The Mediterranean Diet: What Is It Good For?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More to the point: what isn’t it good for?
- It’s been found to reduce all-cause mortality, which is about the best thing one can say of any diet.
- It’s especially good for heart health and against cancer.
- It’s particularly recommended for the prevention or management of diabetes.
- It’s also been found, societally, to reduce general healthcare costs—basically, people get sick less and so have fewer healthcare costs.
What brought it to the attention of the world’s scientific community?
Back in the 1950s, physiologist Ancel Keys wondered why poor people in Italian villages were healthier than wealthy New Yorkers. Upon undertaking studies, he narrowed it down to the Mediterranean diet—something he’d then take on as a public health cause for the rest of his career.
Keys himself lived to the ripe old age of 100, by the way.
When we say “Mediterranean Diet”, what image comes to mind?
We’re willing to bet that tomatoes feature (great source of lycopene, by the way), but what else?
- Salads, perhaps? Vegetables, olives? Olive oil, yea or nay?
- Bread? Pasta? Prosciutto, salami? Cheese?
- Pizza but only if it’s Romana style, not Chicago?
- Pan-seared liver, with some fava beans and a nice Chianti?
In reality, the diet is based on what was historically eaten specifically by Italian peasants. If the word “peasants” conjures an image of medieval paupers in smocks and cowls, and that’s not necessarily wrong, further back historically… but the relevant part here is that they were people who lived and worked in the countryside.
They didn’t have money for meat, which was expensive, nor the industrial setting for refined grain products to be affordable. They didn’t have big monocrops either, which meant no canola oil, for example… Olives produce much more easily extractable oil per plant, so olive oil was easier to get. Nor, of course, did they have the money (or infrastructure) for much in the way of imports.
So what foods are part of “the” Mediterranean Diet?
- Fruits. These would be fruits grown locally, but no need to sweat that, dietwise. It’s hard to go wrong with fruit.
- Tomatoes yes. So many tomatoes. (Knowledge is knowing tomato is a fruit. Wisdom is not putting it in a fruit salad)
- Non-starchy vegetables (e.g. eggplant yes, potatoes no)
- Greens (spinach, kale, lettuce, all those sorts of things)
- Beans and other legumes (whatever was grown nearby)
- Whole grain products in moderation (wholegrain bread, wholewheat pasta)
- Olives and olive oil. Special category, single largest source of fat in the Mediterranean diet, but don’t overdo it.
- Dairy products in moderation (usually hard cheeses, as these keep well)
- Fish, in moderation. Typically grilled, baked, steamed even. Not fried.
- Other meats as a rarer luxury in considerable moderation. There’s more than one reason prosciutto is so thinly sliced!
Want to super-power this already super diet?
Try: A Pesco-Mediterranean Diet With Intermittent Fasting: JACC Review Topic of the Week
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Lost for words? Research shows art therapy brings benefits for mental health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Creating art for healing purposes dates back tens of thousands of years, to the practices of First Nations people around the world. Art therapy uses creative processes, primarily visual art such as painting, drawing or sculpture, with a view to improving physical health and emotional wellbeing.
When people face significant physical or mental ill-health, it can be challenging to put their experiences into words. Art therapists support people to explore and process overwhelming thoughts, feelings and experiences through a reflective art-making process. This is distinct from art classes, which often focus on technical aspects of the artwork, or the aesthetics of the final product.
Art therapy can be used to support treatment for a wide range of physical and mental health conditions. It has been linked to benefits including improved self-awareness, social connection and emotional regulation, while lowering levels of distress, anxiety and even pain scores.
In a study published this week in the Journal of Mental Health, we found art therapy was associated with positive outcomes for children and adolescents in a hospital-based mental health unit.
An option for those who can’t find the words
While a person’s engagement in talk therapies may sometimes be affected by the nature of their illness, verbal reflection is optional in art therapy.
Where possible, after finishing an artwork, a person can explore the meaning of their work with the art therapist, translating unspoken symbolic material into verbal reflection.
However, as the talking component is less central to the therapeutic process, art therapy is an accessible option for people who may not be able to find the words to describe their experiences.
Art therapy has supported improved mental health outcomes for people who have experienced trauma, people with eating disorders, schizophrenia and dementia, as well as children with autism.
Art therapy has also been linked to improved outcomes for people with a range of physical health conditions. These include lower levels of anxiety, depression and fatigue among people with cancer, enhanced psychological stability for patients with heart disease, and improved social connection among people who have experienced a traumatic brain injury.
Art therapy has been associated with improved mood and anxiety levels for patients in hospital, and lower pain, tiredness and depression among palliative care patients.
Studies suggest art therapy could support people with a range of health conditions. mojo cp/Shutterstock Our research
Mental ill-health, including among children and young people, presents a major challenge for our society. While most care takes place in the community, a small proportion of young people require care in hospital to ensure their safety.
In this environment, practices that place even greater restriction, such as seclusion or physical restraint, may be used briefly as a last resort to ensure immediate physical safety. However, these “restrictive practices” are associated with negative effects such as post-traumatic stress for patients and health professionals.
Worryingly, staff report a lack of alternatives to keep patients safe. However, the elimination of restrictive practices is a major aim of mental health services in Australia and internationally.
Our research looked at more than six years of data from a child and adolescent mental health hospital ward in Australia. We sought to determine whether there was a reduction in restrictive practices during the periods when art therapy was offered on the unit, compared to times when it was absent.
We found a clear association between the provision of art therapy and reduced frequency of seclusion, physical restraint and injection of sedatives on the unit.
We don’t know the precise reason for this. However, art therapy may have lessened levels of severe distress among patients, thereby reducing the risk they would harm themselves or others, and the likelihood of staff using restrictive practices to prevent this.
This artwork was described by the young person who made it as a dead tree with new growth, representing a sense of hope emerging as they started to move towards their recovery. Author provided That said, hospital admission involves multiple therapeutic interventions including talk-based therapies and medications. Confirming the effect of a therapeutic intervention requires controlled clinical trials where people are randomly assigned one treatment or another.
Although ours was an observational study, randomised controlled trials support the benefits of art therapy in youth mental health services. For instance, a 2011 hospital-based study showed reduced symptoms of post-traumatic stress disorder among adolescents randomised to trauma-focussed art therapy compared to a “control” arts and crafts group.
Artwork made by a young person during an art therapy session in an in-patient mental health unit. Author provided What do young people think?
In previous research we found art therapy was considered by adolescents in hospital-based mental health care to be the most helpful group therapy intervention compared to other talk-based therapy groups and creative activities.
In research not yet published, we’re speaking with young people to better understand their experiences of art therapy, and why it might reduce distress. One young person accessing art therapy in an acute mental health service shared:
[Art therapy] is a way of sort of letting out your emotions in a way that doesn’t involve being judged […] It let me release a lot of stuff that was bottling up and stuff that I couldn’t explain through words.
A promising area
The burgeoning research showing the benefits of art therapy for both physical and especially mental health highlights the value of creative and innovative approaches to treatment in health care.
There are opportunities to expand art therapy services in a range of health-care settings. Doing so would enable greater access to art therapy for people with a variety of physical and mental health conditions.
Sarah Versitano, Academic, Master of Art Therapy Program, Western Sydney University and Iain Perkes, Senior Lecturer, Child and Adolescent Psychiatry, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Avoiding/Managing Osteoarthritis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Avoiding/Managing Osteoarthritis
Arthritis is the umbrella term for a cluster of joint diseases involving inflammation of the joints, hence “arthr-” (joint) “-itis” (suffix used to denote inflammation).
Inflammatory vs Non-Inflammatory Arthritis
Arthritis is broadly divided into inflammatory arthritis and non-inflammatory arthritis.
Some forms, such as rheumatoid arthritis, are of the inflammatory kind. We wrote about that previously:
See: Avoiding/Managing Rheumatoid Arthritis
You may be wondering: how does one get non-inflammatory inflammation of the joints?
The answer is, in “non-inflammatory” arthritis, such as osteoarthritis, the damage comes first (by general wear-and-tear) and inflammation generally follows as part of the symptoms, rather than the cause.
So the name can be a little confusing. In the case of osteo- and other “non-inflammatory” forms of arthritis, you definitely still want to keep your inflammation at bay as best you can; it’s just not the prime focus.
So, what should we focus on?
First and foremost: avoiding wear-and-tear if possible. Naturally, we all must live our lives, and sometimes that means taking a few knocks, and definitely it means using our joints. An unused joint would suffer just as much as an abused one. But, we can take care of our joints!
We wrote on that previously, too:
See: How To Really Look After Your Joints
New osteoarthritis medication (hot off the press!)
At 10almonds, we try to keep on top of new developments, and here’s a shiny new one from this month:
- Methotrexate to treat hand osteoarthritis with synovitis (12th Oct, clinical trial)
- New research has found an existing drug could help many people with painful hand osteoarthritis (24th Oct, pop-science article about the above, but still written by one of the study authors!)
Note also that Dr. Flavia Cicuttini there talks about what we talked about above—that calling it non-inflammatory arthritis is a little misleading, as the inflammation still occurs.
And finally…
You might consider other lifestyle adjustments to manage your symptoms. These include:
- Exercise—gently, though!
- Rest—while keeping mobility going.
- Mobility aids—if it helps, it helps.
- Go easy on the use of braces, splints, etc—these can offer short-term relief, but at a long term cost of loss of mobility.
- Only you can decide where to draw the line when it comes to that trade-off.
You can also check out our previous article:
See: Managing Chronic Pain (Realistically!)
Take good care of yourself!
Share This Post
-
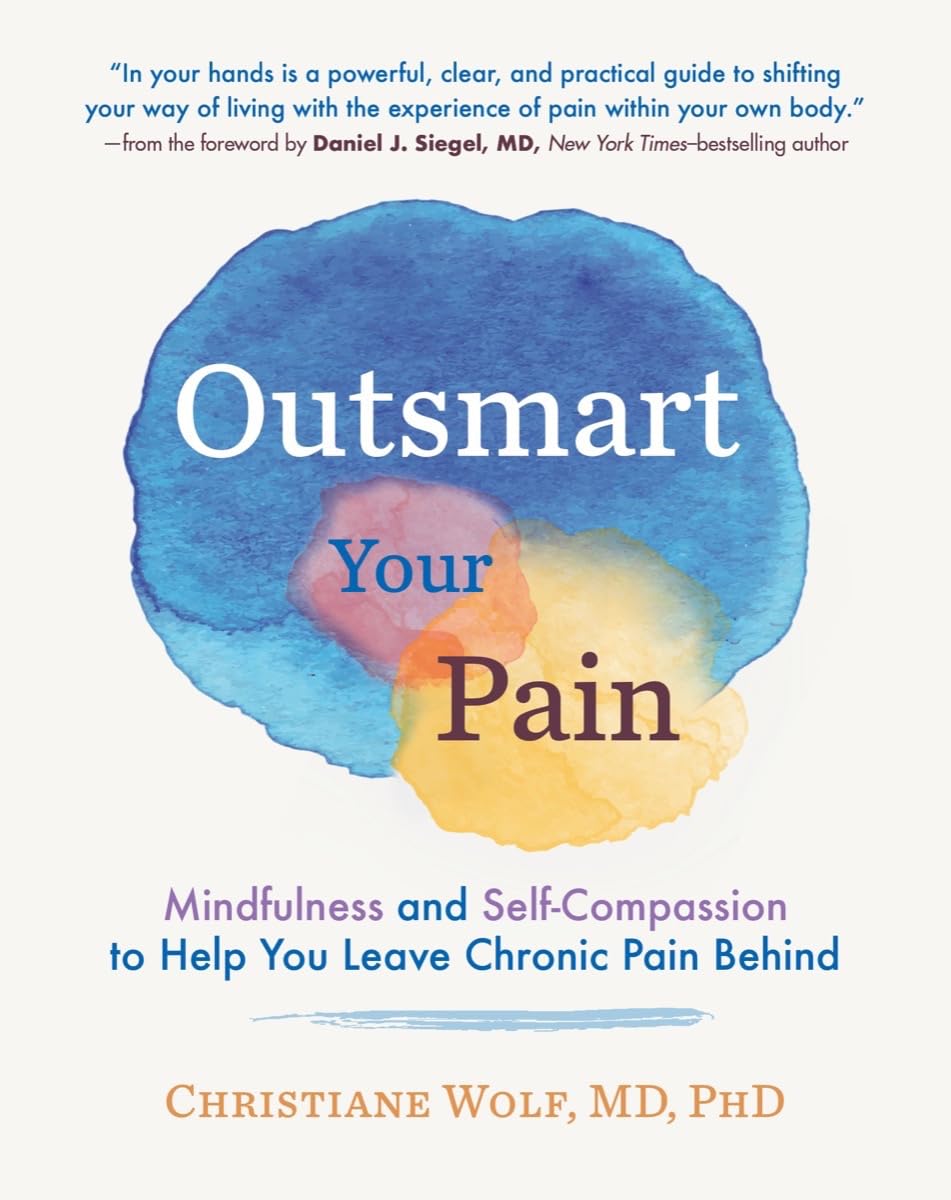
Outsmart Your Pain – by Dr. Christiane Wolf
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Wolf is a physician turned mindfulness teacher. As such, and holding an MD as well as a PhD in psychosomatic medicine, she knows her stuff.
A lot of what she teaches is mindfulness-based stress reduction (MBSR), but this book is much more specific than that. It doesn’t promise you won’t continue to experience pain—in all likelihood you will—but it does change the relationship with pain, and this greatly lessens the suffering and misery that comes with it.
For many, the most distressing thing about pain is not the sensation itself, but how crippling it can be—getting in the way of life, preventing enjoyment of other things, and making every day a constant ongoing exhausting battle… And every night, a “how much rest am I actually going to be able to get, and in what condition will I wake up, and how will I get through tomorrow?” stress-fest.
Dr. Wolf helps the reader to navigate through all these challenges and more; minimize the stress, maximize the moments of respite, and keep pain’s interference with life to a minimum. Each chapter addresses different psychological aspects of chronic pain management, and each comes with specific mindfulness meditations to explore the new ideas learned.
The style is personal and profound, while coming from a place of deep professional understanding as well as compassion.
Bottom line: if you’ve been looking for a life-ring to help you reclaim your life, this one could be it; we wholeheartedly recommend it.
Click here to check out Outsmart Your Pain, and recover the beauty and joy of life!
Share This Post
Related Posts
-
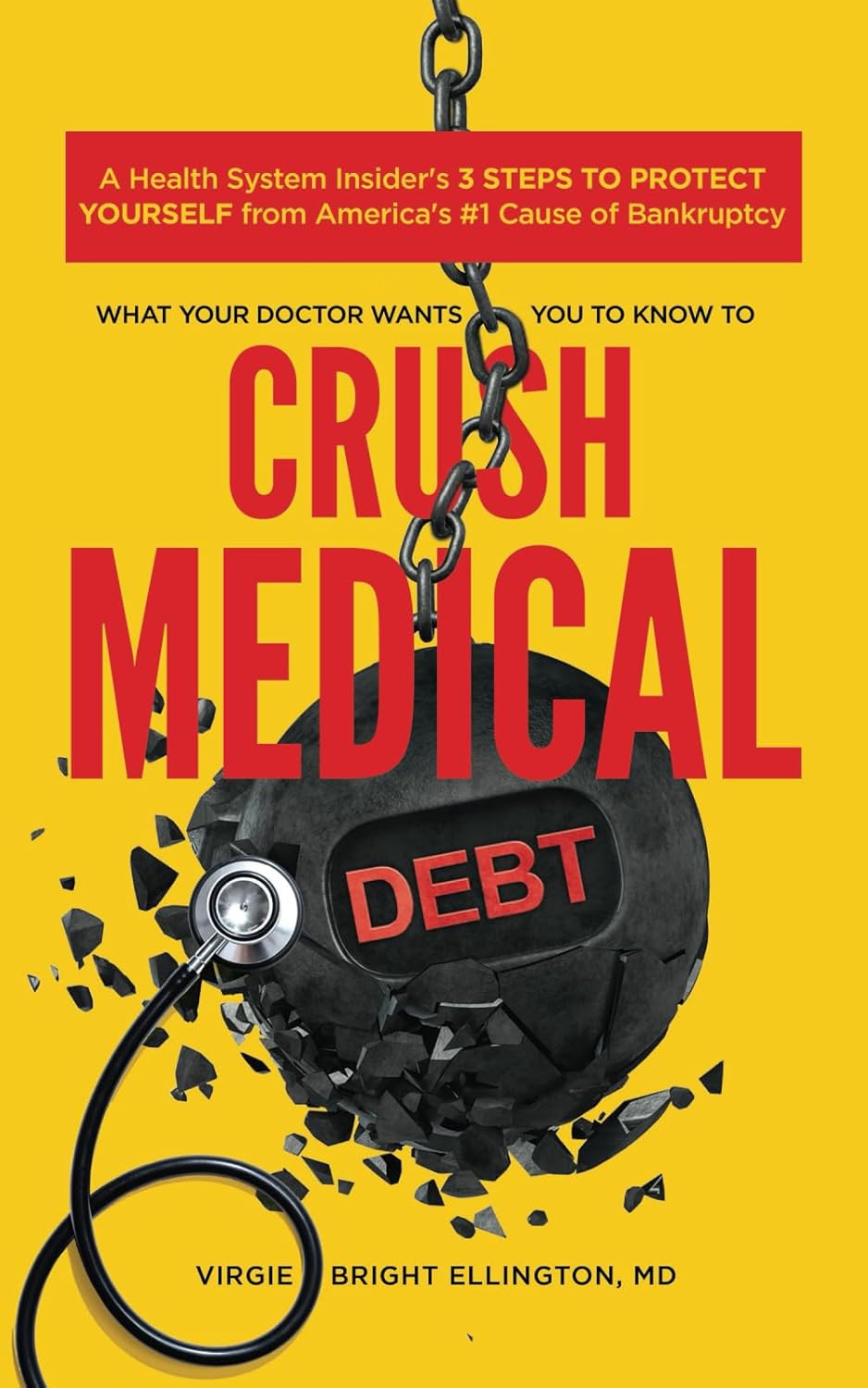
What Your Doctor Wants You to Know to Crush Medical Debt – by Dr. Virgie Ellington
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First things first: this one’s really only of relevance to people living in the US. That’s most of our readership, but if it’s not you, then apologies, this one won’t be of interest.
For the US Americans, though, Dr. Ellington starts strong with “you got a bill—now get the right bill”, and then gives a step-by-step process for finding the mistakes in your medical bills, fixing them, dealing with insurers who do not want to live up to their part of the bargain, and how to minimize what you need to pay, when you actually arrive at your final bill.
The biggest strength of this book is the wealth of insider knowledge (the author has worked as a primary care physician as well as as a health insurance executive), and while this information won’t stay current forever, its relatively recent publication date (2022) means that little has changed since then, and once you’re up to speed with how things are now, it’ll be easy to roll with whatever changes may come in the future.
Bottom line: if you’re living in the US and would like to not be ripped off as badly as possible when it comes to healthcare costs, this book is a very small, very powerful, investment.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Managing Your Mortality
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Planning Is a Matter of Life and Death
Barring medical marvels as yet unrevealed, we are all going to die. We try to keep ourselves and our loved ones in good health, but it’s important to be prepared for the eventuality of death.
While this is not a cheerful topic, considering these things in advance can help us manage a very difficult thing, when the time comes.
We’ve put this under “Psychology Sunday” as it pertains to processing our own mortality, and managing our own experiences and the subsequent grief that our death may invoke in our loved ones.
We’ll also be looking at some of the medical considerations around end-of-life care, though.
Organizational considerations
It’s generally considered good to make preparations in advance. Write (or update) a Will, tie up any loose ends, decide on funerary preferences, perhaps even make arrangements with pre-funding. Life insurance, something difficult to get at a good rate towards the likely end of one’s life, is better sorted out sooner rather than later, too.
Beyond bureaucracy
What’s important to you, to have done before you die? It could be a bucket list, or it could just be to finish writing that book. It could be to heal a family rift, or to tell someone how you feel.
It could be more general, less concrete: perhaps to spend more time with your family, or to engage more with a spiritual practice that’s important to you.
Perhaps you want to do what you can to offset the grief of those you’ll leave behind; to make sure there are happy memories, or to make any requests of how they might remember you.
Lest this latter seem selfish: after a loved one dies, those who are left behind are often given to wonder: what would they have wanted? If you tell them now, they’ll know, and can be comforted and reassured by that.
This could range from “bright colors at my funeral, please” to “you have my blessing to remarry if you want to” to “I will now tell you the secret recipe for my famous bouillabaisse, for you to pass down in turn”.
End-of-life care
Increasingly few people die at home.
- Sometimes it will be a matter of fighting tooth-and-nail to beat a said-to-be-terminal illness, and thus expiring in hospital after a long battle.
- Sometimes it will be a matter of gradually winding down in a nursing home, receiving medical support to the end.
- Sometimes, on the other hand, people will prefer to return home, and do so.
Whatever your preferences, planning for them in advance is sensible—especially as money may be a factor later.
Not to go too much back to bureaucracy, but you might also want to consider a Living Will, to be enacted in the case that cognitive decline means you cannot advocate for yourself later.
Laws vary from place to place, so you’ll want to discuss this with a lawyer, but to give an idea of the kinds of things to consider:
National Institute on Aging: Preparing A Living Will
Palliative care
Palliative care is a subcategory of end-of-life care, and is what occurs when no further attempts are made to extend life, and instead, the only remaining goal is to reduce suffering.
In the case of some diseases including cancer, this may mean coming off treatments that have unpleasant side-effects, and retaining—or commencing—pain-relief treatments that may, as a side-effect, shorten life.
Euthanasia
Legality of euthanasia varies from place to place, and in some times and places, palliative care itself has been considered a form of “passive euthanasia”, that is to say, not taking an active step to end life, but abstaining from a treatment that prolongs it.
Clearer forms of passive euthanasia include stopping taking a medication without which one categorically will die, or turning off a life support machine.
Active euthanasia, taking a positive action to end life, is legal in some places and the means varies, but an overdose of barbiturates is an example; one goes to sleep and does not wake up.
It’s not the only method, though; options include benzodiazepines, and opioids, amongst others:
Efficacy and safety of drugs used for assisted dying
Unspoken euthanasia
An important thing to be aware of (whatever your views on euthanasia) is the principle of double-effect… And how it comes to play in palliative care more often than most people think.
Say a person is dying of cancer. They opt for palliative care; they desist in any further cancer treatments, and take medication for the pain. Morphine is common. Morphine also shortens life.
It’s common for such a patient to have a degree of control over their own medication, however, after a certain point, they will no longer be in sufficient condition to do so.
After this point, it is very common for caregivers (be they medical professionals or family members) to give more morphine—for the purpose of reducing suffering, of course, not to kill them.
In practical terms, this often means that the patient will die quite promptly afterwards. This is one of the reasons why, after sometimes a long-drawn-out period of “this person is dying”, healthcare workers can be very accurate about “it’s going to be in the next couple of days”.
The take-away from this section is: if you would like for this to not happen to you or your loved one, you need to be aware of this practice in advance, because while it’s not the kind of thing that tends to make its way into written hospital/hospice policies, it is very widespread and normalized in the industry on a human level.
Further reading: Goods, causes and intentions: problems with applying the doctrine of double effect to palliative sedation
One last thing…
Planning around our own mortality is never a task that seems pressing, until it’s too late. We recommend doing it anyway, without putting it off, because we can never know what’s around the corner.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Replacing Sugar: Top 10 Anti-Inflammatory Sweet Foods
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For those with a sweet tooth, it can be challenging to indulge one’s desires while also avoiding inflammation. Happily, Dr. Jia-Yia Lui has scientific insights to share!
Dr. Liu’s Top 10
We’ll not keep them a mystery; they are:
- Grapes
- Goji berries
- Barberries
- Persimmons
- Longans
- Lychees
- Raisins¹
- Applesauce²
- Plums³
- Dates
¹Yes, these are technically also grapes, but there are enough differences that Dr. Liu tackles them separately.
²It makes a difference how it’s made, though.
³And dried plums, in other words, prunes.For more details on all of these, plus their extra benefits and relevant considerations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- How to Prevent (or Reduce) Inflammation
- The Not-So-Sweet Science Of Sugar Addiction
- 10 Ways To Balance Blood Sugars
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: