated carrot (I use a handheld box grater)
- 2 tablespoons minced chives (Don’t have chives? Minced green onions or any onions will do)
- 2 teaspoons Old Bay Seasoning
- 1 tablespoon olive oil
- ½ large lemon, sliced, for serving
Not-Oily Aioli:
- ½ cup plain low-fat Greek yogurt
- Juice and zest from ½ large lemon
- 1 clove garlic, crushed and minced fine
- 2 tablespoons chopped fresh dill
- For the patties: mix all the ingredients for the salmon patties together in a medium bowl
- Form patties with your hands and set on a plate or tray (you should have 4 burger-sized patties)
- Heat oil in a large skillet over medium heat.
- Set patties in a skillet and brown for 4 minutes, then carefully flip.
- Brown the other side, then serve hot.
- For the Aioli: mix all the ingredients for the aioli together in a small bowl.
- Plop a dollop alongside or on top of each salmon patty and serve with a spice of lemon.
Per serving: Calories: 367 | Fat: 13.6g | Saturated Fat: 4.4g | Protein: 46g | Sodium: 519mg | Carbohydrates: 13.2g | Fiber: 1.3g | Sugars: 9g | Calcium: 505mg | Iron: 1mg | Potassium 696mg
Notes from the 10almond team:
- If you want to make it plant-based, substitute cooked red lentils (no salt added) for the tinned salmon, and plant-based yogurt for the Greek yogurt
- We recommend adding more garlic. Seriously, who uses 1 clove of garlic for anything, let alone divided between four portions?
- The salads mentioned are given as recipes elsewhere in the same book. We strongly recommend getting her book, if you’re interested in heart health!
Do you have a question you’d like to see answered here? Hit reply or use the feedback widget at the bottom; we’d love to hear from you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Chicken or Fish – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chicken to fish, we picked the fish.
Why?
To understand the choice, we have to start a bit earlier on the decision tree. For most people most of the time, when it comes to a diet high in plants or high in animals, the plant-centric diet will generally be best:
Do We Need Animal Products To Be Healthy?
When it comes to animal meats, red meat is a fairly uncontroversial first thing to strike off the list:
…with pork and some other meats not being much better.
But chicken? Poultry in general appears to be quite health-neutral. The jury is out and the science has mixed results, but the data is leaning towards “it’s probably fine”.
See for example this huge (n=29,682) study:
this same paper shows that…
❝higher intake of processed meat, unprocessed red meat, or poultry, but not fish, was significantly associated with a small increased risk of incident CVD, whereas higher intake of processed meat or unprocessed red meat, but not poultry or fish, was significantly associated with a small increased risk of all-cause mortality❞
So, since poultry isn’t significantly increasing all-cause mortality, and fish isn’t significantly increasing all-cause mortality or cardiovascular disease, fish comes out as the hands-down (fins-down?) winner.
One more (this time, easy) choice to make, though!
While fish in general (please, not fried, though!) is generally considered quite healthy, there is a big difference (more than you might think, and for reasons that are quite alarming), between…
Health Risks & Nutrition: Farmed Fish vs Wild-Caught
Enjoy, and take care!
Share This Post
-
Why do I keep getting urinary tract infections? And why are chronic UTIs so hard to treat?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dealing with chronic urinary tract infections (UTIs) means facing more than the occasional discomfort. It’s like being on a never ending battlefield against an unseen adversary, making simple daily activities a trial.
UTIs happen when bacteria sneak into the urinary system, causing pain and frequent trips to the bathroom.
Chronic UTIs take this to the next level, coming back repeatedly or never fully going away despite treatment. Chronic UTIs are typically diagnosed when a person experiences two or more infections within six months or three or more within a year.
They can happen to anyone, but some are more prone due to their body’s makeup or habits. Women are more likely to get UTIs than men, due to their shorter urethra and hormonal changes during menopause that can decrease the protective lining of the urinary tract. Sexually active people are also at greater risk, as bacteria can be transferred around the area.
Up to 60% of women will have at least one UTI in their lifetime. While effective treatments exist, about 25% of women face recurrent infections within six months. Around 20–30% of UTIs don’t respond to standard antibiotic. The challenge of chronic UTIs lies in bacteria’s ability to shield themselves against treatments.
Why are chronic UTIs so hard to treat?
Once thought of as straightforward infections cured by antibiotics, we now know chronic UTIs are complex. The cunning nature of the bacteria responsible for the condition allows them to hide in bladder walls, out of antibiotics’ reach.
The bacteria form biofilms, a kind of protective barrier that makes them nearly impervious to standard antibiotic treatments.
This ability to evade treatment has led to a troubling increase in antibiotic resistance, a global health concern that renders some of the conventional treatments ineffective.
Some antibiotics no longer work against UTIs.
Michael Ebardt/ShutterstockAntibiotics need to be advanced to keep up with evolving bacteria, in a similar way to the flu vaccine, which is updated annually to combat the latest strains of the flu virus. If we used the same flu vaccine year after year, its effectiveness would wane, just as overused antibiotics lose their power against bacteria that have adapted.
But fighting bacteria that resist antibiotics is much tougher than updating the flu vaccine. Bacteria change in ways that are harder to predict, making it more challenging to create new, effective antibiotics. It’s like a never-ending game where the bacteria are always one step ahead.
Treating chronic UTIs still relies heavily on antibiotics, but doctors are getting crafty, changing up medications or prescribing low doses over a longer time to outwit the bacteria.
Doctors are also placing a greater emphasis on thorough diagnostics to accurately identify chronic UTIs from the outset. By asking detailed questions about the duration and frequency of symptoms, health-care providers can better distinguish between isolated UTI episodes and chronic conditions.
The approach to initial treatment can significantly influence the likelihood of a UTI becoming chronic. Early, targeted therapy, based on the specific bacteria causing the infection and its antibiotic sensitivity, may reduce the risk of recurrence.
For post-menopausal women, estrogen therapy has shown promise in reducing the risk of recurrent UTIs. After menopause, the decrease in estrogen levels can lead to changes in the urinary tract that makes it more susceptible to infections. This treatment restores the balance of the vaginal and urinary tract environments, making it less likely for UTIs to occur.
Lifestyle changes, such as drinking more water and practising good hygiene like washing hands with soap after going to the toilet and the recommended front-to-back wiping for women, also play a big role.
Some swear by cranberry juice or supplements, though researchers are still figuring out how effective these remedies truly are.
What treatments might we see in the future?
Scientists are currently working on new treatments for chronic UTIs. One promising avenue is the development of vaccines aimed at preventing UTIs altogether, much like flu shots prepare our immune system to fend off the flu.
Emerging treatments could help clear chronic UTIs.
guys_who_shoot/ShutterstockAnother new method being looked at is called phage therapy. It uses special viruses called bacteriophages that go after and kill only the bad bacteria causing UTIs, while leaving the good bacteria in our body alone. This way, it doesn’t make the bacteria resistant to treatment, which is a big plus.
Researchers are also exploring the potential of probiotics. Probiotics introduce beneficial bacteria into the urinary tract to out-compete harmful pathogens. These good bacteria work by occupying space and resources in the urinary tract, making it harder for harmful pathogens to establish themselves.
Probiotics can also produce substances that inhibit the growth of harmful bacteria and enhance the body’s immune response.
Chronic UTIs represent a stubborn challenge, but with a mix of current treatments and promising research, we’re getting closer to a day when chronic UTIs are a thing of the past.
Iris Lim, Assistant Professor, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
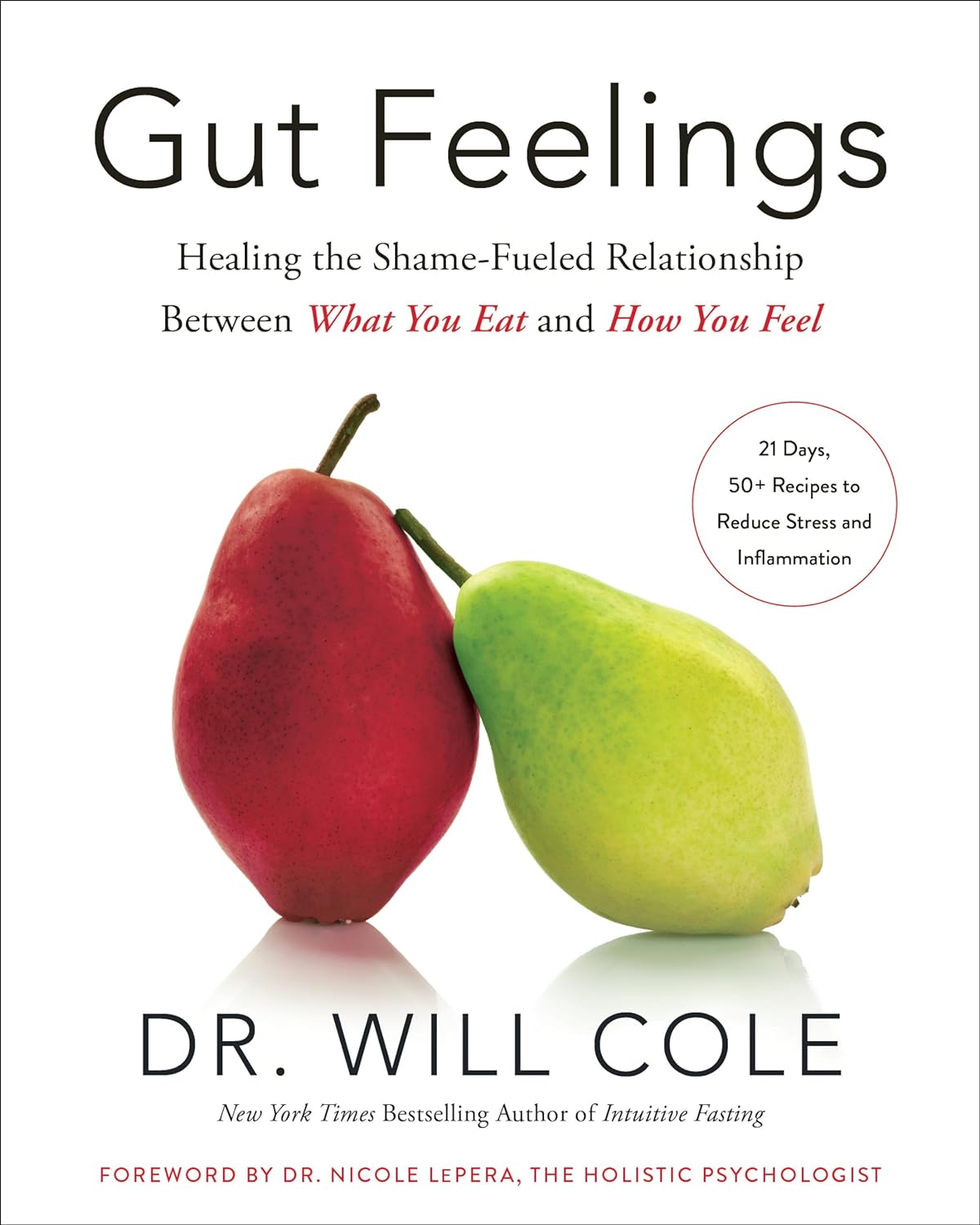
Gut Feelings – by Dr Will Cole
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More and more, science is uncovering links between our gut health and the rest of our health—including our mental health! We all know “get some fiber and consider probiotics”, but what else is there that we can do?
Quite a lot, actually. And part of it, which Dr. Cole also explores, is the fact that the gut-brain highway is a two-way street!
The book looks a lot especially at the particular relationship between shame and eating. The shame need not initially be about eating, though it can certainly end up that way too. But any kind of shame—be it relating to one’s body, work, relationship, or anything else, can not only have a direct effect on the gut, but indirect too:
Once our “eating our feelings” instinct kicks in, things can spiral from there, after all.
So, Dr. Cole walks us through tackling this from both sides—nutrition and psychology. With chapters full of tips and tricks, plus a 21-day plan (not a diet plan, a habit integration plan), this book hits shame (and inflammation, incidentally) hard and leads us into much healthier habits and cycles.
In short: if you’d like to have a better relationship with your food, improve your gut health, and/or reduce inflammation, this is definitely a book for you!
Share This Post
Related Posts
-
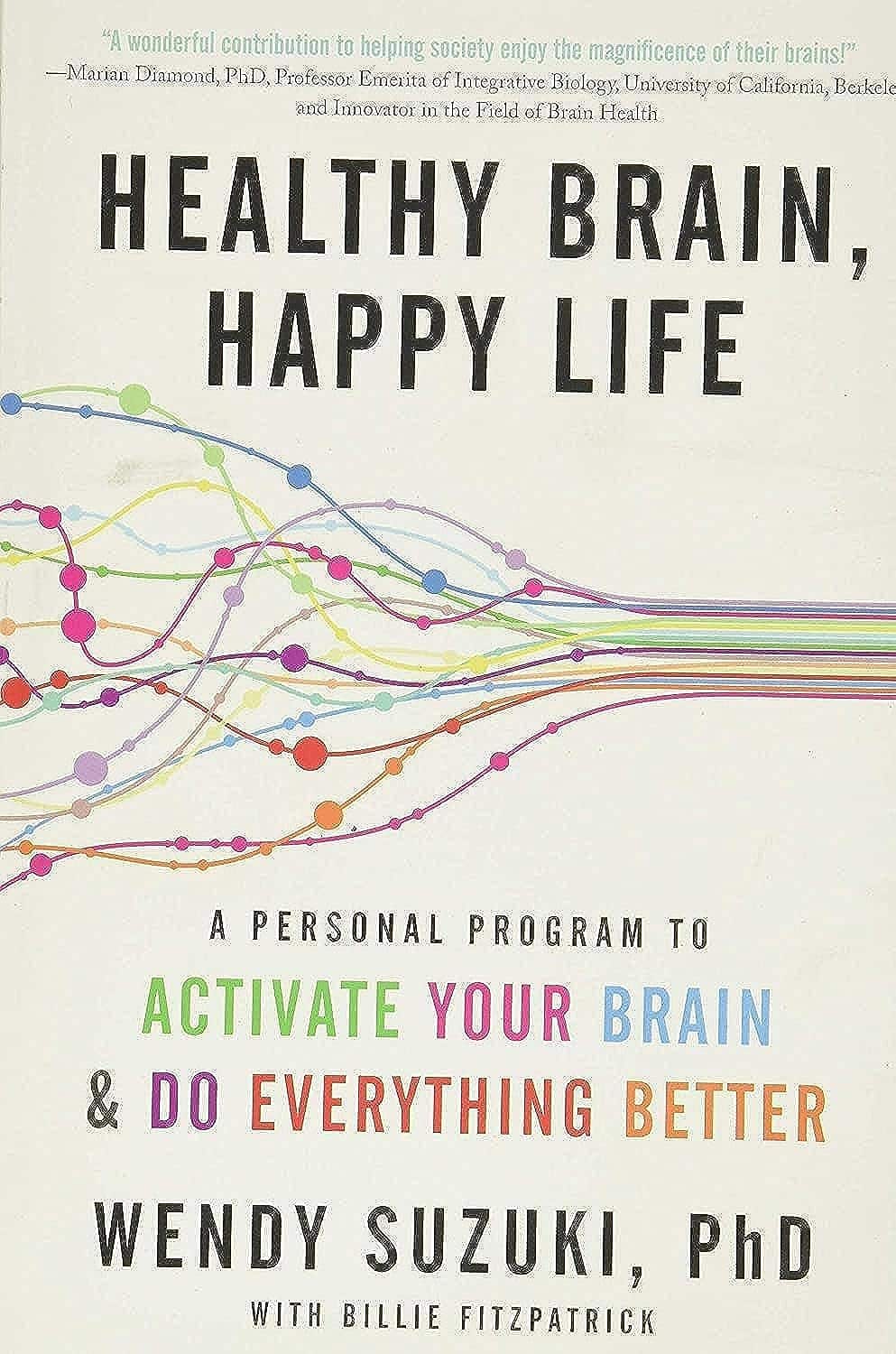
Healthy Brain, Happy Life – by Dr. Wendy Suzuki
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We talked about Dr. Wendy Suzuki’s research in the category of exercise and brain-benefits in our main feature the other day. But she has more to say than we can fit into an article!
This book chronicles her discoveries, through her work in memory and neuroplasticity, to her discoveries about exercise, and her dive into broader neurology-based mental health. So what does neurology-based mental health look like?
The answer is: mitigating brain-busters such as stress and anxiety, revitalizing a fatigued brain, boosting creativity, and other such benefits.
Does she argue that exercise is a cure-all? No, not quite. Sometimes there are other things she’s recommending (such as in her chapter on challenging the neurobiology of the stress response, or her chapter on meditation and the brain).
The writing style is mostly casual, interspersed with occasional mini-lectures (complete with diagrams and other illustrations), and is very readable and informative throughout.
Bottom line: if you’d like the more in-depth details of Dr. Suzuki’s work, this book is a very accessible way to get 320 pages of that!
Click here to check out Healthy Brain, Happy Life, and give yours the best!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Mediterranean Diet Cookbook for Beginners – by Jessica Aledo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are a lot of Mediterranean Diet books on the market, and not all of them actually stick to the Mediterranean Diet. There’s a common mistake of thinking “Well, this dish is from the Mediterranean region, so…”, but that doesn’t make, for example, bacon-laden carbonara part of the Mediterranean Diet!
Jessica Aledo does better, and sticks unwaveringly to the Mediterranean Diet principles.
First, she gives a broad introduction, covering:
- The Mediterranean Diet pyramid
- Foods to eat on the Mediterranean Diet
- Foods to avoid on the Mediterranean Diet
- Benefits of the Mediterranean Diet
Then, it’s straight into the recipes, of which there are 201 (as with many recipe books, the title is a little misleading about this).
They’re divided into sections, thus:
- Breakfasts
- Lunches
- Snacks
- Dinners
- Desserts
The recipes are clear and simple, one per double-page, with high quality color illustrations. They give ingredients/directions/nutrients. There’s no padding!
Helpfully, she does include a shopping list as an appendix, which is really useful!
Bottom line: if you’re looking to build your Mediterranean Diet repertoire, this book is an excellent choice.
Get your copy of The Mediterranean Diet Cookbook for Beginners from Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Grow In Comfort
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Grow (Without Leaving Your Comfort Zone)
“You have to get out of your comfort zone!” we are told, from cradle to grave.
When we are young, we are advised (or sometimes more forcefully instructed!) that we have to try new things. In our middle age, we are expected to be the world’s greatest go-getters, afraid of nothing and always pushing limits. And when we are old, people bid us “don’t be such a dinosaur”.
It is assumed, unquestioned, that growth can only occur through hardship and discomfort.
But what if that’s a discomforting lie?
Butler (2023) posited an idea: “We never achieve success faster and with less effort than when we are in our comfort zone”
Her words are an obvious callback to the ideas of Csikszentmihalyi (1970) in the sense of “flow”, in the sense in which that word is used in psychology.
Flow is: when a person is in a state of energized focus, full involvement, and enjoyment of an activity.
As a necessary truth (i.e: a function of syllogistic logic), the conditions of “in a state of flow” and “outside of one’s comfort zone” cannot overlap.
From there, we can further deduce (again by simple logic) that if flow can be found, and/but cannot be found outside of the comfort zone, then flow can only be found within the comfort zone.
That is indeed comforting, but what about growth?
Imagine you’ve never gone camping in your life, but you want to get outside of your comfort zone, and now’s the time to do it. So, you check out some maps of the Yukon, purchase some camping gear, and off you go into the wilderness. In the event that you survive to report it, you will indeed be able to say “it was not comfortable”.
But, did growth occur? Maybe, but… it’s a folly to say “what doesn’t kill us makes us stronger” as a reason to pursue such things. Firstly, there’s a high chance it may kill us. Secondly, what doesn’t kill us often leaves us incredibly weakened and vulnerable.
When Hannibal famously took his large army of mostly African mercenaries across the Alps during winter to march on Rome from the other side, he lost most of his men on the way, before proceeding to terrorize Northern Italy convincingly with the small remainder. But! Their hard experience hadn’t made them stronger; it had just removed the weaker soldiers, making the resultant formations harder to break.
All this to say, please do not inflict hardship and discomfort and danger in the hopes it’ll make you stronger; it will probably do the opposite.
But…
If, instead of wilderness trekking in the Yukon…
- You start off with a camper van holiday, then you’ll be taking a fair amount of your comfort with you. In effect, you will be stretching and expanding your comfort zone without leaving it.
- Then maybe another year you might try camping in a tent on a well-catered camping site.
- Later, you might try “roughing it” at a much less well-catered camping site.
- And so on.
Congratulations, you have tried new things and undergone growth, taking your comfort zone with you all the way!
This is more than just “easing yourself into” something
It really is about taking your comfort with you too. If you want to take up running, don’t ask “how can I run just a little bit first” or “how can I make it easier” (well, feel free to ask those things too, but) ask yourself: how can I bring my comfort with me? Comfortable shoes, perhaps, an ergonomic water bottle, shade for your head, maybe.
❝Any fool can rough it, but a good soldier can make himself comfortable in any circumstances❞
~ British Army maxim
This goes for more than just physical stuff, too
If you want to learn a new skill, the initial learning curve can be anxiety-inducing, especially if you are taking a course and worried about keeping up or “not being good enough”.
So, “secretly” study in advance, at your leisure, get yourself a head start. Find a degree of comfort in what you’ve learned so far, and then bring that comfort with you into your entry-level course that is now less intimidating.
Discomfort isn’t a badge of honor (and impedes growth)
Take that extra rest stop on the highway. Bring your favorite coffee with you. Use that walking stick, if it helps.
Whatever it takes to bring your comfort with you, bring it.
Trust us, you’ll get further that way.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: