The Anti-Stress Herb That Also Fights Cancer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What does Rhodiola rosea actually do, anyway?
Rhodiola rosea (henceforth, “rhodiola”) is a flowering herb whose roots have adaptogenic properties.
In the cold, mountainous regions of Europe and Asia where it grows, it has been used in herbal medicine for centuries to alleviate anxiety, fatigue, and depression.
What does the science say?
Well, let’s just say the science is more advanced than the traditional use:
❝In addition to its multiplex stress-protective activity, Rhodiola rosea extracts have recently demonstrated its anti-aging, anti-inflammation, immunostimulating, DNA repair and anti-cancer effects in different model systems❞
Nor is how it works a mystery, as the same paper explains:
❝Molecular mechanisms of Rhodiola rosea extracts’s action have been studied mainly along with one of its bioactive compounds, salidroside. Both Rhodiola rosea extracts and salidroside have contrasting molecular mechanisms on cancer and normal physiological functions.
For cancer, Rhodiola rosea extracts and salidroside inhibit the mTOR pathway and reduce angiogenesis through down-regulation of the expression of HIF-1α/HIF-2α.
For normal physiological functions, Rhodiola rosea extracts and salidroside activate the mTOR pathway, stimulate paracrine function and promote neovascularization by inhibiting PHD3 and stabilizing HIF-1α proteins in skeletal muscles❞
~ Ibid.
And, as for the question of “do the supplements work?”,
❝In contrast to many natural compounds, salidroside is water-soluble and highly bioavailable via oral administration❞
~ Ibid.
And as to how good it is:
❝Rhodiola rosea extracts and salidroside can impose cellular and systemic benefits similar to the effect of positive lifestyle interventions to normal physiological functions and for anti-cancer❞
~ Ibid.
Source: Rhodiola rosea: anti-stress, anti-aging, and immunostimulating properties for cancer chemoprevention
But that’s not all…
We can’t claim this as a research review if we only cite one paper (even if that paper has 144 citations of its own), and besides, it didn’t cover all the benefits yet!
Let’s first look at the science for the “traditional use” trio of benefits:
When you read those, what are your first thoughts?
Please don’t just take our word for things! Reading even just the abstracts (summaries) at the top of papers is a very good habit to get into, if you don’t have time (or easy access) to read the full text.
Reading the abstracts is also a very good way to know whether to take the time to read the whole paper, or whether it’s better to skip onto a different one.
- Perhaps you noticed that the paper we cited for anxiety was quite a small study.
- The fact is, while we found mountains of evidence for rhodiola’s anxiolytic (antianxiety) effects, they were all small and/or animal studies. So we picked a human study and went with it as illustrative.
- Perhaps you noticed that the paper we cited for fatigue pertained mostly to stress-related fatigue.
- This, we think, is a feature not a bug. After all, most of us experience fatigue because of the general everything of life, not because we just ran a literal marathon.
- Perhaps you noticed that the paper we cited for depression said it didn’t work as well as sertraline (a very common pharmaceutical SSRI antidepressant).
- But, it worked almost as well and it had far fewer adverse effects reported. Bear in mind, the side effects of antidepressants are the reason many people avoid them, or desist in taking them. So rhodiola working almost as well as sertraline for far fewer adverse effects, is quite a big deal!
Bonus features
Rhodiola also putatively offers protection against Alzheimer’s disease, Parkinson’s disease, and cerebrovascular disease in general:
Rosenroot (Rhodiola): Potential Applications in Aging-related Diseases
It may also be useful in the management of diabetes (types 1 and 2), but studies so far have only been animal studies, and/or in vitro studies. Here are two examples:
- Antihyperglycemic action of rhodiola-aqeous extract in type 1 diabetic rats
- Evaluation of Rhodiola crenulata and Rhodiola rosea for management of type 2 diabetes and hypertension
How much to take?
Dosages have varied a lot in studies. However, 120mg/day seems to cover most bases. It also depends on which of rhodiola’s 140 active compounds a particular benefit depends on, though salidroside and rosavin are the top performers.
Where to get it?
As ever, we don’t sell it (or anything else) but here’s an example product on Amazon.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Stay A Step Ahead Of Peripheral Artery Disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Far less well-known than Coronary Artery Disease, it can still result in loss of life and limb (not in that order). Fortunately, there are ways to be on your guard:
What it is
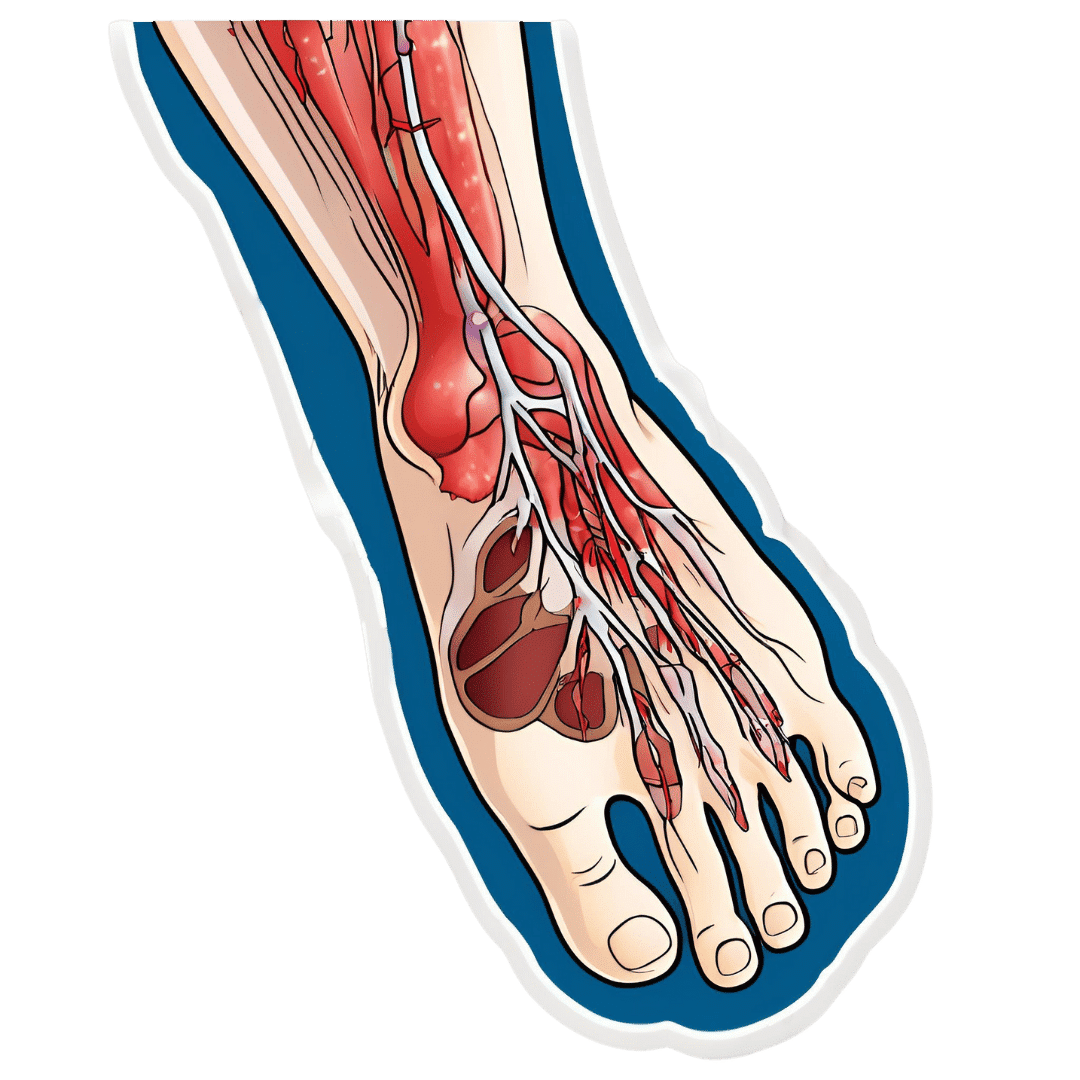
Peripheral Artery Disease (PAD) is the same thing as Coronary Artery Disease (CAD), just, in the periphery—which by definition means “outside of the heart and brain”, but in practice, it starts with the extremities. And of the extremities, it tends to start with the feet and legs, for the simple reason that if someone’s circulation is sluggish, then because of gravity, that’s where’s going to get blocked first.
In both CAD and PAD, the usual root cause is atherosclerosis, that is to say, the build-up of fatty material inside the arteries, usually commensurate to LDL (“bad”) cholesterol, especially in men (high LDL is still a predictor of cardiovascular disease in women though, just more modestly so, at least pre-menopause or in cases of treated menopause whereby HRT has returned hormones to pre-menopause levels).
See also: Demystifying Cholesterol
And for that about sex differences: His & Hers: The Hidden Complexities of Statins and Cardiovascular Disease (CVD)
Why it is
This one’s straightforward, as it’s the same things as any kind of cardiovascular disease: high blood pressure, high cholesterol, older age, obesity, smoking, drinking, diabetes, and genetic factors (so, a risk factor is: family history of heart disease).
However, while those are the main causes and/or risk factors, it absolutely can still strike other people, so it’s as well to be watch out for…
What to look out for
Many people first notice signs and symptoms that turn out to be PAD when they experience pain or numbness in the foot or feet, and/or a discoloration of the feet (especially toes), and slow wound healing.
At that stage, chances are you will need to go urgently to a specialist, and surgery is a likely necessity. With a little luck, it’ll be a minimally-invasive surgery to unblock an artery; failing that, an amputation will be in order.
At that stage, under 50% will be alive 5 years from diagnosis:
You probably want to avoid those. Good news is, you can, by catching it earlier!
What to look out for before that
The most common test for PAD is one you can do at home, but enlisting a nurse to do it for you will help ensure accurate readings. It’s called the Ankle-Brachial Index (ABI) test, and it involves comparing the blood pressure in your ankle with the blood pressure in your arm, and expressing them as a ratio.
Here’s how to do it (instructions and a video demonstration if you want it):
Do Try This At Home: ABI Test For Clogged Arteries
If you need a blood pressure monitor, by the way, here’s an example product on Amazon.
- A healthy ABI score is between 1.0 and 1.4; anything outside this range may indicate arterial problems.
- Low ABI scores (below 0.8) suggest plaque is likely obstructing blood flow
- High ABI scores (above 1.4) may indicate artery hardening
Do note also that yes, if you have plaque obstructing blood flow and hardened arteries, your scores may cancel out and give you a “healthy” score, despite your arteries being very much not healthy.
For this reason, this test can be used to raise the alarm, but not to give the “all clear”.
There are other tests that clinicians can do for you, but you can’t do at home unless you have an MRI machine, a CT scanner, an x-ray machine, a doppler-and-ultrasound machine, etc. We’ll not go into those in detail here, but ask your doctor about them if you’re concerned.
What to do about it
In the mid-to-late stages of the disease, the options are medication and surgery, respectively, but your doctor will advise about those in that eventuality.
In the early stages of the disease, the first-line recommend treatment is exercise, of which, especially walking:
Lower Extremity Peripheral Artery Disease: Diagnosis and Treatment
Given that this more often happens when someone hasn’t been walking so much, it can be a walk-rest-walk approach at first (a treadmill on a low setting can be very useful for this):
See also: Exercise Comparison Head-to-Head: Treadmill vs Road
Take care!
Share This Post
-
Banana Bread vs Bagel – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing banana bread to bagel, we picked the bagel.
Why?
Unlike most of the items we compare in this section, which are often “single ingredient” or at least highly standardized, today’s choices are rather dependent on recipe. Certainly, your banana bread and your bagels may not be the same as your neighbor’s. Nevertheless, to compare averages, we’ve gone with the FDA’s Food Central Database for reference values, using the most default average recipes available. Likely you could make either or both of them a little healthier, but as it is, this is how we’ve gone about making it a fair comparison. With that in mind…
In terms of macros, bagels have more than 2x the protein and about 4x the fiber, while banana bread has slightly higher carbs and about 7x more fat. You may be wondering: are the fats healthy? And the answer is, it could be better, could be worse. The FDA recipe went with margarine rather than butter, which lowered the saturated fat to being only ¼ of the total fat (it would have been higher, had they used butter) whereas bagels have no saturated fat at all—which characteristic is quite integral to bagels, unless you make egg bagels, which is rather a different beast. All in all, the macros category is a clear win for bagels, especially when we consider the carb to fiber ratio.
In the category of vitamins, bagels have on average more vitamin B1, B3, B5, and B9, while banana bread has on average more of vitamins A and C. A modest win for bagels.
When it comes to minerals, bagels are the more nutrient dense with more copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while banana bread is not higher in any minerals. An obvious and easy win for bagels.
Closing thoughts: while the micronutrient profile quite possibly differs wildly from one baker to another, something that will probably stay more or less the same regardless is the carb to fiber ratio, and protein to fat. As a result, we’d weight the macros category as the more universally relevant. Bagels won in all categories today, as it happened, but it’s fairly safe to say that, on average, a baker who makes bagels and banana bread with the same levels of conscientiousness for health (or lack thereof) will tend to make bagels that are healthier than banana bread, based on the carb to fiber ratio, and the protein to fat ratio.
Enjoy!
Want to learn more?
You might like to read:
- Should You Go Light Or Heavy On Carbs?
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Wholewheat Bread vs Seeded White – Which is Healthier?
Take care!
Share This Post
-
Twenty-One, No Wait, Twenty Tweaks For Better Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Greger’s 21 Tweaks… We say 20, though!
We’ve talked before about Dr. Greger’s Daily Dozen (12 things he advises that we make sure to eat each day, to enjoy healthy longevity), but much less-talked-about are his “21 Tweaks”…
They are, in short, a collection of little adjustments one can make for better health. Some of them are also nutritional, but many are more like lifestyle tweaks. Let’s do a rundown:
At each meal:
- Preload with water
- Preload with “negative calorie” foods (especially: greens)
- Incorporate vinegar (1-2 tbsp in a glass of water will slow your blood sugar increase)
- Enjoy undistracted meals
- Follow the 20-minute rule (enjoy your meal over the course of at least 20 minutes)
Get your daily doses:
- Black cumin ¼ tsp
- Garlic powder ¼ tsp
- Ground ginger (1 tsp) or cayenne pepper (½ tsp)
- Nutritional yeast (2 tsp)
- Cumin (½ tsp)
- Green tea (3 cups)
Every day:
- Stay hydrated
- Deflour your diet
- Front-load your calories (this means implementing the “king, prince, pauper” rule—try to make your breakfast the largest meal of your day, followed my a medium lunch, and a small evening meal)
- Time-restrict your eating (eat your meals within, for example, an 8-hour window, and fast the rest of the time)
- Optimize exercise timing (before breakfast is best for most people, unless you are diabetic)
- Weigh yourself twice a day (doing this when you get up and when you go to bed results in much better long-term weight management than weighing only once per day)
- Complete your implementation intentions (this sounds a little wishy-washy, but it’s about building a set of “if this, then that” principles, and then living by them. An example could be directly physical health-related such as “if there is a choice of stairs or elevator, I will take the stairs”, or could be more about holistic good-living, such as “if someone asks me for help, I will try to oblige them so far as I reasonably can”)
Every night:
- Fast after 7pm
- Get sufficient sleep (7–9 hours is best. As we get older, we tend more towards the lower end of that, but try get at least those 7 hours!)
Experiment with Mild Trendelenburg(better yet, skip this one)*
*This involves a 6º elevation of the bed, at the foot end. Dr. Greger advises that this should only be undertaken after consulting your doctor, though, as a lot of health conditions can contraindicate it. We at 10almonds couldn’t find any evidence to support this practice, and numerous warnings against it, so we’re going to go ahead and say we think this one’s skippable.
Again, we do try to bring you the best evidence-based stuff here at 10almonds, and we’re not going to recommend something just because of who suggested it
As for the rest, you don’t have to do them all! And you may have noticed there was a little overlap in some of them. But, we consider them a fine menu of healthy life hacks from which to pick and choose!
Share This Post
Related Posts
-
A Fresh Take On Hypothyroidism
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Three Rs To Boost Thyroid-Related Energy Levels
This is Dr. Izabella Wentz. She’s a doctor of pharmacology, and after her own diagnosis with Hashimoto’s thyroiditis, she has taken it up as her personal goal to educate others on managing hypothyroidism.
Dr. Wentz is also trained in functional medicine through The Institute for Functional Medicine, Kalish Functional Medicine, and the American Academy of Anti-Aging Medicine. She is a Fellow of the American Society of Consultant Pharmacists, and holds certifications in Medication Therapy Management as well as Advanced Diabetes Care through the American Pharmacists Association. In 2013, she received the Excellence in Innovation Award from the Illinois Pharmacists Association.
Dr. Wentz’s mission
Dr. Wentz was disenchanted by the general medical response to hypothyroidism in three main ways. She tells us:
- Thyroid patients are not diagnosed appropriately.
- For this, she criticises over-reliance on TSH tests that aren’t a reliable marker of thyroid function, especially if you have Hashimoto’s.
- Patients should be better optimized on their medications.
- For this, she criticizes many prescribed drugs that are actually pro-drugs*, that don’t get converted adequately if you have an underactive thyroid.
- Lifestyle interventions are often ignored by mainstream medicine.
- Medicines are great; they truly are. But medicating without adjusting lifestyle can be like painting over the cracks in a crumbling building.
*a “pro-drug” is what it’s called when the drug we take is not the actual drug the body needs, but is a precursor that will get converted to that actual drug we need, inside our body—usually by the liver, but not always. An example in this case is T4, which by definition is a pro-drug and won’t always get correctly converted to the T3 that a thyroid patient needs.
Well that does indeed sound worthy of criticism. But what does she advise instead?
First, she recommends a different diagnostic tool
Instead of (or at least, in addition to) TSH tests, she advises to ask for TPO tests (thyroid peroxidase), and a test for Tg antibodies (thyroglobulin). She says these are elevated for many years before a change in TSH is seen.
Next, identify the root cause and triggers
These can differ from person to person, but in countries that add iodine to salt, that’s often a big factor. And while gluten may or may not be a factor, there’s a strong correlation between celiac disease and Hashimoto’s disease, so it is worth checking too. Same goes for lactose.
By “checking”, here we mean testing eliminating it and seeing whether it makes a difference to energy levels—this can be slow, though, so give it time! It is best to do this under the guidance of a specialist if you can, of course.
Next, get to work on repairing your insides.
Remember we said “this can be slow”? It’s because your insides won’t necessarily bounce back immediately from whatever they’ve been suffering from for what’s likely many years. But, better late than never, and the time will pass anyway, so might as well get going on it.
For this, she recommends a gut-healthy diet with specific dietary interventions for hypothyroidism. Rather than repeat ourselves unduly here, we’ll link to a couple of previous articles of ours, as her recommendations match these:
She also recommends regular blood testing to see if you need supplementary TSH, TPO antibodies, and T3 and T4 hormones—as well as vitamin B12.
Short version
After diagnosis, she recommends the three Rs:
- Remove the causes and triggers of your hypothyroidism, so far as possible
- Repair the damage caused to your body, especially your gut
- Replace the thyroid hormones and related things in which your body has become deficient
Learn more
If you’d like to learn more about this, she offers a resource page, with resources ranging from on-screen information, to books you can get, to links to hook you up with blood tests if you need them, as well as recommended supplements to consider.
She also has a blog, which has an interesting relevant article added weekly.
Enjoy, and take care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Thyroid patients are not diagnosed appropriately.
-
How To Escape From A Despairing Mood
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When we are in a despairing mood, that’s when it can feel hardest to actually implement anything we know about getting out of one. That’s why sometimes, the simplest solutions are the best:
Imagination Is Key
Despairing moods occur when it’s hard to envision a better life. Imagination is the power to envision alternatives, such as new jobs, relationships, or lifestyle, but sadness can cloud our ability to imagine solutions like changing careers, moving house, or starting fresh. With enough imagination, most problems can be worked around—and new opportunities can always be found.
Importantly: we are not bound by our past or present circumstances; we have the freedom and flexibility to choose new paths. That doesn’t mean it’ll always be a walk in the park, but “this too shall pass”.
You may be thinking: “sometimes the hardship does pass, but can last many years”, and that is true. All the more reason to check if there’s a freer lane you can slip into to speed ahead. Even if there isn’t, the mere act of imagining such lanes is already respite from the hardships—and having envisioned such will make it much easier for you to recognise when opportunities for change do come along.
To foster imagination, we are advised to expose ourselves to different narratives, preparing ourselves for alternative ways of living. Thus, we can reframe life’s challenges as intellectual puzzles, urging us to rebuild creatively and find new solutions!
For more on all this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Behavioral Activation Against Depression & Anxiety
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
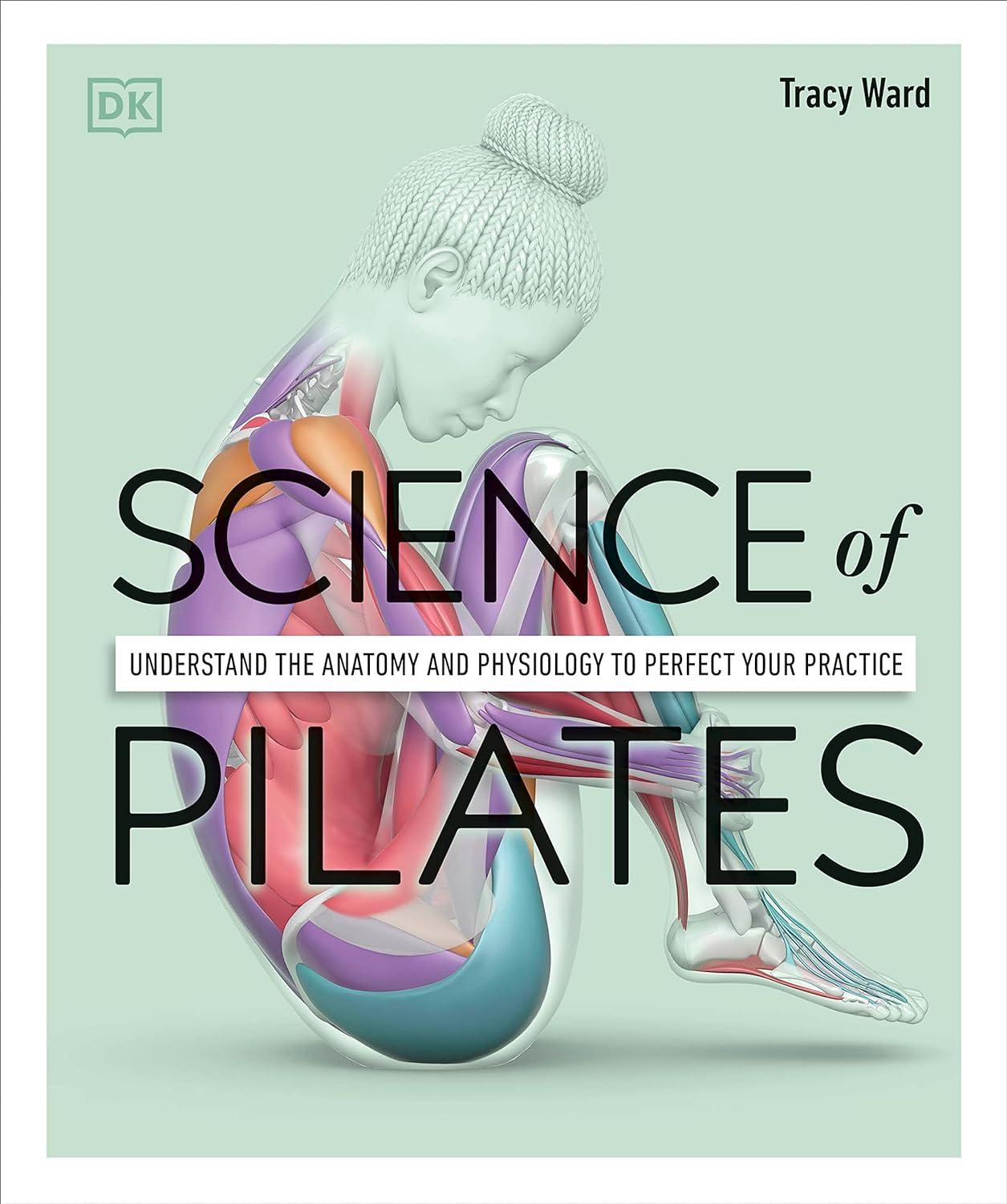
Science of Pilates – by Tracy Ward
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed other books in this series, “Science of Yoga” and “Science of HIIT” (they’re great too; check them out!). What does this one add to the mix?
Pilates is a top-tier “combination exercise” insofar as it checks a lot of boxes, e.g:
- Strength—especially core strength, but also limbs
- Mobility—range of motion and resultant reduction in injury risk
- Stability—impossible without the above two things, but Pilates trains this too
- Fitness—many dynamic Pilates exercises can be performed as cardio and/or HIIT.
The author, a physiotherapist, explains (as the title promises!) the science of Pilates, with:
- the beautifully clear diagrams we’ve come to expect of this series,
- equally clear explanations, with a great balance of simplicity of terms and depth where necessary, and
- plenty of citations for the claims made, linking to lots of the best up-to-date science.
Bottom line: if you are in a position to make a little time for Pilates (if you don’t already), then there is nobody who would not benefit from reading this book.
Click here to check out Science of Pilates, and keep your body well!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: