How To Set Anxiety Aside
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Set Anxiety Aside
We’ve talked previously about how to use the “release” method to stop your racing mind.
That’s a powerful technique, but sometimes we need to be calm enough to use it. So first…
Breathe
Obviously. But, don’t underestimate the immediate power of focusing on your breath, even just for a moment.
There are many popular breathing exercises, but here’s one of the simplest and most effective, “4–4 breathing”:
- Breathe in for a count of four
- Hold for a count four
- Breathe out for a count of four
- Hold for a count of four
- Repeat
Depending on your lung capacity and what you’re used to, it may be that you need to count more quickly or slowly to make it feel right. Experiment with what feels comfortable for you, but the general goal should breathing deeply and slowly.
Identify the thing that’s causing you anxiety
We’ve also talked previously about how to use the RAIN technique to manage difficult emotions, and that’s good for handling anxiety too.
Another powerful tool is journaling.
Read: How To Use Journaling to Challenge Anxious Thoughts
If you don’t want to use any of those (very effective!) methods, that’s fine too—journaling isn’t for everyone.
You can leverage some of the same benefits by simply voicing your worries, even to yourself:
There’s an old folk tradition of “worry dolls”; these are tiny little dolls so small they can be kept in a pocket-size drawstring purse. Last thing at night, the user whispers their worries to the dolls and puts them back in their bag, where they will work on the person’s problem overnight.
We’re a health and productivity newsletter, not a dealer of magic and spells, but you can see how it works, right? It gets the worries out of one’s head, and brings about a helpful placebo effect too.
Focus on what you can control
- Most of what you worry about will not happen.
- Some of what you worry about may happen.
- Worrying about it will not help.
In fact, in some cases it may bring about what you fear, by means of the nocebo effect (like the placebo effect, but bad). Additionally, worrying drains your body and makes you less able to deal with whatever life does throw at you.
So while “don’t worry; be happy” may seem a flippant attitude, sometimes it can be best. However, don’t forget the other important part, which is actually focusing on what you can control.
- You can’t control whether your car will need expensive maintenance…
- …but you can control whether you budget for it.
- You can’t control whether your social event will go well or ill…
- …but you can control how you carry yourself.
- You can’t control whether your loved one’s health will get better or worse…
- …but you can control how you’re there for them, and you can help them take what sensible precautions they may.
…and so forth.
Look after your body as well!
Your body and mind are deeply reliant on each other. In this case, just as anxiety can drain your body’s resources, keeping your body well-nourished, well-exercised, and well-rested and can help fortify you against anxiety. For example, when it comes to diet, exercise, and sleep:
- Read: Fruit and vegetable intake is inversely associated with perceived stress across the adult lifespan
- Read: Exercise and anxiety: physical activity appears to be protective against anxiety disorders in clinical and non-clinical populations
- Read: Sleep problems predict and are predicted by generalized anxiety/depression
Don’t know where to start? How about the scientifically well-researched, evidence-based, 7-minute workout?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Can you die from long COVID? The answer is not so simple
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nearly five years into the pandemic, COVID is feeling less central to our daily lives.
But the virus, SARS-CoV-2, is still around, and for many people the effects of an infection can be long-lasting. When symptoms persist for more than three months after the initial COVID infection, this is generally referred to as long COVID.
In September, Grammy-winning Brazilian musician Sérgio Mendes died aged 83 after reportedly having long COVID.
Australian data show 196 deaths were due to the long-term effects of COVID from the beginning of the pandemic up to the end of July 2023.
In the United States, the Centers for Disease Control and Prevention reported 3,544 long-COVID-related deaths from the start of the pandemic up to the end of June 2022.
The symptoms of long COVID – such as fatigue, shortness of breath and “brain fog” – can be debilitating. But can you die from long COVID? The answer is not so simple.
Jan Krava/Shutterstock How could long COVID lead to death?
There’s still a lot we don’t understand about what causes long COVID. A popular theory is that “zombie” virus fragments may linger in the body and cause inflammation even after the virus has gone, resulting in long-term health problems. Recent research suggests a reservoir of SARS-CoV-2 proteins in the blood might explain why some people experience ongoing symptoms.
We know a serious COVID infection can damage multiple organs. For example, severe COVID can lead to permanent lung dysfunction, persistent heart inflammation, neurological damage and long-term kidney disease.
These issues can in some cases lead to death, either immediately or months or years down the track. But is death beyond the acute phase of infection from one of these causes the direct result of COVID, long COVID, or something else? Whether long COVID can directly cause death continues to be a topic of debate.
Of the 3,544 deaths related to long COVID in the US up to June 2022, the most commonly recorded underlying cause was COVID itself (67.5%). This could mean they died as a result of one of the long-term effects of a COVID infection, such as those mentioned above.
COVID infection was followed by heart disease (8.6%), cancer (2.9%), Alzheimer’s disease (2.7%), lung disease (2.5%), diabetes (2%) and stroke (1.8%). Adults aged 75–84 had the highest rate of death related to long COVID (28.8%).
These findings suggest many of these people died “with” long COVID, rather than from the condition. In other words, long COVID may not be a direct driver of death, but rather a contributor, likely exacerbating existing conditions.
The symptoms of long COVID can be debilitating. Lysenko Andrii/Shutterstock ‘Cause of death’ is difficult to define
Long COVID is a relatively recent phenomenon, so mortality data for people with this condition are limited.
However, we can draw some insights from the experiences of people with post-viral conditions that have been studied for longer, such as myalgic encephalomyelitis or chronic fatigue syndrome (ME/CFS).
Like long COVID, ME/CFS is a complex condition which can have significant and varied effects on a person’s physical fitness, nutritional status, social engagement, mental health and quality of life.
Some research indicates people with ME/CFS are at increased risk of dying from causes including heart conditions, infections and suicide, that may be triggered or compounded by the debilitating nature of the syndrome.
So what is the emerging data on long COVID telling us about the potential increased risk of death?
Research from 2023 has suggested adults in the US with long COVID were at greater risk of developing heart disease, stroke, lung disease and asthma.
Research has also found long COVID is associated with a higher risk of suicidal ideation (thinking about or planning suicide). This may reflect common symptoms and consequences of long COVID such as sleep problems, fatigue, chronic pain and emotional distress.
But long COVID is more likely to occur in people who have existing health conditions. This makes it challenging to accurately determine how much long COVID contributes to a person’s death.
Research has long revealed reliability issues in cause-of-death reporting, particularly for people with chronic illness.
Determining the exact cause of someone’s death is not always easy. Pixabay/Pexels So what can we conclude?
Ultimately, long COVID is a chronic condition that can significantly affect quality of life, mental wellbeing and overall health.
While long COVID is not usually immediately or directly life-threatening, it’s possible it could exacerbate existing conditions, and play a role in a person’s death in this way.
Importantly, many people with long COVID around the world lack access to appropriate support. We need to develop models of care for the optimal management of people with long COVID with a focus on multidisciplinary care.
Dr Natalie Jovanovski, Vice Chancellor’s Senior Research Fellow in the School of Health and Biomedical Sciences at RMIT University, contributed to this article.
Rose (Shiqi) Luo, Postdoctoral Research Fellow, School of Health and Biomedical Sciences, RMIT University; Catherine Itsiopoulos, Professor and Dean, School of Health and Biomedical Sciences, RMIT University; Kate Anderson, Vice Chancellor’s Senior Research Fellow, RMIT University; Magdalena Plebanski, Professor of Immunology, RMIT University, and Zhen Zheng, Associate Professor, STEM | Health and Biomedical Sciences, RMIT University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Q&A with the 10almonds Team
Q: Very interested in this article on CBD oil in the states. hope you do another one in the future with more studies done on people and more information on what’s new as far as CBD oil goes
A: We’re glad you enjoyed it! We’ll be sure to revisit CBD in the future—partly because it was a very popular article, and partly because, as noted, there is a lot going on there, research-wise!
And yes, we prefer human studies rather than mouse/rat studies where possible, too, and try to include those where we find them. In some cases, non-human animal studies allow us to know things that we can’t know from human studies… because a research institution’s ethics board will greenlight things for mice that it’d never* greenlight for humans.
Especially: things that for non-human animals are considered “introduction of external stressors” while the same things done to humans would be unequivocally called “torture”.
Animal testing in general is of course a moral quagmire, precisely because of the suffering it causes for animals, while the research results (hopefully) can be brought to bear to reduce to suffering of humans. We’re a health and productivity newsletter, not a philosophical publication, but all this to say: we’re mindful of such too.
And yes, we agree, when studies are available on humans, they’re always going to be better than the same study done on mice and rats.
As a topical aside, did you know there’s a monument to laboratory mice and all they’ve (however unintentionally) done for us?
❝The quirky statue depicts an anthropomorphic mouse as an elderly woman, complete with glasses balanced atop its nose. Emerging from two knitting needles in its hands is the recognizable double-helix of a strand of DNA.❞
~ Smithsonian Magazine
Share This Post
-
Women and Minorities Bear the Brunt of Medical Misdiagnosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Charity Watkins sensed something was deeply wrong when she experienced exhaustion after her daughter was born.
At times, Watkins, then 30, had to stop on the stairway to catch her breath. Her obstetrician said postpartum depression likely caused the weakness and fatigue. When Watkins, who is Black, complained of a cough, her doctor blamed the flu.
About eight weeks after delivery, Watkins thought she was having a heart attack, and her husband took her to the emergency room. After a 5½-hour wait in a North Carolina hospital, she returned home to nurse her baby without seeing a doctor.
When a physician finally examined Watkins three days later, he immediately noticed her legs and stomach were swollen, a sign that her body was retaining fluid. After a chest X-ray, the doctor diagnosed her with heart failure, a serious condition in which the heart becomes too weak to adequately pump oxygen-rich blood to organs throughout the body. Watkins spent two weeks in intensive care.
She said a cardiologist later told her, “We almost lost you.”
Watkins is among 12 million adults misdiagnosed every year in the U.S.
In a study published Jan. 8 in JAMA Internal Medicine, researchers found that nearly 1 in 4 hospital patients who died or were transferred to intensive care had experienced a diagnostic error. Nearly 18% of misdiagnosed patients were harmed or died.
In all, an estimated 795,000 patients a year die or are permanently disabled because of misdiagnosis, according to a study published in July in the BMJ Quality & Safety periodical.
Some patients are at higher risk than others.
Women and racial and ethnic minorities are 20% to 30% more likely than white men to experience a misdiagnosis, said David Newman-Toker, a professor of neurology at Johns Hopkins School of Medicine and the lead author of the BMJ study. “That’s significant and inexcusable,” he said.
Researchers call misdiagnosis an urgent public health problem. The study found that rates of misdiagnosis range from 1.5% of heart attacks to 17.5% of strokes and 22.5% of lung cancers.
Weakening of the heart muscle — which led to Watkins’ heart failure — is the most common cause of maternal death one week to one year after delivery, and is more common among Black women.
Heart failure “should have been No. 1 on the list of possible causes” for Watkins’ symptoms, said Ronald Wyatt, chief science and chief medical officer at the Society to Improve Diagnosis in Medicine, a nonprofit research and advocacy group.
Maternal mortality for Black mothers has increased dramatically in recent years. The United States has the highest maternal mortality rate among developed countries. According to the Centers for Disease Control and Prevention, non-Hispanic Black mothers are 2.6 times as likely to die as non-Hispanic white moms. More than half of these deaths take place within a year after delivery.
Research shows that Black women with childbirth-related heart failure are typically diagnosed later than white women, said Jennifer Lewey, co-director of the pregnancy and heart disease program at Penn Medicine. That can allow patients to further deteriorate, making Black women less likely to fully recover and more likely to suffer from weakened hearts for the rest of their lives.
Watkins said the diagnosis changed her life. Doctors advised her “not to have another baby, or I might need a heart transplant,” she said. Being deprived of the chance to have another child, she said, “was devastating.”
Racial and gender disparities are widespread.
Women and minority patients suffering from heart attacks are more likely than others to be discharged without diagnosis or treatment.
Black people with depression are more likely than others to be misdiagnosed with schizophrenia.
Minorities are less likely than whites to be diagnosed early with dementia, depriving them of the opportunities to receive treatments that work best in the early stages of the disease.
Misdiagnosis isn’t new. Doctors have used autopsy studies to estimate the percentage of patients who died with undiagnosed diseases for more than a century. Although those studies show some improvement over time, life-threatening mistakes remain all too common, despite an array of sophisticated diagnostic tools, said Hardeep Singh, a professor at Baylor College of Medicine who studies ways to improve diagnosis.
“The vast majority of diagnoses can be made by getting to know the patient’s story really well, asking follow-up questions, examining the patient, and ordering basic tests,” said Singh, who is also a researcher at Houston’s Michael E. DeBakey VA Medical Center. When talking to people who’ve been misdiagnosed, “one of the things we hear over and over is, ‘The doctor didn’t listen to me.’”
Racial disparities in misdiagnosis are sometimes explained by noting that minority patients are less likely to be insured than white patients and often lack access to high-quality hospitals. But the picture is more complicated, said Monika Goyal, an emergency physician at Children’s National Hospital in Washington, D.C., who has documented racial bias in children’s health care.
In a 2020 study, Goyal and her colleagues found that Black kids with appendicitis were less likely than their white peers to be correctly diagnosed, even when both groups of patients visited the same hospital.
Although few doctors deliberately discriminate against women or minorities, Goyal said, many are biased without realizing it.
“Racial bias is baked into our culture,” Goyal said. “It’s important for all of us to start recognizing that.”
Demanding schedules, which prevent doctors from spending as much time with patients as they’d like, can contribute to diagnostic errors, said Karen Lutfey Spencer, a professor of health and behavioral sciences at the University of Colorado-Denver. “Doctors are more likely to make biased decisions when they are busy and overworked,” Spencer said. “There are some really smart, well-intentioned providers who are getting chewed up in a system that’s very unforgiving.”
Doctors make better treatment decisions when they’re more confident of a diagnosis, Spencer said.
In an experiment, researchers asked doctors to view videos of actors pretending to be patients with heart disease or depression, make a diagnosis, and recommend follow-up actions. Doctors felt far more certain diagnosing white men than Black patients or younger women.
“If they were less certain, they were less likely to take action, such as ordering tests,” Spencer said. “If they were less certain, they might just wait to prescribe treatment.”
It’s easy to see why doctors are more confident when diagnosing white men, Spencer said. For more than a century, medical textbooks have illustrated diseases with stereotypical images of white men. Only 4.5% of images in general medical textbooks feature patients with dark skin.
That may help explain why patients with darker complexions are less likely to receive a timely diagnosis with conditions that affect the skin, from cancer to Lyme disease, which causes a red or pink rash in the earliest stage of infection. Black patients with Lyme disease are more likely to be diagnosed with more advanced disease, which can cause arthritis and damage the heart. Black people with melanoma are about three times as likely as whites to die within five years.
The covid-19 pandemic helped raise awareness that pulse oximeters — the fingertip devices used to measure a patient’s pulse and oxygen levels — are less accurate for people with dark skin. The devices work by shining light through the skin; their failures have delayed critical care for many Black patients.
Seven years after her misdiagnosis, Watkins is an assistant professor of social work at North Carolina Central University in Durham, where she studies the psychosocial effects experienced by Black mothers who survive severe childbirth complications.
“Sharing my story is part of my healing,” said Watkins, who speaks to medical groups to help doctors improve their care. “It has helped me reclaim power in my life, just to be able to help others.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
Common Sense Labs: Blood Labs Demystified – by Dr. Ken Berry & Kim Howerton
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most people, if given their test results as a set of numbers, will have no idea what they mean.
And a doctor or nurse saying “this is good”, “this is a bit low”, “this is very high” etc isn’t that much more informative, as it doesn’t really give a true feel for the information.
Dr. Berry produced this book to bridge that knowledge gap, and in his words, “put the power of health back in the hands of the people”. The book also covers what blood tests to recommend annually (finding common recommendations insufficient), and how to go about asking for those if your doctor might be keen to brush you off.
This is a short book (weighing in at a lithe 78 pages), but the information contained therein is very dense, and very convenient to have it all in one place.
As one Amazon reviewer wrote,
❝Someone said you can find the information on the Internet, but I would say good luck with that. It will be many many many hours compiling the gold that is in this book.❞
Writer’s anecdote: indeed, I recently had 14 blood tests done as part of a regular checkup (I’m pleased to report I could not be in better health), and while interpreting the results, I had to look up a lot of things (which were often in the wrong units*), and if I’d had this book already, it would have been a breeze, as it covers everything I had done!
*On which note, this book does provide results in US and International units, so you won’t be left wondering how to convert mmol/mol into mmol/L or mg/dL or such.
Bottom line: if you are a person who has blood, this book will at some point be of immense value to you, if not immediately!
Click here to check out Common Sense Labs, and understand what your blood is saying!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
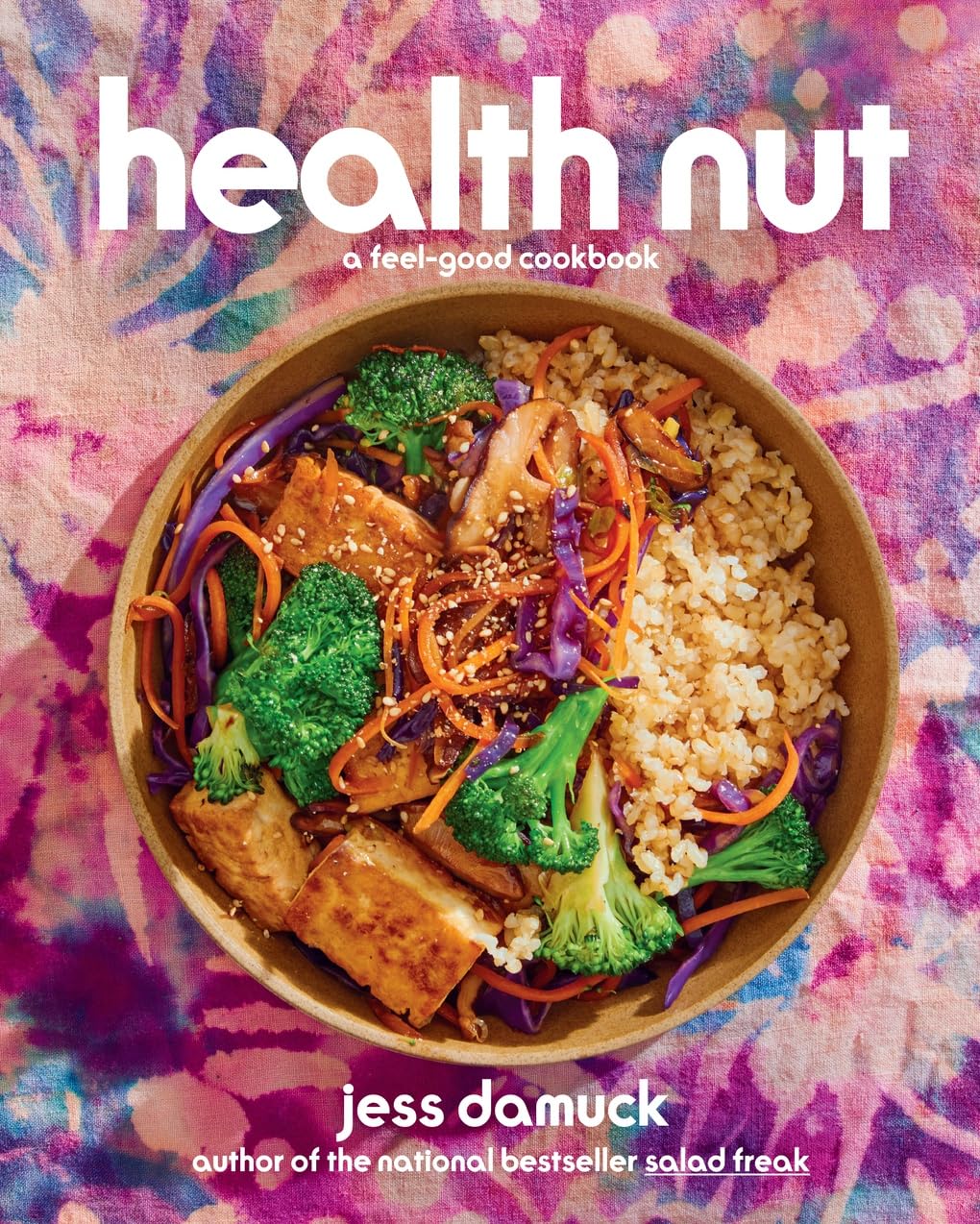
Health Nut: A Feel-Good Cookbook – by Jess Damuck
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author is a classically trained chef (worked with Martha Stewart for a long time!), and while health is the focus here, it’s not the be-all-and-end-all, so there’s a lot of attention given to pleasure also. Which, after all, is not a zero-sum game—we can have both!
So, the title and subtitle together sum up the ethos of the book pretty well.
The recipes themselves are divided into categories by meal-type, snacks, desserts, etc. They’re varied enough to suit most moods and seasons, as well as being equally appropriate for cooking for one, or a family, or entertaining. Many (but not all) of the recipes are vegan, though where they’re not, the substitutions are mostly easy and obvious, or explained, or else alternative recipes are given (for example a vegan “tuna” recipe).
In terms of complexity, these are not very complex, yet include everything they need to to make things interesting. That said, the ingredients are also not obscure, and should be easy to find in any reasonably well-stocked supermarket.
One small downside is that many of the recipes are not illustrated, but the instructions are clear enough that this isn’t really a problem, in this reviewer’s opinion.
Bottom line: if you’d like to broaden your kitchen repertoire with plants-forward cooking from an accomplished chef, then this is a good book for that.
Click here to check out Health Nut, and enjoy the feel-good food!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Grapefruit vs Lemon – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing grapefruit to lemon, we picked the lemon.
Why?
Grapefruit has its merits, but in the battle of the citrus fruits, lemons come out on top nutritionally:
In terms of macros, grapefruit has more carbs while lemons have more fiber. So, while both have a low glycemic index, lemon is still the winner by the numbers.
Looking at the vitamins, here we say grapefruit’s strengths: grapefruit has more of vitamins A, B2, B3, and choline, while lemon has more of vitamins B6 and C. So, a 4:2 win for grapefruit here.
In the category of minerals, lemons retake the lead: grapefruit has more zinc, while lemon has more calcium, copper, iron, manganese, and selenium.
One final consideration that’s not shown in the nutritional values, is that grapefruit contains high levels of furanocoumarin, which can inhibit cytochrome P-450 3A4 isoenzyme and P-glycoptrotein transporters in the intestine and liver—slowing down their drug metabolism capabilities, thus effectively increasing the bioavailability of many drugs manifold.
This may sound superficially like a good thing (improving bioavailability of things we want), but in practice it means that in the case of many drugs, if you take them with (or near in time to) grapefruit or grapefruit juice, then congratulations, you just took an overdose. This happens with a lot of meds for blood pressure, cholesterol (including statins), calcium channel-blockers, anti-depressants, benzo-family drugs, beta-blockers, and more. Oh, and Viagra, too. Which latter might sound funny, but remember, Viagra’s mechanism of action is blood pressure modulation, and that is not something you want to mess around with unduly. So, do check with your pharmacist to know if you’re on any meds that would be affected by grapefruit or grapefruit juice!
PS: the same substance is quite available in pummelos and sour oranges (but not meaningfully in sweet oranges); you can see a chart here showing the relative furanocoumarin contents of many citrus fruits, or lack thereof as the case may be, as it is for lemons and most limes)
Adding up the sections gives us a clear win for lemons, but by all means enjoy either or both; just watch out for that furanocoumarin content of grapefruit if you’re on any meds affected by such (again, do check with your pharmacist, as our list was far from exhaustive—and yes, this question is one that a pharmacist will answer more easily and accurately than a doctor will).
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← citrus fruits in general make the list; they inhibit tumor growth and kill cancer cells; regular consumption is also associated with a lower cancer risk 🙂
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: