Is Dairy Scary?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is Dairy Scary?
Milk and milk products are popularly enjoyed as a good source of calcium and vitamin D.
In contrast, critics of dairy products (for medical reasons, rather than ethical, which is another matter entirely and beyond the scope of this article) point to risks of cancer, heart disease, and—counterintuitively—osteoporosis. We’ll focus more on the former, but touch on the latter two before closing.
Dairy & Cancer
Evidence is highly conflicting. There are so many studies with so many different results. This is partially explicable by noting that not only is cancer a many-headed beast that comes in more than a hundred different forms and all or any of them may be affected one way or another by a given dietary element, but also… Not all milk is created equal, either!
Joanna Lampe, of the Public Health Sciences division, Fred Hutchinson Cancer Research Center in Seattle, writes:
❝Dairy products are a complex group of foods and composition varies by region, which makes evaluation of their association with disease risk difficult. For most cancers, associations between cancer risk and intake of milk and dairy products have been examined only in a small number of cohort studies, and data are inconsistent or lacking❞
In her systematic review of studies, she noted, for example, that:
- Milk and dairy products contain micronutrients and several bioactive constituents that may influence cancer risk and progression
- There’s probable association between milk intake and lower risk of colorectal cancer
- There’s a probable association between diets high in calcium and increased risk of prostate cancer
- Some studies show an inverse association between intake of cultured dairy products and bladder cancer (i.e., if you eat yogurt you’re less likely to get bladder cancer)
Since that systemic review was undertaken, more research has been conducted, and the results are… Not conclusive, but converging towards a conclusion:
- Dairy products can increase or decrease cancer risk
- The increase in cancer risk seems strongest when milk is consumed in quantities that result in too much calcium. When it comes to calcium, you can absolutely have too much of a good thing—just ask your arteries!
- The decrease in cancer seems to be mostly, if not exclusively, from fermented dairy products. This usually means yogurts. The benefit here is not from the milk itself, but rather from the gut-friendly bacteria.
You may be wondering: “Hardened arteries, gut microbiome health? I thought we were talking about cancer?” and yes we are. No part of your health is an island unrelated to other parts of your health. One thing can lead to another. Sometimes we know how and why, sometimes we don’t, but it’s best to not ignore the data.
The bottom line on dairy products and cancer is:
- Consuming dairy products in general is probably fine
- Yogurt, specifically, is probably beneficial
Dairy and Heart Disease
The reason for the concern is clear enough: it’s largely assumed to be a matter of saturated fat intake.
The best combination of “large” and “recent” that we found was a three-cohort longitudinal study in 2019, which pretty much confirms what was found in smaller or less recent studies:
- There is some evidence to suggest that consumption of dairy can increase all-cause mortality in general, and death from (cancer and) cardiovascular disease in particular
- The evidence is not, however, overwhelming. It is marginal.
Dairy and Osteoporosis
Does dairy cause osteoporosis? Research here tends to fall into one of two categories when it comes to conclusions, so we’ll give an example of each:
- “Results are conflicting, saying yes/no/maybe, and basically we just don’t know”
- “Results are conflicting, but look: cross-sectional and case-control studies say yes; cohort studies say maybe or no; we prefer the cohort studies”
See them for yourself:
- Osteoporosis: Is milk a kindness or a curse?
- Consumption of milk and dairy products and risk of osteoporosis and hip fracture
Conclusion: really, the jury is very much still out on this one
Summary:
- Moderate consumption of dairy products is almost certainly fine
- More specifically: it probably has some (small) pros and some (small) cons
- Yogurt is almost certainly healthier than other dairy products, and is almost universally considered a healthy food (assuming not being full of added sugar etc, of course)
- If you’re going to have non-dairy alternatives to milk, choose wisely!
That’s all we have time for today, but perhaps in a future edition we’ll do a run-down of the pros and cons of various dairy alternatives!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fatigue? Unexplained weight gain and dry skin? Could it be Hashimoto’s disease?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Maybe you feel worn out. Perhaps you’re also having trouble losing weight. Generally, you just don’t feel 100%.
Could it be Hashimoto’s disease? This common autoimmune thyroid disorder is when your immune system (which fights off viruses and bacteria), mistakenly attacks a part of your body. In this case, it’s your thyroid – a gland located at the base of your neck – and can cause low thyroid hormones levels (hypothyroidism).
Hypothyroidism affects one in 33 Australians and Hashimoto’s is one of the most common thyroid conditions in first-world countries.
While symptoms can be subtle, untreated Hashimoto’s can cause long-term problems with your heart, memory and fertility. Here is what you need to know.
What happens when you have Hashimoto’s?
Your thyroid gland is a butterfly-shaped gland in the neck. It is essential in regulating things like muscle function, digestion, metabolism, the heart and lungs. In children, thyroid hormones are also needed for normal growth and development.
Hashimoto’s thyroid disease, named after the Japanese doctor who discovered it in 1912, is also known as Hashimoto’s thyroiditis or chronic lymphocytic thyroiditis. The disease can cause the immune system to mistakenly produce proteins called antibodies (thyroid peroxidase and thyroglobulin). These can cause inflammation and long-term damage to the thyroid gland. Over time, as thyroid tissue is inflamed and/or destroyed, there can be a decrease in the production of thyroid hormones (hypothyroidism).
Hashimoto’s can present subtly at first. If you only have antibodies with no change in thyroid levels, it is likely you won’t have any symptoms.
However, as the disease progresses, you may experience fatigue, weight gain (or difficulty losing weight), increased sensitivity to the cold, constipation, dry skin, muscle aches, irregular or heavy menstrual cycles, enlarged thyroid (goitre) and occasionally hair loss, including at the ends of your eyebrows.
What causes Hashimoto’s thyroid disease?
Several risk factors can contribute to the development of Hashimoto’s including:
-
genetic risk – your risk is higher if you have family members with Hashimoto’s
-
gender – women are up to ten times more likely than men to develop the disease
-
age – you are more likely to develop the disease from 30 to 50 years of age
-
autoimmune condition – having another autoimmune condition like systemic lupus, Type 1 diabetes and celiac disease increases your risk
-
excessive iodine intake and radiation exposure may also increase risk in people who are already genetically at greater risk.
What are the long-term risks?
Long-term, untreated Hashimoto’s thyroiditis can cause heart issues, higher cholesterol levels, nerve damage (peripheral neuropathy), reduced cognition and infertility.
In pregnancy, Hashimoto’s has a higher risk of pre-eclampsia (high blood pressure affecting several organs), premature birth, placental abruption (when the placenta separates from the inner wall of the uterus before birth) and, in severe cases, pregnancy loss.
The disease has also been linked with an increased risk (but low incidence) of the lymphocytes of the thyroid turning into cancer cells to cause thyroid lymphoma.
How is Hashimoto’s diagnosed?
Diagnosis can be confirmed with a blood test to check thyroid levels and antibodies.
Thyroid peroxidase antibodies are commonly present but about 5% of patients test antibody-negative. In those people, diagnosis depends on the thyroid levels, clinical presentation and ultrasound appearance of general inflammation. An ultrasound may not be required though, especially if the diagnosis is obvious.
Three hormone levels are tested to determine if you have Hashimoto’s.
Thyroid stimulating hormone (TSH) is produced by the brain to speak to the thyroid, telling it to produce two types of thyroid hormones – T3 and T4.
If you have either relative or absolute thyroid hormone deficiency, a test will show the stimulating hormones as high because the brain is trying to get the thyroid to work harder.
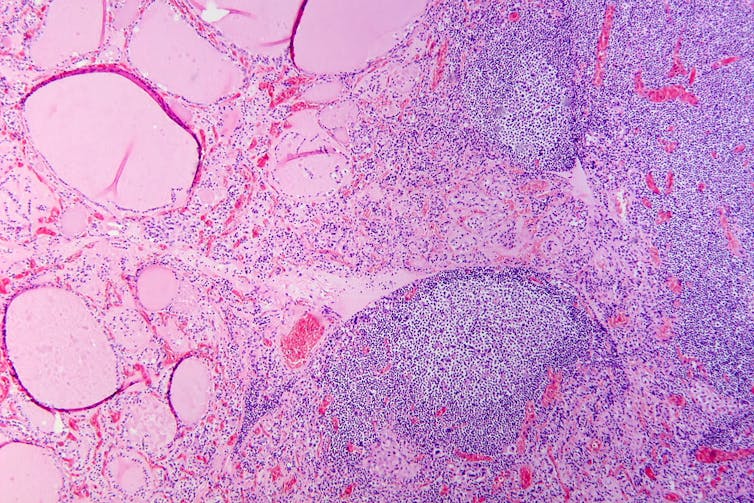
Hashimoto’s thyroiditis under the microscope. Antibodies against thyroid peroxidase and thyroglobulin were elevated.
Patho/Wikimedia Commons, CC BY-SACan it be treated?
The management of Hashimoto’s depends on the severity of the thyroid levels. Up to 20% of the population can have antibodies but normal thyroid levels. This is still Hashimoto’s thyroid disease, but it is very mild and does not require treatment. There is no current treatment to reduce antibody levels alone.
Because thyroid peroxidase antibodies increase the risk of abnormal thyroid levels in the future, regular thyroid testing is recommended.
When the thyroid stimulating hormone is high with normal thyroid hormone levels it is termed “subclinical hypothyroidism”. When it is paired with low hormone levels it is called “overt hypothyroidism”. The first is a mild form of the disease and treatment depends on the degree of stimulating hormone elevation.
Overt hypothyroidism warrants treatment. The main form of this is thyroid hormone replacement therapy (levothyroxine) with the dose of the drug adjusted until thyroid levels are within the normal range. This is usually a lifelong treatment but, once the dose is optimised, hormone levels usually remain relatively stable.
In some people with very enlarged thyroid glands causing compressive symptoms (such as difficulty swallowing or breathing), thyroidectomy (surgical removal of the thyroid) is considered.
Hashimoto’s thyroiditis is a common condition caused by your body’s immune system incorrectly damaging to your thyroid and can go undetected. Long-term, untreated, it can cause issues with your heart, cognition, and fertility. It can be diagnosed with a simple blood test. Speak to your doctor if you have any concerns as early diagnosis and treatment can help prevent complications.
Aakansha Zala, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
-
Blood, urine and other bodily fluids: how your leftover pathology samples can be used for medical research
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A doctor’s visit often ends with you leaving with a pathology request form in hand. The request form soon has you filling a sample pot, having blood drawn, or perhaps even a tissue biopsy taken.
After that, your sample goes to a clinical pathology lab to be analysed, in whichever manner the doctor requested. All this is done with the goal of getting to the bottom of the health issue you’re experiencing.
But after all the tests are done, what happens with the leftover sample? In most cases, leftover samples go in the waste bin, destined for incineration. Sometimes though, they may be used again for other purposes, including research.
Kaboompics.com/Pexels Who can use my leftover samples?
The samples we’re talking about here cover the range of samples clinical labs receive in the normal course of their testing work. These include blood and its various components (including plasma and serum), urine, faeces, joint and spinal fluids, swabs (such as from the nose or a wound), and tissue samples from biopsies, among others.
Clinical pathology labs often use leftover samples to practise or check their testing methods and help ensure test accuracy. This type of use is a vital part of the quality assurance processes labs need to perform, and is not considered research.
Leftover samples can also be used by researchers from a range of agencies such as universities, research institutes or private companies.
They may use leftover samples for research activities such as trying out new ideas or conducting small-scale studies (more on this later). Companies that develop new or improved medical diagnostic tests can also use leftover samples to assess the efficacy of their test, generating data needed for regulatory approval.
What about informed consent?
If you’ve ever participated in a medical research project such as a clinical trial, you may be familiar with the concept of informed consent. In this process, you have the opportunity to learn about the study and what your participation involves, before you decide whether or not to participate.
So you may be surprised to learn using leftover samples for research purposes without your consent is permitted in most parts of Australia, and elsewhere. However, it’s only allowed under certain conditions.
In Australia, the National Health and Medical Research Council (NHMRC) offers guidance around the use of leftover pathology samples.
One of the conditions for using leftover samples without consent for research is that they were received and retained by an accredited pathology service. This helps ensure the samples were collected safely and properly, for a legitimate clinical reason, and that no additional burdens or risk of harm to the person who provided the sample will be created with their further use.
Another condition is anonymity: the leftover samples must be deidentified, and not easily able to be reidentified. This means they can only be used in research if the identity of the donor is not needed.
Leftover pathology samples are sometimes used in medical research. hedgehog94/Shutterstock The decision to allow a particular research project to use leftover pathology samples is made by an independent human research ethics committee which includes consumers and independent experts. The committee evaluates the project and weighs up the risks and potential benefits before permitting an exemption to the need for informed consent.
Similar frameworks exist in the United States, the United Kingdom, India and elsewhere.
What research might be done on my leftover samples?
You might wonder how useful leftover samples are, particularly when they’re not linked to a person and their medical history. But these samples can still be a valuable resource, particularly for early-stage “discovery” research.
Research using leftover samples has helped our understanding of antibiotic resistance in a bacterium that causes stomach ulcers, Helicobacter pylori. It has helped us understand how malaria parasites, Plasmodium falciparum, damage red blood cells.
Leftover samples are also helping researchers identify better, less invasive ways to detect chronic diseases such as pulmonary fibrosis. And they’re allowing scientists to assess the prevalence of a variant in haemoglobin that can interfere with widely used diagnostic blood tests.
All of this can be done without your permission. The kinds of tests researchers do on leftover samples will not harm the person they were taken from in any way. However, using what would otherwise be discarded allows researchers to test a new method or treatment and avoid burdening people with providing fresh samples specifically for the research.
When considering questions of ethics, it could be argued not using these samples to derive maximum benefit is in fact unethical, because their potential is wasted. Using leftover samples also minimises the cost of preliminary studies, which are often funded by taxpayers.
The use of leftover pathology samples in research has been subject to some debate. Andrey_Popov/Shutterstock Inconsistencies in policy
Despite NHMRC guidance, certain states and territories have their own legislation and guidelines which differ in important ways. For instance, in New South Wales, only pathology services may use leftover specimens for certain types of internal work. In all other cases consent must be obtained.
Ethical standards and their application in research are not static, and they evolve over time. As medical research continues to advance, so too will the frameworks that govern the use of leftover samples. Nonetheless, developing a nationally consistent approach on this issue would be ideal.
Striking a balance between ensuring ethical integrity and fostering scientific discovery is essential. With ongoing dialogue and oversight, leftover pathology samples will continue to play a crucial role in driving innovation and advances in health care, while respecting the privacy and rights of individuals.
Christine Carson, Senior Research Fellow, School of Medicine, The University of Western Australia and Nikolajs Zeps, Professor, School of Public Health and Preventive Medicine, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Chatter – by Dr. Ethan Kross
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is about much more than just one’s internal monologue. It does tackle that, but also the many non-verbal rabbit-holes that our brains can easily disappear into.
The author is an experimental psychologist, and brings his professional knowledge and experience to bear on this problem—citing many studies, including his own studies from his own lab, in which he undertook to answer precisely the implicit questions of “How can I…” in terms of tackling these matters, from root anxiety (for example) to end-state executive dysfunction (for example).
The writing style isn’t dense science though, and is very approachable for all.
The greatest value in this book lies in its prescriptive element, that is to say, its advice, especially in the category of evidence-based things we can do to improve matters for ourselves; beyond generic things like “mindfulness-based stress reduction” to much more specific things like “observe yourself in the 3rd person for a moment” and “take a break to imagine looking back on this later” and “interrupt yourself with a brief manual task”. With these sorts of interventions and more, we can shift the voice in our head from critic to coach.
Bottom line: if you would like your brain to let you get on with the things you actually want to do instead of constantly sidetracking you, this is the book for you.
Share This Post
Related Posts
-
Fast. Feast. Repeat – by Dr. Gin Stephens
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed intermittent fasting books before, so what makes this one different?
The title “Fast. Feast. Repeat.” doesn’t give much away; after all, we already know that that’s what intermittent fasting is.
After taking the reader though the basics of how intermittent fasting works and what it does for the body, much of the rest of the book is given over to improvements.
That’s what the real strength of this book is: ways to make intermittent fasting more efficient, including how to avoid plateaus. After all, sometimes it can seem like the only way to push further with intermittent fasting is to restrict the eating window further. Not so!
Instead, Dr. Stephens gives us ways to keep confusing our metabolism (in a good way) if, for example, we had a weight loss goal we haven’t met yet.
Best of all, this comes without actually having to eat less.
Bottom line: if you want to be in good physical health, and/but also believe that life is for living and you enjoy eating food, then this book can resolve that age-old dilemma!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
8 Signs Of High Cortisol & How To Reverse “Cortisol Face”
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Shereene Idriss has insights about the facial features that might indicate chronically elevated cortisol levels, and what to do about same:
At face value
Dr. Idriss notes that for most people, this should not be cause for undue concern, although hypercortisolism can also be associated with genetic disorders such as Cushing’s syndrome, as well as prolonged use of certain medication, or the presence of certain tumors. As well as facial swelling, hypercortisolism can also result in other physical changes like acne, weight gain, skin thinning, stretch marks, infections, and hair loss.
As for what to do about it, she recommends addressing lifestyle factors like poor sleep, unhealthy diet, alcohol consumption, and lack of hydration to reduce facial puffiness related to stress. Diet suggestions include incorporating foods rich in magnesium, vitamin C, and omega-3s, such as leafy greens, fatty fish, nuts and seeds, and berries.
She also suggests some supplements to consider, such as ashwagandha, magnesium, omega-3s, and/or l-theanine, but you might want to speak to your doctor/pharmacist to check in case of contraindications per any other conditions you may have, or medications you may be on.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Lower Your Cortisol! (Here’s Why & How)
- Ashwagandha: The Root of All Even-Mindedness?
- L-Theanine: What’s The Tea?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Rebounding Into The Best Of Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Trampoline” is a brand-name that’s been popularized as a generic name, and “rebounding”, the name used in this video, is the same thing as “trampolining”. With that in mind, let us bounce swiftly onwards:
Surprising benefits
It’s easy to think “isn’t that cheating?” to the point that such “cheating” could be useless, since surely the device is doing most of the work?
The thing is, while indeed it’s doing a lot of the work for you, your muscles are still doing a lot—mostly stabilization work, which is of course a critical thing for our muscles to be able to do. While it’s rare that we need to do a somersault in everyday life, it’s common that we have to keep ourselves from falling over, after all.
It also represents a kind of gentle resistance exercise, and as such, improves bone density—something first discovered during NASA research for astronauts. Other related benefits pertain to the body’s ability to deal with acceleration and deceleration; it also benefits the lymphatic system, which unlike the blood’s circulatory system, has no pump of its own. Rebounding does also benefit the cardiovascular system, though, as now the heart gets confused (in the healthy way, a little like it gets confused with high-intensity interval training).
Those are the main evidence-based benefits; anecdotally (but credibly, since these things can be said of most exercise) it’s also claimed that it benefits posture, improves sleep and mood, promotes weight loss and better digestion, reduces bloating, improves skin (the latter being due to improved circulation), and alleviates arthritis (most moderate exercise improves immune response, and thus reduces chronic inflammation, so again, this is reasonable, even if anecdotal).
For more details on all of these and more, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Exercise Less, Move More
- How To Do HIIT (Without Wrecking Your Body)
- Resistance Is Useful! (Especially As We Get Older)
- HIIT, But Make It HIRT
- The Lymphatic System Against Cancer & More
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: