What’s the difference between shyness and social anxiety?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
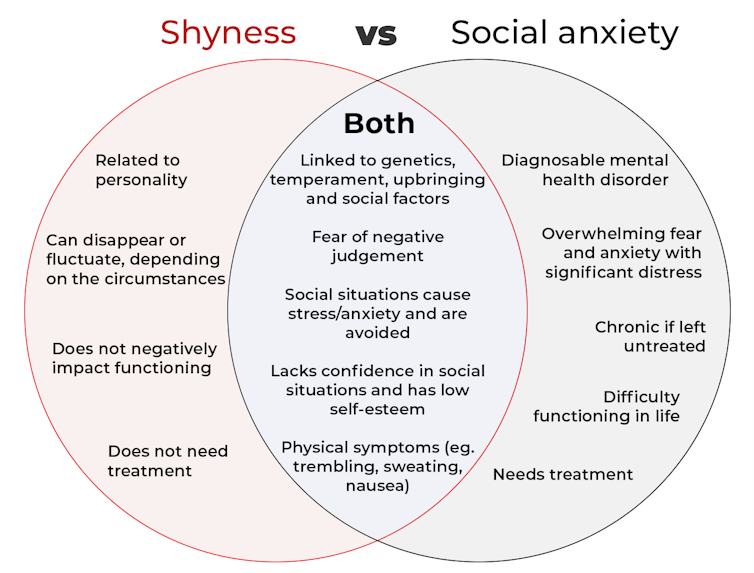
The terms “shyness” and “social anxiety” are often used interchangeably because they both involve feeling uncomfortable in social situations.
However, feeling shy, or having a shy personality, is not the same as experiencing social anxiety (short for “social anxiety disorder”).
Here are some of the similarities and differences, and what the distinction means.

How are they similar?
It can be normal to feel nervous or even stressed in new social situations or when interacting with new people. And everyone differs in how comfortable they feel when interacting with others.
For people who are shy or socially anxious, social situations can be very uncomfortable, stressful or even threatening. There can be a strong desire to avoid these situations.
People who are shy or socially anxious may respond with “flight” (by withdrawing from the situation or avoiding it entirely), “freeze” (by detaching themselves or feeling disconnected from their body), or “fawn” (by trying to appease or placate others).
A complex interaction of biological and environmental factors is also thought to influence the development of shyness and social anxiety.
For example, both shy children and adults with social anxiety have neural circuits that respond strongly to stressful social situations, such as being excluded or left out.
People who are shy or socially anxious commonly report physical symptoms of stress in certain situations, or even when anticipating them. These include sweating, blushing, trembling, an increased heart rate or hyperventilation.
How are they different?
Social anxiety is a diagnosable mental health condition and is an example of an anxiety disorder.
For people who struggle with social anxiety, social situations – including social interactions, being observed and performing in front of others – trigger intense fear or anxiety about being judged, criticised or rejected.
To be diagnosed with social anxiety disorder, social anxiety needs to be persistent (lasting more than six months) and have a significant negative impact on important areas of life such as work, school, relationships, and identity or sense of self.
Many adults with social anxiety report feeling shy, timid and lacking in confidence when they were a child. However, not all shy children go on to develop social anxiety. Also, feeling shy does not necessarily mean a person meets the criteria for social anxiety disorder.
People vary in how shy or outgoing they are, depending on where they are, who they are with and how comfortable they feel in the situation. This is particularly true for children, who sometimes appear reserved and shy with strangers and peers, and outgoing with known and trusted adults.
Individual differences in temperament, personality traits, early childhood experiences, family upbringing and environment, and parenting style, can also influence the extent to which people feel shy across social situations.

However, people with social anxiety have overwhelming fears about embarrassing themselves or being negatively judged by others; they experience these fears consistently and across multiple social situations.
The intensity of this fear or anxiety often leads people to avoid situations. If avoiding a situation is not possible, they may engage in safety behaviours, such as looking at their phone, wearing sunglasses or rehearsing conversation topics.
The effect social anxiety can have on a person’s life can be far-reaching. It may include low self-esteem, breakdown of friendships or romantic relationships, difficulties pursuing and progressing in a career, and dropping out of study.
The impact this has on a person’s ability to lead a meaningful and fulfilling life, and the distress this causes, differentiates social anxiety from shyness.
Children can show similar signs or symptoms of social anxiety to adults. But they may also feel upset and teary, irritable, have temper tantrums, cling to their parents, or refuse to speak in certain situations.
If left untreated, social anxiety can set children and young people up for a future of missed opportunities, so early intervention is key. With professional and parental support, patience and guidance, children can be taught strategies to overcome social anxiety.
Why does the distinction matter?
Social anxiety disorder is a mental health condition that persists for people who do not receive adequate support or treatment.
Without treatment, it can lead to difficulties in education and at work, and in developing meaningful relationships.
Receiving a diagnosis of social anxiety disorder can be validating for some people as it recognises the level of distress and that its impact is more intense than shyness.
A diagnosis can also be an important first step in accessing appropriate, evidence-based treatment.
Different people have different support needs. However, clinical practice guidelines recommend cognitive-behavioural therapy (a kind of psychological therapy that teaches people practical coping skills). This is often used with exposure therapy (a kind of psychological therapy that helps people face their fears by breaking them down into a series of step-by-step activities). This combination is effective in-person, online and in brief treatments.

For more support or further reading
Online resources about social anxiety include:
- This Way Up’s online program for managing excessive shyness and fear of social situations
- Beyond Blue’s resources on social anxiety
- a guide to looking after yourself if you have social anxiety, from the Western Australian health department
- social anxiety online program for children and teens from the University of Queensland
- inroads, a self-guided online program for young adults who drink alcohol to manage their anxiety.
We thank the Black Dog Institute Lived Experience Advisory Network members for providing feedback and input for this article and our research.
Kayla Steele, Postdoctoral research fellow and clinical psychologist, UNSW Sydney and Jill Newby, Professor, NHMRC Emerging Leader & Clinical Psychologist, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Seeds: The Good, The Bad, And The Not-Really-Seeds!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Doctors are great at saving lives like mine. I’m a two time survivor of colon cancer and have recently been diagnosed with Chron’s disease at 62. No one is the health system can or is prepared to tell me an appropriate diet to follow or what to avoid. Can you?❞
Congratulations on the survivorship!
As to Crohn’s, that’s indeed quite a pain, isn’t it? In some ways, a good diet for Crohn’s is the same as a good diet for most other people, with one major exception: fiber
…and unfortunately, that changes everything, in terms of a whole-foods majority plant-based diet.
What stays the same:
- You still ideally want to eat a lot of plants
- You definitely want to avoid meat and dairy in general
- Eating fish is still usually* fine, same with eggs
- Get plenty of water
What needs to change:
- Consider swapping grains for potatoes or pasta (at least: avoid grains)
- Peel vegetables that are peelable; discard the peel or use it to make stock
- Consider steaming fruit and veg for easier digestion
- Skip spicy foods (moderate spices, like ginger, turmeric, and black pepper, are usually fine in moderation)
Much of this latter list is opposite to the advice for people without Crohn’s Disease.
*A good practice, by the way, is to keep a food journal. There are apps that you can get for free, or you can do it the old-fashioned way on paper if prefer.
But the important part is: make a note not just of what you ate, but also of how you felt afterwards. That way, you can start to get a picture of patterns, and what’s working (or not) for you, and build up a more personalized set of guidelines than anyone else could give to you.
We hope the above pointers at least help you get going on the right foot, though!
❝Why do baked goods and deep fried foods all of a sudden become intolerable? I used to b able to ingest bakery foods and fried foods. Lately I developed an extreme allergy to Kiwi… what else should I “fear”❞
About the baked goods and the deep-fried foods, it’s hard to say without more information! It could be something in the ingredients or the method, and the intolerance could be any number of symptoms that we don’t know. Certainly, pastries and deep-fried foods are not generally substantial parts of a healthy diet, of course!
Kiwi, on the other hand, we can answer… Or rather, we can direct you to today’s “What’s happening in the health world” section below, as there is news on that front!
We turn the tables and ask you a question!
We’ll then talk about this tomorrow:
Share This Post
-
4 things ancient Greeks and Romans got right about mental health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
According to the World Health Organization, about 280 million people worldwide have depression and about one billion have a mental health problem of any kind.
People living in the ancient world also had mental health problems. So, how did they deal with them?
As we’ll see, some of their insights about mental health are still relevant today, even though we might question some of their methods.
Jr Morty/Shutterstock 1. Our mental state is important
Mental health problems such as depression were familiar to people in the ancient world. Homer, the poet famous for the Iliad and Odyssey who lived around the eighth century BC, apparently died after wasting away from depression.
Already in the late fifth century BC, ancient Greek doctors recognised that our health partly depends on the state of our thoughts.
In the Epidemics, a medical text written in around 400BC, an anonymous doctor wrote that our habits about our thinking (as well as our lifestyle, clothing and housing, physical activity and sex) are the main determinants of our health.
Homer, the ancient Greek poet, had depression. Thirasia/Shutterstock 2. Mental health problems can make us ill
Also writing in the Epidemics, an anonymous doctor described one of his patients, Parmeniscus, whose mental state became so bad he grew delirious, and eventually could not speak. He stayed in bed for 14 days before he was cured. We’re not told how.
Later, the famous doctor Galen of Pergamum (129-216AD) observed that people often become sick because of a bad mental state:
It may be that under certain circumstances ‘thinking’ is one of the causes that bring about health or disease because people who get angry about everything and become confused, distressed and frightened for the slightest reason often fall ill for this reason and have a hard time getting over these illnesses.
Galen also described some of his patients who suffered with their mental health, including some who became seriously ill and died. One man had lost money:
He developed a fever that stayed with him for a long time. In his sleep he scolded himself for his loss, regretted it and was agitated until he woke up. While he was awake he continued to waste away from grief. He then became delirious and developed brain fever. He finally fell into a delirium that was obvious from what he said, and he remained in this state until he died.
3. Mental illness can be prevented and treated
In the ancient world, people had many different ways to prevent or treat mental illness.
The philosopher Aristippus, who lived in the fifth century BC, used to advise people to focus on the present to avoid mental disturbance:
concentrate one’s mind on the day, and indeed on that part of the day in which one is acting or thinking. Only the present belongs to us, not the past nor what is anticipated. The former has ceased to exist, and it is uncertain if the latter will exist.
The philosopher Clinias, who lived in the fourth century BC, said that whenever he realised he was becoming angry, he would go and play music on his lyre to calm himself.
Doctors had their own approaches to dealing with mental health problems. Many recommended patients change their lifestyles to adjust their mental states. They advised people to take up a new regime of exercise, adopt a different diet, go travelling by sea, listen to the lectures of philosophers, play games (such as draughts/checkers), and do mental exercises equivalent to the modern crossword or sudoku.
Galen, a famous doctor, believed mental problems were caused by some idea that had taken hold of the mind. Pierre Roche Vigneron/Wikimedia For instance, the physician Caelius Aurelianus (fifth century AD) thought patients suffering from insanity could benefit from a varied diet including fruit and mild wine.
Doctors also advised people to take plant-based medications. For example, the herb hellebore was given to people suffering from paranoia. However, ancient doctors recognised that hellebore could be dangerous as it sometimes induced toxic spasms, killing patients.
Other doctors, such as Galen, had a slightly different view. He believed mental problems were caused by some idea that had taken hold of the mind. He believed mental problems could be cured if this idea was removed from the mind and wrote:
a person whose illness is caused by thinking is only cured by taking care of the false idea that has taken over his mind, not by foods, drinks, [clothing, housing], baths, walking and other such (measures).
Galen thought it was best to deflect his patients’ thoughts away from these false ideas by putting new ideas and emotions in their minds:
I put fear of losing money, political intrigue, drinking poison or other such things in the hearts of others to deflect their thoughts to these things […] In others one should arouse indignation about an injustice, love of rivalry, and the desire to beat others depending on each person’s interest.
4. Addressing mental health needs effort
Generally speaking, the ancients believed keeping our mental state healthy required effort. If we were anxious or angry or despondent, then we needed to do something that brought us the opposite of those emotions.
Watch some comedy, said physician Caelius Aurelianus. VCU Tompkins-McCaw Library/Flickr, CC BY-NC-SA This can be achieved, they thought, by doing some activity that directly countered the emotions we are experiencing.
For example, Caelius Aurelianus said people suffering from depression should do activities that caused them to laugh and be happy, such as going to see a comedy at the theatre.
However, the ancients did not believe any single activity was enough to make our mental state become healthy. The important thing was to make a wholesale change to one’s way of living and thinking.
When it comes to experiencing mental health problems, we clearly have a lot in common with our ancient ancestors. Much of what they said seems as relevant now as it did 2,000 years ago, even if we use different methods and medicines today.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Konstantine Panegyres, McKenzie Postdoctoral Fellow, researching Greco-Roman antiquity, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Fitness Walking and Bodyweight Exercises – by Frank S. Ring
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of exercise manuals assume that the reader has a “basic” body (nothing Olympian, but nothing damaged either). As we get older, increasingly few of us fall into the “but nothing damaged either” category!
Here’s where Ring brings to bear his decades of experience as a coach and educator, and also his personal recovery from a serious back injury.
The book covers direct, actionable exercise advice (with all manner of detail), and also offers mental health tips he’s learned along the way.
Ring, like us, is a big fan of keeping things simple, so he focusses on “the core four” of bodyweight exercises:
- Pushups
- Squats
- Lunges
- Planks
These four exercises get a whole chapter devoted to them, though! Because there are ways to make each exercise easier or harder, or have different benefits. For example, adjustments include:
- Body angle
- Points of contact
- Speed
- Pausing
- Range of motion
This, in effect, makes a few square meters of floor (and perhaps a chair or bench) your fully-equipped gym.
As for walking? Ring enjoys and extols the health benefits, and/but also uses his walks a lot for assorted mental exercises, and recommends we try them too.
A fine book for anyone who wants to gain and/or maintain good health, but doesn’t pressingly want to join a gym or start pumping iron!
Share This Post
Related Posts
-
How To Stay In Shape At 70
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Questions and Answers at 10almonds
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
I have a question: what are the pros and cons of older people (60+) taking creatine every day?
It depends what else you’re doing, as creatine mostly helps the muscles recover after exercise. So:
- iff you’re doing resistance training (such as weights or bodyweight training), or HIIT (High Intensity Interval Training), then creatine monohydrate may help you keep at that and keep doing well.
- if you’re just doing light-to-moderate exercises, you might not get much benefit from creatine!
The topic merits diving deeper though, so we’ll queue that for one of our “Research Review Monday” days!
I wanted to ask if you think marine collagen is decent to take. I’ve heard a lot of bad press about it
We don’t know what you’ve heard, but generally speaking it’s been found to be very beneficial to bones, joints, and skin! We wrote about it quite recently on a “Research Review Monday”:
See: We Are Such Stuff As Fish Are Made Of
Natural alternatives to medication for depression?
Great question! We did a mean feature a while back, but we definitely have much more to say! We’ll do another main feature soon, but in the meantime, here’s what we previously wrote:
See: The Mental Health First-Aid That You’ll Hopefully Never Need
^This covers not just the obvious, but also why the most common advice is not helpful, and practical tips to actually make manageable steps back to wellness, on days when “literally just survive the day” is one’s default goal.
I am now in the “aging” population. A great concern for me is Alzheimers. My father had it and I am so worried. What is the latest research on prevention?
One good thing to note is that while Alzheimer’s has a genetic component, it doesn’t appear to be hereditary per se. Still, good to be on top of these things, and it’s never too early to start with preventive measures!
You might like a main feature we did on this recently:
See: How To Reduce Your Alzheimer’s Risk
Side effects of statins, are they worth it? Depression, are antidepressants worth it?
About statins, that depends a lot on you, your circumstances, and—as it happens—your gender. We covered this in a main feature recently, but a short answer is: for most people, they may not be the best first choice, and could even make things worse. For some people, however, they really are just what’s needed.
- Factors that make them more likely better for you: being a man, or having atherosclerosis
- Factors that make them more likely worse for you: being a woman in general
Check out the main feature we did: Statins: His & Hers?
As for antidepressants? That depends a lot on you, your physiology, your depression, your circumstances, and more. We’ll definitely do a main feature on that sometime soon, as there’s a lot that most people don’t know!
I am interested in the following: Aging, Exercise, Diet, Relationships, Purpose, Lowering Stress
You’re going to love our Psychology Sunday editions of 10almonds!
You may particularly like some of these:
- Seriously Useful Communication Skills! ← this is about relationship stuff
- Lower Your Cortisol! (Here’s Why & How) ← about “the stress hormone”
- How To Set Your Anxiety Aside ← these methods work for stress too
(This coming Psychology Sunday will have a feature specifically on stress, so do make sure to read that when it comes out!)
Hair growth strategies for men combing caffeine and minoxidil?
Well, the strategy for that is to use caffeine and minoxidil! Some more specific tips, though:
- Both of those things need to be massaged (gently!) into your scalp especially around your hairline.
- In the case of caffeine, that boosts hair growth. No extra thought or care needed for that one.
- In the case of minoxidil, it reboots the hair growth cycle, so if you’ve only recently started, don’t be surprised (or worried) if you see more shedding in the first three months. It’s jettisoning your old hairs because new ones were just prompted (by the minoxidil) to start growing behind them. So: it will get briefly worse before it gets better, but then it’ll stay better… provided you keep using it.
- If you’d like other options besides minoxidil, finasteride is a commonly prescribed oral drug that blocks the conversion of testosterone to DHT, which latter is what tells your hairline to recede.
- If you’d like other options besides prescription drugs, saw palmetto performs comparably to finasteride (and works the same way).
- You may also want to consider biotin supplementation if you don’t already enjoy that
- Consider also using a dermaroller on your scalp. If you’re unfamiliar, this is a device that looks like a tiny lawn aerator, with many tiny needles, and you roll it gently across your skin.
- It can be used for promoting hair growth, as well as for reducing wrinkles and (more slowly) healing scars.
- It works by breaking up the sebum that may be blocking new hair growth, and also makes the skin healthier by stimulating production of collagen and elastin (in response to the thousands of microscopic wounds that the needles make).
- Sounds drastic, but it doesn’t hurt and doesn’t leave any visible marks—the needles are that tiny. Still, practise good sterilization and ensure your skin is clean when using it.
See: How To Use A Dermaroller ← also explains more of the science of it
PS: this question was asked in the context of men, but the information goes the same for women suffering from androgenic alepoceia—which is a lot more common than most people think!
How to get to sleep at night as fast and as naturally as possible? Thank you!
We’ll definitely write more on that! You might like these articles we wrote already, meanwhile:
- Beating The Insomnia Blues ← this one is general advice and tips
- Time For Some Pillow Talk ← this one compares and reviews some popular sleep apps
- Insomnia? High Blood Pressure? Try these! ← this one tackles the matter from a dietary angle
Q: How to be your best self after 60: Self motivation / Avoiding or limiting salt, sugar & alcohol: Alternatives / Ways to sneak in more movements/exercise
…and, from a different subscriber…
Q: Inflammation & over 60 weight loss. Thanks!
Here are some of our greatest hits on those topics:
- Where Nutrition Meets Habits ← focusing on food that’s all three of: healthy + easy + cheap
- How To Keep On Keeping On ← exercise tips for when the motivation wanes
- Keep Inflammation At Bay ← science-based tips and advice
Also, while we’ve recommended a couple of books on stopping (or reducing) drinking, we’ve not done a main feature on that, so we definitely will one of these days!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Minerals That Neutralize Viruses (While Being Harmless To Humans)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Researchers in Estonia and Sweden (it was a joint project, with five researchers from each country) have found a way to use titanium dioxide nanoparticles to neutralize viruses, including COVID & flu.
Titanium dioxide, yes, the common additive to foods, cosmetics, and more (in most cases, added as a non-bleaching whitening agent—simply, titanium dioxide is body-safe, white in color, and very reflective, making it a brilliant, shiny white). Also used in sunscreens, for its excellent safety profile and again, its full-spectrum reflectiveness.
See also: Who Screens The Sunscreens?
How it works
Some viruses, including coronaviruses and influenza viruses, have an outer layer that’s a lipid membrane. The researchers found (by testing against multiple viruses, and by using a control of silicotungstate polyoxymethalate nanoparticles), that the ability of titanium dioxide to bind to phospholipids (and ability that the silicotungstate polyoxymethalate doesn’t have) means that the nanoparticles bind to the virus’s outer case, thus preventing it from effectively entering human cells (which it needs to do in order to infect the host, as this is how viruses replicate themselves).
What this means, in practical terms
While more research will be needed to know whether this can be used in the medicinal sense, it already means that a nanoparticle spray can be used to create virus-neutralizing layers on surfaces and in air filters. This alone could greatly reduce transmission in enclosed spaces such as public transport (ranging from taxis to airplanes), as well as other places where people get packed into a small space.
If you have an air purifier at home, keep an eye out for when improved filters arrive on the market!
See also: What’s Lurking In Your Household Air?
Wait, you said “minerals”; are there more?
It seems so, but we can’t truly say for sure until they’ve been tested. However, the researchers see no reason why other small metal oxides that bind strongly to phospholipids shouldn’t work exactly the same way—which would include iron oxide (yes, as in rust) and aluminum oxide (the coating that automatically forms immediately when aluminum is exposed to oxygen (aluminum is so reactive to oxygen, that it’s almost impossible to get aluminum without an oxidized surface, unless you use something else to coat it, or cut it in an oxygen-free atmosphere and keep it there).
You can read the paper itself here:
Molecular mechanisms behind the anti corona virus activity of small metal oxide nanoparticles
And on a related note (different scientists, different science, similar principle, though, using mineral nanotechnology to kill microbes):
❝Researchers report that laboratory tests of their nanoflower-coated dressings demonstrate antibiotic, anti-inflammatory and biocompatible properties. They say these results show these tannic acid and copper(II) phosphate sprouted nanoflower bandages are promising candidates for treating infections and inflammatory conditions.❞
Read in full: This delicate nanoflower is downright deadly to bacteria
Want to learn more?
Check out:
Move over, COVID and Flu! We Have “Hybrid Viruses” To Contend With Now
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
5 Minute Posture Improvement Routine!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
McKay Lang walks us through it:
Step by Step
Breathing exercise:
- Place your hands on your lower abdomen.
- Take three deep breaths, focusing on body tension in the shoulders and neck… And release.
Shoulder squeeze:
- With your hands on your hips, inhale and squeeze your shoulders upwards.
- Hold your breath for 3–4 seconds, then exhale.
- Repeat two more times, holding the squeeze a little longer each time.
Upper shoulder massage:
- Massage your upper shoulder muscles to release tension stored there.
Overhead arm stretch:
- Raise your arms above your head, clasping each elbow with the opposite hand.
- Inhale deeply, stretch upwards, then exhale and release.
- Repeat, alternating elbows.
Neck and head push:
- Place your palms on the back of the head, and push your head into your hands (and vice versa, because of Newton’s Third Law of Motion).
- Do the same sideways (one side and then the other), to engage the other neck muscles.
Cool down:
- Gently unclasp your hands, bring your head upright, and massage your muscles. And breathe.
For variations and a visual demonstration of all, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
6 Ways To Look After Your Back
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: