The Mental Health First-Aid That You’ll Hopefully Never Need
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Take Your Mental Health As Seriously As General Health!
Sometimes, health and productivity means excelling—sometimes, it means avoiding illness and unproductivity. Both are essential, and today we’re going to tackle some ground-up stuff. If you don’t need it right now, great; we suggest to read it for when and if you do. But how likely is it that you will?
- One in four of us are affected by serious mental health issues in any given year.
- One in five of us have suicidal thoughts at some point in our lifetime.
- One in six of us are affected to at least some extent by the most commonly-reported mental health issues, anxiety and depression, in any given week.
…and that’s just what’s reported, of course. These stats are from a UK-based source but can be considered indicative generally. Jokes aside, the UK is not a special case and is not measurably worse for people’s mental health than, say, the US or Canada.
While this is not an inherently cheery topic, we think it’s an important one.
Depression, which we’re going to focus on today, is very very much a killer to both health and productivity, after all.
One of the most commonly-used measures of depression is known by the snappy name of “PHQ9”. It stands for “Patient Health Questionnaire Nine”, and you can take it anonymously online for free (without signing up for anything; it’s right there on the page already):
Take The PHQ9 Test Here! (under 2 minutes, immediate results)
There’s a chance you took that test and your score was, well, depressing. There’s also a chance you’re doing just peachy, or maybe somewhere in between. PHQ9 scores can fluctuate over time (because they focus on the past two weeks, and also rely on self-reports in the moment), so you might want to bookmark it to test again periodically. It can be interesting to track over time.
In the event that you’re struggling (or: in case one day you find yourself struggling, or want to be able to support a loved one who is struggling), some top tips that are useful:
Accept that it’s a medical condition like any other
Which means some important things:
- You/they are not lazy or otherwise being a bad person by being depressed
- You/they will probably get better at some point, especially if help is available
- You/they cannot, however, “just snap out of it”; illness doesn’t work that way
- Medication might help (it also might not)
Do what you can, how you can, when you can
Everyone knows the advice to exercise as a remedy for depression, and indeed, exercise helps many. Unfortunately, it’s not always that easy.
Did you ever see the 80s kids’ movie “The Neverending Story”? There’s a scene in which the young hero Atreyu must traverse the “Swamp of Sadness”, and while he has a magical talisman that protects him, his beloved horse Artax is not so lucky; he slows down, and eventually stops still, sinking slowly into the swamp. Atreyu pulls at him and begs him to keep going, but—despite being many times bigger and stronger than Atreyu, the horse just sinks into the swamp, literally drowning in despair.
See the scene: The Neverending Story movie clip – Artax and the Swamp of Sadness (1984)
Wow, they really don’t make kids’ movies like they used to, do they?
But, depression is very much like that, and advice “exercise to feel less depressed!” falls short of actually being helpful, when one is too depressed to do it.
If you’re in the position of supporting someone who’s depressed, the best tool in your toolbox will be not “here’s why you should do this” (they don’t care; not because they’re an uncaring person by nature, but because they are physiologically impeded from caring about themself at this time), but rather:
“please do this with me”
The reason this has a better chance of working is because the depressed person will in all likelihood be unable to care enough to raise and/or maintain an objection, and while they can’t remember why they should care about themself, they’re more likely to remember that they should care about you, and so will go with your want/need more easily than with their own. It’s not a magic bullet, but it’s worth a shot.
What if I’m the depressed person, though?
Honestly, the same, if there’s someone around you that you do care about; do what you can to look after you, for them, if that means you can find some extra motivation.
But I’m all alone… what now?
Firstly, you don’t have to be alone. There are free services that you can access, for example:
- US: https://nami.org/help
- Canada: https://www.wellnesstogether.ca/en-CA
- UK: https://www.samaritans.org/
…which varyingly offer advice, free phone services, webchats, and the like.
But also, there are ways you can look after yourself a little bit; do the things you’d advise someone else to do, even if you’re sure they won’t work:
- Take a little walk around the block
- Put the lights on when you’re not sleeping
- For that matter, get out of bed when you’re not sleeping. Literally lie on the floor if necessary, but change your location.
- Change your bedding, or at least your clothes
- If changing the bedding is too much, change just the pillowcase
- If changing your clothes is too much, change just one item of clothing
- Drink some water; it won’t magically cure you, but you’ll be in slightly better order
- On the topic of water, splash some on your face, if showering/bathing is too much right now
- Do something creative (that’s not self-harm). You may scoff at the notion of “art therapy” helping, but this is a way to get at least some of the lights on in areas of your brain that are a little dark right now. Worst case scenario is it’ll be a distraction from your problems, so give it a try.
- Find a connection to community—whatever that means to you—even if you don’t feel you can join it right now. Discover that there are people out there who would welcome you if you were able to go join them. Maybe one day you will!
- Hiding from the world? That’s probably not healthy, but while you’re hiding, take the time to read those books (write those books, if you’re so inclined), learn that new language, take up chess, take up baking, whatever. If you can find something that means anything to you, go with that for now, ride that wave. Motivation’s hard to come by during depression and you might let many things slide; you might as well get something out of this period if you can.
If you’re not depressed right now but you know you’re predisposed to such / can slip that way?
Write yourself instructions now. Copy the above list if you like.
Most of all: have a “things to do when I don’t feel like doing anything” list.
If you only take one piece of advice from today’s newsletter, let that one be it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Beat Food Addictions!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When It’s More Than “Just” Cravings
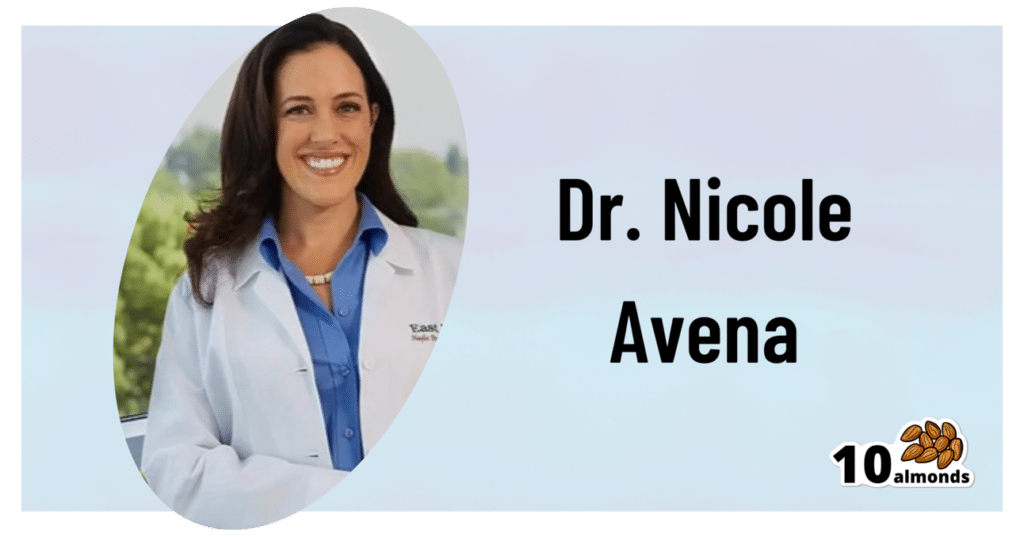
This is Dr. Nicole Avena. She’s a research neuroscientist who also teaches at Mount Sinai School of Medicine, as well as at Princeton. She’s done a lot of groundbreaking research in the field of nutrition, diet, and addition, with a special focus on women’s health and sugar intake specifically.
What does she want us to know?
Firstly, that food addictions are real addictions.
We know it can sound silly, like the famous line from Mad Max:
❝Do not, my friends, become addicted to water. It will take hold of you and you will resent its absence!❞
As an aside, it is actually possible to become addicted to water; if one drinks it excessively (we are talking gallons every day) it does change the structure of the brain (no surprise; the brain is not supposed to have that much water!) causing structural damage that then results in dependency, and headaches upon withdrawal. It’s called psychogenic polydipsia:
But back onto today’s more specific topic, and by a different mechanism of addiction…
Food addictions are dopaminergic addictions (as is cocaine)
If you are addicted to a certain food (often sugar, but other refined carbs such as potato products, and also especially refined flour products, are also potential addictive substances), then when you think about the food in question, your brain lights up with more dopamine than it should, and you are strongly motivated to seek and consume the substance in question.
Remember, dopamine functions by expectation, not by result. So until your brain’s dopamine-gremlin is sated, it will keep flooding you with motivational dopamine; that’s why the first bite tastes best, then you wolf down the rest before your brain can change its mind, and afterwards you may be left thinking/feeling “was that worth it?”.
Much like with other addictions (especially alcohol), shame and regret often feature strongly afterwards, even accompanied by notions of “never again”.
But, binge-eating is as difficult to escape as binge-drinking.
You can break free, but you will probably have to take it seriously
Dr. Avena recommends treating a food addiction like any other addiction, which means:
- Know why you want to quit (make a list of the reasons, and this will help you stay on track later!)
- Make a conscious decision to genuinely quit
- Learn about the nature of the specific addiction (know thy enemy!)
- Choose a strategy (e.g. wean off vs cold turkey, and decide what replacements, if any, you will use)
- Get support (especially from those around you, and/but the support of others facing, or who have successfully faced, the same challenge is very helpful too)
- Keep track of your success (build and maintain a streak!)
- Lean into how you will better enjoy life without addiction to the substance (it never really made you happy anyway, so enjoy your newfound freedom and good health!)
Want more from Dr. Avena?
You can check out her column at Psychology Today here:
Psychology Today | Food Junkie ← it has a lot of posts about sugar addiction in particular, and gives a lot of information and practical advice
You can also read her book, which could be a great help if you are thinking of quitting a sugar addiction:
Sugarless: A 7-Step Plan to Uncover Hidden Sugars, Curb Your Cravings, and Conquer Your Addiction
Enjoy!
Share This Post
-
High Histamine Foods To Avoid (And Low Histamine Foods To Eat Instead)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nour Zibdeh is an Integrative and Functional Dietician, and she helps people overcome food intolerances. Today, it’s about getting rid of the underdiagnosed condition that is histamine intolerance, by first eliminating the triggers, and then not getting stuck on the low-histamine diet
The recommendations
High histamine foods to avoid include:
- Alcohol (all types)
- Fermented foods—normally great for the gut, but bad in this case
- That includes most cheeses and yogurts
- Aged, cured, or otherwise preserved meat
- Some plants, e.g. tomato, spinach, eggplant, banana, avocado. Again, normally all great, but not in this case.
Low histamine foods to eat include:
- Fruits and vegetables not mentioned above
- Minimally processed meat and fish, either fresh from the butcher/fishmonger, or frozen (not from the chilled food section of the supermarket), and eaten the same day they were purchased or defrosted, because otherwise histamine builds up over time (and quite quickly)
- Grains, but she recommends skipping gluten, given the high likelihood of a comorbid gluten intolerance. So instead she recommends for example quinoa, oats, rice, buckwheat, millet, etc.
For more about these (and more examples), as well as how to then phase safely off the low histamine diet, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
Food intolerances often gang up on a person (i.e., comorbidity is high), so you might also like to read about:
- Gluten: What’s The Truth?
- Fiber For FODMAP-Avoiders
- Foods For Managing Hypothyroidism (incl. Hashimoto’s)
- Crohn’s, Food Intolerances, & More
Take care!
Share This Post
-
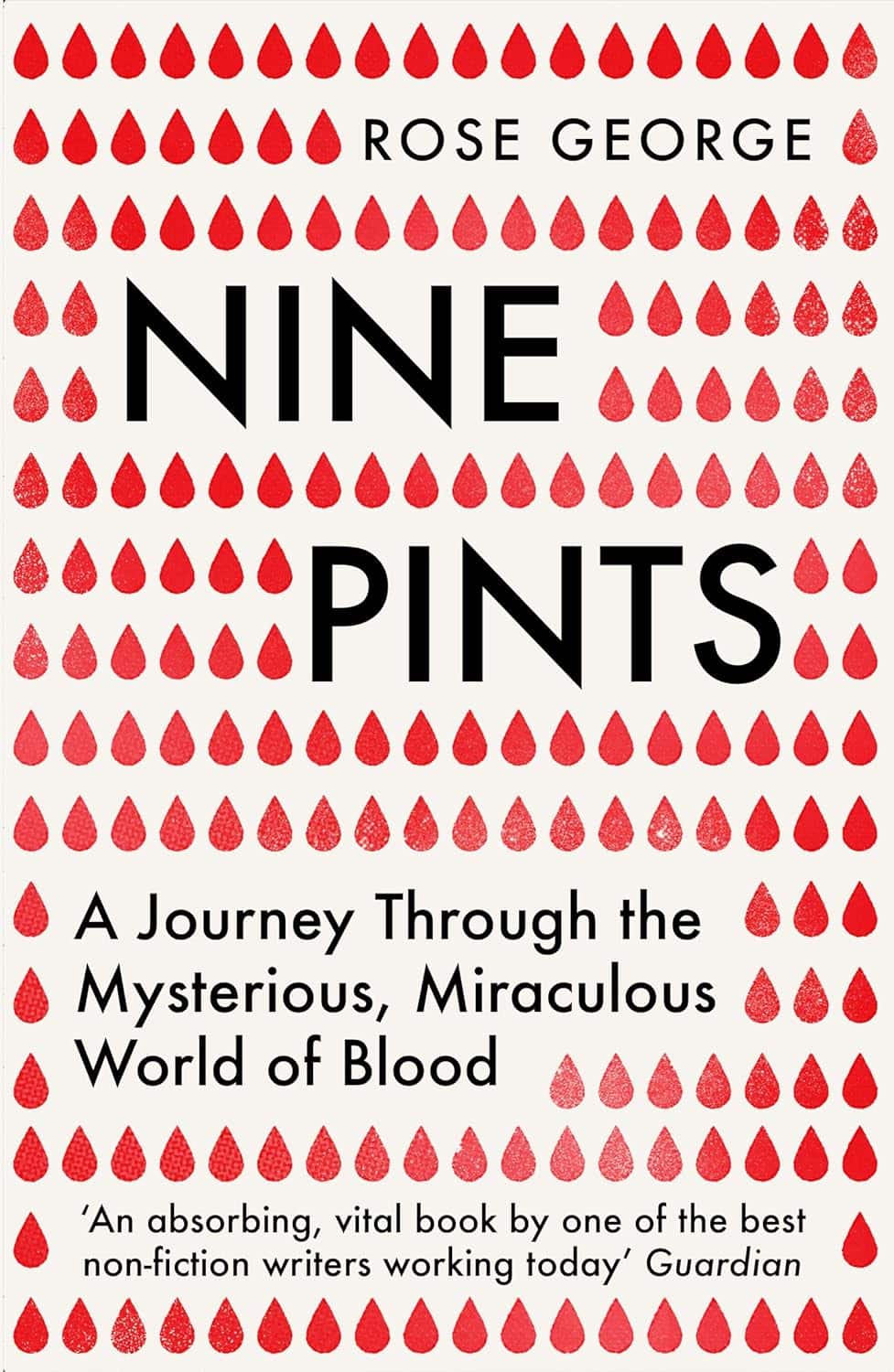
Nine Pints – by Rose George
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Rose George is not a scientist, but an investigative journalist. As such, she’s a leave-no-stone-unturned researcher, and that shows here.
The style throughout is, as one might expect, journalistic. But, she’s unafraid of diving into the science of it, interviewing many medical professionals as part of her work. She also looks to people living with various blood-related conditions, ranging from hemophilia to HIV.
Speakling of highly-stigmatized yet very manageable conditions, there’s also a fair section devoted to menstruation, menstrual blood, and societies’ responses to such, from shunning to active support.
We also learn about the industrialization of blood—from blood banks to plasma labs to leech farms. You probably knew leeches are still used as a medical tool in even the most high-tech of hospitals, but you’ll doubtlessly learn a fascinating thing or two from the “insider views” along the way.
Bottom line: if you’d like to know more about the red stuff in all its marvelous aspects, with neither sensationalization nor sanitization (the topic needs neither!), this is the book for you.
Click here to check out Nine Pints, and learn more about yours!
Share This Post
Related Posts
-
Chocolate & Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chocolate & Health: Fact or Fiction?
“Chocolate Is Good For The Heart”
“When making chocolate chip cookies, you don’t measure using cups, you measure by heart”
…but how good is chocolate when it comes to heart health?
First, what is heart health?
A healthy heart typically has a low resting pulse rate and a strong, steady beat. This is affected strongly by exercise habits, and diet plays only a support role (can’t exercise without energy from food!).
It is also important to have blood pressure within a healthy range (with high blood pressure being a more common problem than low, so things that lower blood pressure are generally considered good).
- Flavanols, flavonoids, and polyphenols in chocolate contribute to lower blood pressure
- Dark chocolate is best for these, as milk chocolate contains much less cocoa solids and more unhelpful fats
- White chocolate contains no cocoa solids and is useless for this
- Some of the fats in most commercial chocolate can contribute to atherosclerosis which raises blood pressure and ultimately can cause heart attacks.
- If you’re diabetic, you will probably not get the usual heart-related benefits from chocolate (sorry)
The Verdict: dark chocolate, in moderation, can support good heart health.
“Chocolate Is Good For The Brain”
Chocolate has been considered a “brain food”… why?
- The brain uses more calories than any other organ (chocolate has many calories)
- The heart benefits we listed above mean improved blood flow—including to your brain
- Chocolate contains phenylethylamine, a powerful chemical that has a similar effect to amphetamines… But it’s metabolized in digestion and never makes it to the central nervous system (so basically, this one’s a miss; we had a good run with the other two, though!)
The Verdict: dark chocolate, in moderation, can support good brain health
“Chocolate Is An Aphrodisiac”
“If chocolate be the food of love, pass me that cocoa; I’m starving”
Most excitingly, chocolate contains phenylethylamine, the “molecule of love” or, more accurately, lust. It has an effect similar to amphetamines, and while we can synthesize it in the body, we can also get it from certain foods. But…
Our body is so keen to get it that most of it is metabolized directly during digestion and doesn’t make it to the brain. Also, chocolate is not as good a source as cabbage—do with that information what you will!
However!
Chocolate contains theobromine and small amounts of caffeine, both stimulants and both generally likely to improve mood; it also contains flavonoids which in turn stimulate production of nitric oxide, which is a relaxant. All in all, things that are convivial to having a good time.
On the other hand…
That relaxation comes specifically with a reduction in blood pressure—something typically considered good for the health for most people most of the time… but that means lowering blood pressure in all parts of your body, which could be the opposite of what you want in intimate moments.
Chocolate also contains zinc, which is essential for hormonal health for most people—the body uses it to produce testosterone and estrogen, respectively. Zinc supplements are popularly sold to those wishing to have more energy in general and good hormonal health in particular, and rightly so. However…
This approach requires long-term supplementation—you can’t just pop a zinc tablet / bar of chocolate / almond before bed and expect immediate results. And if your daily zinc supplementation takes the form of a 3.5oz (100g) bar of chocolate, then you may find it has more effects on your health, and not all of them good!
The Verdict: dark chocolate, in moderation, may promote “the mood”, but could be a double-edged sword when it comes to “the ability”.
“Chocolate Is Good During Menstruation”
The popular wisdom goes that chocolate is rich in iron (of which more is needed during menstruation), and indeed, if you eat 7oz (150g) of dark chocolate made with 85% cocoa, you’ll get a daily a dose of iron (…and nearly 1,000 calories).
More bang-for-buck dietary sources of iron include chickpeas and broccoli, but for some mysterious reason, these are not as commonly reported as popular cravings.
The real explanation for chocolate cravings is more likely that eating chocolate—a food high in sugar and fat along with a chemical bombardment of more specialized “hey, it’s OK, you can relax now” molecules (flavanols/flavonoids, polyphenols, phenylamines, even phenylethylamine, etc) gives a simultaneous dopamine kick (the body’s main “reward” chemical) with a whole-body physiological relaxation… so, little wonder we might crave it in times of stress and discomfort!
The Verdict: it helps, not because it serves a special nutritional purpose, but rather, because the experience of eating chocolate makes us feel good.
Fun fact: Tiramisu (this writer’s favorite dessert) is literally Italian for “pick-me-up”
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Most Annoying Nutrition Tips (7 Things That Actually Work)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You can’t out-exercise a bad diet, and getting a good diet can be a challenge depending on your starting point. Here’s Cori Lefkowith’s unglamorous seven-point plan:
Step by step
Seven things to do:
- Start tracking first: track your food intake (as it is, without changing anything) without judgment to identify realistic areas for improvement.
- Add protein: add 10g of protein to three meals daily to improve satiety, aid fat loss, and retain muscle.
- Fiber swaps: swap foods for higher-fiber options where possible to improve gut health, improve heart health, support fat loss, and promote satiety.
- Hydration: take your body weight in kilograms (or half your body weight in pounds), then get that many ounces of water daily to support metabolism and reduce cravings.
- Calorie swaps: replace or reduce calorie-dense foods to create a small, modestly sustainable calorie deficit. Your body will still adjust to this after a while; that’s fine; it’s about a gradual reduction.
- Tweak and adjust: regularly reassess and adjust your diet and habits to fit your lifestyle and progress.
- Guard against complacency: track consistently, and stay on course.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
The Smartest Way To Get To 20% Body Fat (Or 10% For Men)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Hormone Therapy That Reduces Breast Cancer Risk & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Hormone Balancing Act
We’ve written before about menopausal HRT:
What You Should Have Been Told About Menopause Beforehand
…and even specifically about the considerations when it comes to breast cancer risk:
Menopausal Hormone Replacement Therapy
this really does bear reading, by the way—scroll down to the bit about breast cancer risk, because it’s not a simple increased/decreased risk; it can go either way, and which way it goes will depend on various factors including your medical history and what HRT, if any, you are taking.
Hormone Modulating Therapy
Hormone modulating therapy, henceforth HMT, is something a little different.
Instead of replacing hormones, as hormone replacement therapy does, guess what hormone modulating therapy does instead? That’s right…
MHT can modulate hormones by various means, but the one we’re going to talk about today does it by blocking estrogen receptors,
Isn’t that the opposite of what we want?
You would think so, but since for many people with an increased breast cancer risk, the presence of estrogen increases that risk, which leaves menopausal (peri- or post) people in an unfortunate situation, having to choose between increased breast cancer risk (with estrogen), or osteoporosis and increased dementia risk, amongst other problems (without).
However, the key here (in fact, that’s a very good analogy) is in how the blocker works. Hormones and their receptors are like keys and locks, meaning that the wrong-shaped hormone won’t accidentally trigger it. And when the right-shaped hormone comes along, it gets activated and the message (in this case, “do estrogenic stuff here!” gets conveyed). A blocker is sufficiently similar to fit into the receptor, without being so similar as to otherwise act as the hormone.
In this case, it has been found that HMT blocking estrogen receptors was sufficient to alleviate the breast cancer risk, while also being associated with a 7% lower risk of developing Alzheimer’s disease or related dementias, with that risk reduction being even greater for some demographics depending on race and age. Black women in the 65–74 age bracket enjoyed a 24% relative risk reduction, with white women of the same age getting an 11% relative risk reduction. Black women enjoyed the same benefits after that age, whereas white women starting it at that age did not get the same benefits. The conclusion drawn from this is that it’s good to start this at 65 if relevant and practicable, especially if white, because the protective effect is strongest when gained aged 65–69.
Here’s a pop-science article that goes into the details more deeply than we have room for here:
Hormone therapy for breast cancer linked with lower dementia risk
And here’s the paper itself; we highly recommend reading at least the abstract, because it goes into the numbers in much more detail than we reasonably can here. It’s a huge cohort study of 18,808 women aged 65 years or older, so this is highly relevant data:
Want to learn more?
If you’d like a much deeper understanding of breast cancer risk management, including in the context of hormone therapy, you might like this excellent book that we reviewed recently:
The Smart Woman’s Guide to Breast Cancer – by Dr. Jenn Simmons
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: