Non-Alcohol Mouthwash vs Alcohol Mouthwash – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing non-alcohol mouthwash to alcohol mouthwash, we picked the alcohol.
Why?
Note: this is a contingent choice and is applicable to most, but not all, people.
In short, there has been some concern about alcohol mouthwashes increasing cancer risk, but research has shown this is only the case if you already have an increased risk of oral cancer (for example if you smoke, and/or have had an oral cancer before).
For those for whom this is not the case (for example, if you don’t smoke, and/or have no such cancer history), then best science currently shows that alcohol mouthwash does not cause any increased risk.
What about non-alcohol mouthwashes? Well, they have a different problem; they usually use chlorine-based chemicals like chlorhexidine or cetylpyridinium chloride, which are (exactly as the label promises) exceptionally good at killing oral bacteria.
(They’d kill us too, at higher doses, hence: swill and spit)
Unfortunately, much like the rest of our body, our mouth is supposed to have bacteria there and bad things happen when it doesn’t. In the case of our oral microbiome, cleaning it with such powerful antibacterial agents can kill our “good” bacteria along with the bad, which lowers the pH of our saliva (that’s bad; it means it is more acidic), and thus indirectly erodes tooth enamel.
You can read more about the science of all of the above (with references), here:
Toothpastes & Mouthwashes: Which Help And Which Harm?
Summary:
For most people, alcohol mouthwashes are a good way to avoid the damage that can be done by chlorhexidine in non-alcohol mouthwashes.
Here are some examples, but there will be plenty in your local supermarket:
Non-Alcohol, by Colgate | Alcohol, by Listerine
If you have had oral cancer, or if you smoke, then you may want to seek a third alternative (and also, please, stop smoking if you can).
Or, really, most people could probably skip mouthwashes, if you’ve good oral care already by other means. See also:
Toothpastes & Mouthwashes: Which Help And Which Harm?
(yes, it’s the same link as before, but we’re now drawing your attention to the fact it has information about toothpastes too)
If you do want other options though, might want to check out:
Less Common Oral Hygiene Options ← miswak sticks are especially effective
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Vegan Eager for Milk Alternatives
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Q: Thanks for the info about dairy. As a vegan, I look forward to a future comment about milk alternatives
Thanks for bringing it up! What we research and write about is heavily driven by subscriber feedback, so notes like this really help us know there’s an audience for a given topic!
We’ll do a main feature on it, to do it justice. Watch out for Research Review Monday!
Share This Post
-
Avoid Knee Surgery With This Proven Strategy (Over-50s Specialist Physio)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A diagnosis of knee arthritis can be very worrying, but it doesn’t necessarily mean a knee replacement surgery is inevitable. Here’s how to keep your knee better, for longer (and potentially, for life):
Flexing your good health
You know we wouldn’t let that “proven” go by unchallenged if it weren’t, so what’s the evidence for it? Research (papers linked in the video description) showed 70% of patients (so, not 100%, but 70% is good odds and a lot better than the alternative) with mild to moderate knee arthritis avoided surgery after following a specific protocol—the one we’re about to describe.
The key strategy is to focus on strengthening the quadriceps muscles for joint protection, as strong quads correlate with reduced pain. However, a full range of motion in the knee is essential for optimal quad function, so that needs attention too, and in fact is foundational (can’t strengthen a quadriceps that doesn’t have a range of motion available to it):
Steps to follow:
- Improve knee extension:
- Passive knee extension exercise: gently press your knee down while lying flat, to increase straightening.
- Weighted heel props: use light weights to encourage gradual knee straightening.
- Enhance knee flexion:
- Use a towel to gently pull the knee towards the body to improve bending range.
Regular practice (multiple times daily) leads to improved knee function and pain relief. Exercises should be performed gently and without pain, aiming for consistent, gradual progress.And of course, if you do experience pain, it is recommend to consult with a local physiotherapist for more personalized guidance.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Treat Your Own Knee – by Robin McKenzie
Take care!
Share This Post
- Improve knee extension:
-
Exercises for Sciatica Pain Relief
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Jessica Valant is a physiotherapist and Pilates teacher, and today she’s going to demonstrate some exercise that relieve (and also correct the cause of) sciatica pain.
Back to good health
You will need a large strap for one of these exercises; a Pilates strap is great, but you can also use a towel. The exercises are:
Pelvic Rocking Exercise:
- Lie on your back, feet flat, knees bent.
- Gently rock your pelvis forwards and backwards (50% effort, no glute squeezing).
Leg Stretch with Strap:
- Straighten your left leg and loop the strap around the ball of your right foot.
- Gently straighten and bend your right leg while holding the strap.
- Perform a “nerve glide” by flexing and pointing your foot (not a stretch, just gentle movement).
- Repeat on the left leg.
Piriformis Stretch:
- Bend your right knee and place your left ankle over it (figure-four position).
- For a deeper stretch, hold your right thigh and pull your legs inwards.
Lower Back Release:
- Let your legs fall gently to one side after stretching each leg, opening the lower back.
Back Extension:
- Lie on your belly, placing your elbows down, palms flat.
- Optional: push up slightly into a back bend if it feels comfortable.
Seated Stretching:
- Finish by sitting cross-legged or on a chair.
- Inhale while raising your arms up, exhale while lowering them down, then reach sideways with your arms to stretch.
- Perform gentle neck stretches by tilting your ear to your shoulder on each side.
She recommends doing these exercises daily for at least a few weeks, though you should start to see improvement in your symptoms immediately. Nothing here should cause a problem or make things worse, but if it does, stop immediately and consult a local physiotherapist for more personalized advice.
For more on all of this, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
6 Ways To Look After Your Back
Take care!
Share This Post
Related Posts
-
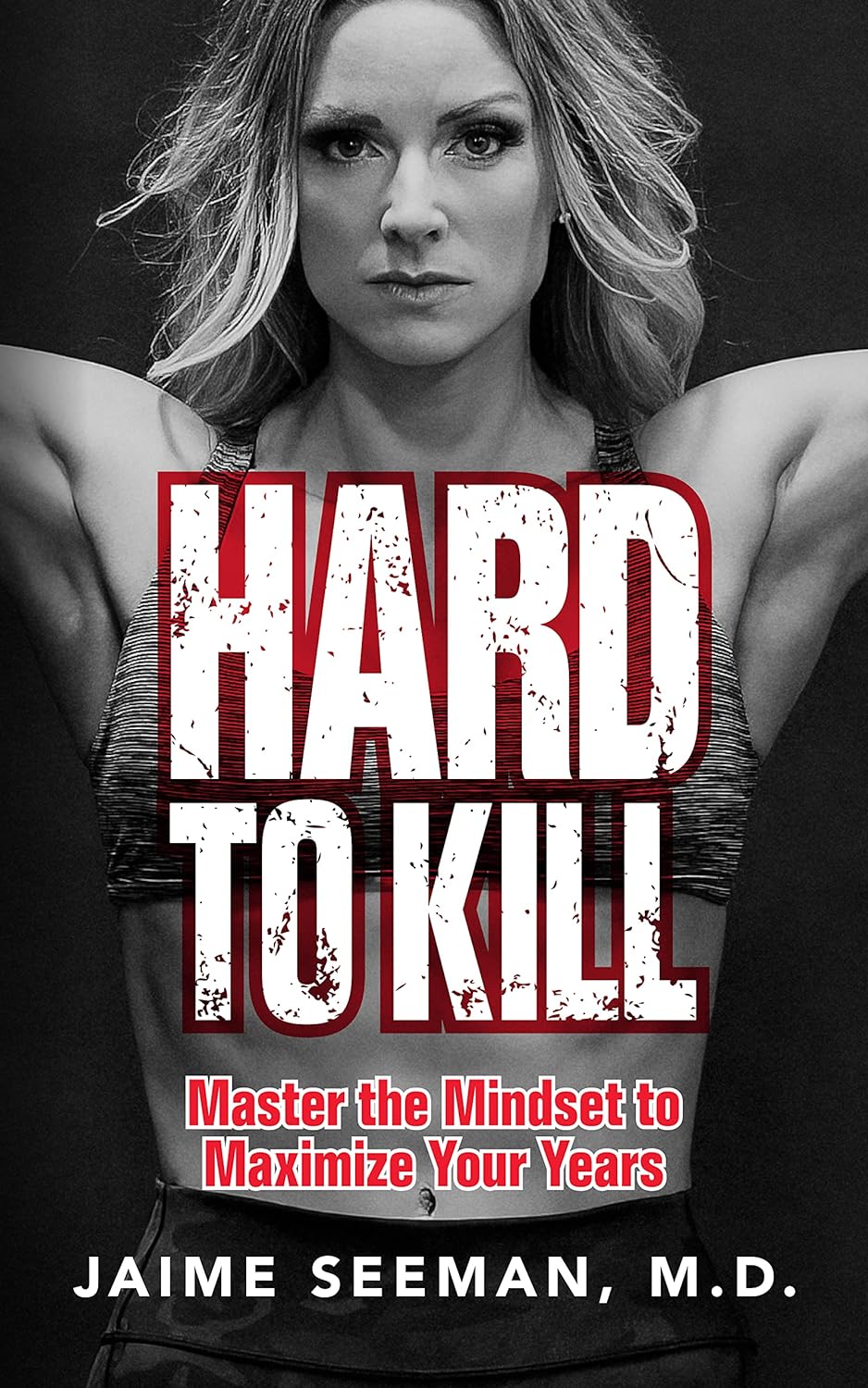
Hard to Kill – by Dr. Jaime Seeman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about Dr. Seeman’s method for robust health at all ages, focussing on:
- Nutrition
- Movement
- Sleep
- Mindset
- Environment
In this book, she expands on these things far more than we have room to in our little newsletter, including (importantly!) how each interplays with the others. She also follows up with an invitation to take the “Hard to Kill 30-Day Challenge”.
That said, in the category of criticism, it’s only 152 pages, and she takes some of that to advertise her online services in an effort to upsell the reader.
Nevertheless, there’s a lot of worth in the book itself, and the writing style is certainly easy-reading and compelling.
Bottom line: this book is half instructional, half motivational, and covers some very important areas of health.
Click here to check out “Hard to Kill”, and enjoy robust health at every age!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Five Key Traits Of Healthy Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Five Keys Of Aging Healthily
Image courtesy of Peter Prato. This is Dr. Daniel Levitin. He’s a neuroscientist, and his research focuses on aging, the brain, health, productivity, and creativity. Also music, and he himself is an accomplished musician also, but we’re not going to be focusing on that today.
We’re going to be looking at the traits that, according to science, promote healthy longevity in old age. In other words, the things that increase our healthspan, from the perspective of a cognitive scientist.
What does he say we should do?
Dr. Levitin offers us what he calls the “COACH” traits:
- Curiosity
- Openness
- Associations
- Conscientiousness
- Healthy practices
By “associations”, he means relationships. However, that would have made the acronym “CORCH”, and decisions had to be made.
Curiosity
Leonardo da Vinci had a list of seven traits he considered most important.
We’ll not go into those today (he is not our featured expert of the day!), but we will say that he agreed with Dr. Levitin on what goes at the top of the list: curiosity.
- Without curiosity, we will tend not to learn things, and learning things is key to keeping good cognitive function in old age
- Without curiosity, we will tend not to form hypotheses about how/why things are the way they are, so we will not exercise imagination, creativity, problem-solving, and other key functions of our brain
- Without curiosity, we will tend not to seek out new experiences, and consequently, our stimuli will be limited—and thus, so will our brains
Openness
Being curious about taking up ballroom dancing will do little for you, if you are not also open to actually trying it. But, openness is not just a tag-on to curiosity; it deserves its spot in its own right too.
Sometimes, ideas and opportunities come to us unbidden, and we have to be able to be open to those too. This doesn’t mean being naïve, but it does mean having at least a position of open-minded skepticism.
Basically, Dr. Levitin is asking us to be the opposite of the pejorative stereotype of “an old person stuck in their ways”.
Associations
People are complex, and so they bring complexities to our lives. Hopefully, positively stimulating ones. Without them to challenge us (again, hopefully in a positive way), we can get very stuck in a narrow field of experience.
And of course, having at least a few good friends has numerous benefits to health. There’s been a lot of research on this; 5 appears to be optimal.
- More than that, and the depth tends to tail off, and/or stresses ensue from juggling too many relationships
- Fewer than that, and we might be only a calendar clash away from loneliness
Friends provide social stimulation and mutual support; they’re good for our mental health and even our physiological immunity (counterintuitively, by means of shared germs).
And, a strong secure romantic relationship is something that has been found time and again to extend healthy life.
Note: by popular statistics, this benefit is conferred upon men partnered with women, men partnered with men, women partnered with women, but not women partnered with men.
There may be a causative factor that’s beyond the scope of this article which is about cognitive science, not feminism, but there could also be a mathematical explanation for this apparent odd-one-out:
Since women tend to live longer than men (who are also often older than their female partners), women who live the longest are often not in a relationship—precisely because they are widows. So these long-lived widows will tend to skew the stats, through no fault of their husbands.
On the flipside of this, for a woman to predecease her (statistically older and shorter-lived) husband will often require that she die quite early (perhaps due to accident or illness unrelated to age), which will again skew the stats to “women married to men die younger”, without anything nefarious going on.
Conscientiousness
People who score highly in the character trait “conscientiousness” will tend to live longer. The impact is so great, that a child’s scores will tend to dictate who dies in their 60s or their 80s, for example.
What does conscientiousness mean? It’s a broad character trait that’s scored in psychometric tests, so it can be things that have a direct impact on health, such as brushing one’s teeth, or things that are merely correlated, such as checking one’s work for typos (this writer does her best!).
In short, if you are the sort of person who attends to the paperwork for your taxes on time, you are probably also the sort of person who remembers to get your flu vaccination and cancer screening.
Healthy practices
This means “the usual things”, such as:
- Healthy diet (Mediterranean Diet consistently scores up top)
- Good exercise (especially the tendency to keep moving in general)
- Good sleep (7–9 hours, no compromises)
- Not drinking (or at least only very moderate consumption, but the only safe amount is zero)
- Not smoking (just don’t; there is no wiggle room on this one)
Want to learn more?
You can check out his book, which we reviewed all so recently, and you can also enjoy this video, in which he talks about matters concerning healthy aging from a neuroscientist’s perspective, ranging from heart health and neurodegeneration, to the myth of failing memory, to music and lifespan and more:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Undoing Creatine’s Puffiness Side Effect
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Creatine is known to increase “puffiness”, especially in my face. Are there any supplements that do the opposite?!❞
So first, let’s examine why this happens: creatine is most often taken to boost muscle size and performance. Your muscles are, of course, mostly water by mass, and so building your muscles requires extra water, which triggers systemic water retention.
In other words: you take creatine, exercise, and as the muscles start growing, the body goes “oh heck, we are running out of water, better save as much as possible in order to keep hydrating the muscles without running out” and starts putting it anywhere it can that’s not your bladder, so this will largely be the soft tissues of your body.
So, this results in classic water retentions symptoms including bloating and, yes, facial puffiness.
How much this happens, and how long the effects last, depend on three main things:
- What daily dose of creatine you are taking
- What kind of exercise you are doing
- What your hydration is like
The dose is relevant as it’s most common to get this puffiness during the “loading” phase, i.e. if you’re taking an increased dose to start with.
The exercise is relevant as it affects how much your body is actually using the water to build muscles.
The hydration is relevant because the less water you are taking, the more the body will try to retain whatever you do have.
This means, of course, that the supplement you are looking for to undo the facial puffiness is, in fact, water (even, nay, especially, if you feel bloated too):
Water For Everything? Water’s Counterintuitive Properties
Additionally, you could scale back the dose of creatine you’re taking, if you’re not currently doing heavy muscle-building exercise.
That said, the recommended dose for cognitive benefits is 5g/day, which is a very standard main-phase (i.e., post-loading) bodybuilding dose, so do with that information what you will.
See also: Creatine’s Brain Benefits Increase With Age
On which note: whether or not you want to take creatine for brain benefits, however, may depend on your age:
Creatine: Very Different For Young & Old People
Most research on creatine’s effects on humans has usually been either collegiate athletes or seniors, which leaves quite a research gap in the middle—so it’s unclear at what age the muscle-building effects begin to taper off, and at what age the cognitive benefits begin to take off.
Want a quicker fix?
If you want to reduce your facial puffiness acutely (e.g., you have a date in an hour and would like to not have a puffy face), then there are two things you can do that will help immediately, and/but only have short-term effects, meaning you’d have to do them daily to enjoy the results every day:
The first is an ice bath; simply fill a large bowl with water and ice cubes, give it a couple of minutes to get down to temperature, hold your breath and plunge your face in for as long as you can comfortably hold your breath. Repeat a few times, and towel off.
This helps by waking up the vasculature in your face, helping it to reduce puffiness naturally.
The second is facial yoga or guā shā, which is the practice of physically manipulating the soft tissues of your face to put them where you want them, rather than where you don’t want them. This will work against water retention puffiness, as well as cortisol puffiness, lymphatic puffiness, and more:
7-Minute Face Fitness For Lymphatic Drainage & Youthful Jawline
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: