Vegan Eager for Milk Alternatives
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Q: Thanks for the info about dairy. As a vegan, I look forward to a future comment about milk alternatives
Thanks for bringing it up! What we research and write about is heavily driven by subscriber feedback, so notes like this really help us know there’s an audience for a given topic!
We’ll do a main feature on it, to do it justice. Watch out for Research Review Monday!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

The Most Anti Aging Exercise
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve referenced this (excellent) video before, but never actually put it under the spotlight in one of these features, so here we go!
Deep squats
It’s about deep squats, also called Slav squats, Asian squats, sitting squats, resting squats, or various other names. However, fear not; you don’t need to be Slavic or Asian to do it; you just need to practice.
As for why this is called “anti-aging”, by the way, it’s because being able to get up off the ground is one of the main tests of age-related mobility decline, and if you can deep-squat comfortably, then you can do that easily. And so long as you continue being able to deep-squat comfortably, you’ll continue to be able to get up off the ground easily too, because you have the strength in the right muscles, as well as the suppleness, comfort with range of motion, and balance (those stabilizing muscles are used constantly in a deep squat, whereas Western lifestyle sitting leaves those muscles very neglected and thus atrophied).
Epidemiological note: chairs, couches, and assorted modern conveniences reduce the need for squatting in daily life, leading to stiffness in joints, muscles, tendons, and ligaments. Many adults in developed countries struggle with deep squats due to lack of use, not aging. Which is a problem, because a lack of full range of motion in joints causes wear and tear, leading to chronic pain and degenerative joint diseases. People in countries where squatting is a common resting position have lower incidences of osteoarthritis, for example—contrary to what some might expect, squatting does not harm joints but rather protects them from arthritis and knee pain. Strengthening leg muscles through squatting can alleviate knee pain, whereas knee pain is often worsened by inactivity.
Notwithstanding the thumbnail, which is showing an interim position, one’s feet should be flat on the ground, by the way, and one’s butt should be nearby, just a few inches off the ground (in other words, the position that we see her in for most of this video).
Troubleshooting: if you’re accustomed to sitting in chairs a lot, then this may be uncomfortable at first. Zuzka advises us to go gently, and/but gradually increase our range of motion and (equally importantly) duration in the resting position.
You can use a wall or doorway to partially support you, at first, if you struggle with mobility or balance. Just try to gradually use it less, until you’re comfortable deep-squatting with no support.
Since this is not an intrinsically very exciting exercise, once you build up the duration for which you’re comfortable deep-squatting, it can be good to get in the habit of “sitting” this way (i.e. deep squatting, still butt-off-the-floor, but doing the job of sitting) while doing other things such as working (if you have an appropriate work set-up for that*), reading, or watching TV.
*this is probably easiest with a laptop placed on an object/surface of appropriate height, such as a coffee table or such. As a bonus, having your hands in front of you while working will also bring your center of gravity forwards a bit, making the position easier and more comfortable to maintain. This writer (hi, it’s me) prefers her standing desk for work in general, with a nice ergonomic keyboard and all that, but if using a laptop from time to time, then squatting is a very good option.
In terms of working up duration, if you can only manage seconds to start with, that’s fine. Just do a few more seconds each time, until it’s 30, 60, 120, and so on until it’s 5 minutes, 10, 15, and so on.
You can even start that habit-forming while you’re still in the “seconds at a time” stage! You can deep-squat just for some seconds while you:
- pick up something from the floor
- check on something in the oven
- get something out of the bottom of the fridge
…etc!
For more on all this, plus many visual demonstrations including interim exercises to get you there if it’s difficult for you at first, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Mobility For Now & For Later: Train For The Marathon That Is Your Life!
Take care!
Share This Post

Dr. Kim Foster’s Method For Balancing Hormones Naturally
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not just sex hormones, but also hormones like cortisol (the stress hormone), and thyroid hormones (for metabolism regulation) too! The body is most of the time self-regulating when it comes to hormones, but there are things that we can do to help our body look after us correctly.
In short, if we give our body what it needs, it will (usually, barring serious illness!) give us what we need.
Dr. Foster recommends…
Foods:
- Healthy fats (especially avocados and nuts)
- Lean proteins (especially poultry, fish, and legumes)
- Fruits & vegetables (especially colorful ones)
- Probiotics (especially fermented foods like sauerkraut, kimchi, etc)
- Magnesium-rich foods (especially dark leafy greens, nuts, and yes, dark chocolate)
Teas:
- Camomile tea (especially beneficial against cortisol overproduction)
- Nettle tea (especially beneficial for estrogen production)
- Peppermint tea (especially beneficial for gut health, thus indirect hormone benefits)
Stress reduction:
- Breathing exercises (especially mindfulness exercises)
- Yoga (especially combining exercise with stretches)
- Spending time in nature (especially green spaces)
Dr. Foster explains more about all of these things, along with more illustrative examples, so if you can, do enjoy her video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to read more about this topic?
You might like our main feature: What Does “Balance Your Hormones” Even Mean?
Enjoy!
Share This Post

Cold Weather Health Risks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many Are Cold; Few Are Frozen
Many of those of us in the Northern Hemisphere are getting hit with a cold spell around now. How severe that may be depends on more precisely where we are, but it’s affecting a lot of people. So, with apologies to our readers in Australia, we’re going to do a special on that today.
Acute cold is, for most people, good for the health:
A Cold Shower A Day Keeps The Doctor Away?
Persistent cold, not so much. Let’s look at the risks, and what can be done about them…
Hypothermia
It kills. Don’t let it kill you or your loved ones.
And, this is really important: it doesn’t care whether you’re on a mountain or not.
In other words: a lot of people understand (correctly!) that hypothermia is a big risk to hikers, climbers, and the like. But if the heating goes out in your house and the temperature drops for long enough before the heating is fixed, you can get hypothermia there too just the same if you’re not careful.
How cold is too cold? It doesn’t even have to be sub-zero. According to the CDC, temperatures of 4℃ (40℉) can be low enough to cause hypothermia if other factors combine:
CDC | Prevent Hypothermia & Frostbite ← you can also see the list of symptoms to watch out for, there!
Skin health
Not generally an existential risk, but we may as well stay healthy as not!
Cold air often means dry air, so use a moisturizer with an oil base (if you don’t care for fancy beauty products, ordinary coconut oil is top-tier).
Bonus if you do it after a warming bath/shower!
Heart health
Cold has a vasconstricting effect; that is to say, it causes the body’s vasculature to shrink, increasing localized blood pressure. If it’s a cold shower as above, that can be very invigorating. If it’s a week of sub-zero temperatures, it can become a problem.
❝Shoveling a little snow off your sidewalk may not seem like hard work. However, […] combined with the fact that the exposure to cold air can constrict blood vessels throughout the body, you’re asking your heart to do a lot more work in conditions that are diminishing the heart’s ability to function at its best.❞
Source: Snow shoveling, cold temperatures combine for perfect storm of heart health hazards
If you have a heart condition, please do not shovel snow. Let someone else do it, or stay put.
And if you are normally able to exercise safely? Unless you’re sure your heart is in good order, exercising in the warmth, not the cold, seems to be the best bet.
See also: Heart Attack: His & Hers (Be Prepared!) ← can you remember which symptoms are for which sex? If not, now’s a good time to refresh that knowledge.
Immune health
We recently discussed how cold weather indirectly increases the risk of respiratory viral infection:
The Cold Truth About Respiratory Infections
So, now’s the time to be extra on-guard about that.
See also: Beyond Supplements: The Real Immune-Boosters!
Balance
Icy weather increases the risk of falling. If you think “having a fall” is something that happens to other/older people, please remember that there’s a first time for everything. Some tips:
- Walk across icy patches with small steps in a flat-footed fashion like a penguin.
- It may not be glamorous, but neither is going A-over-T and breaking (or even just spraining) things.
- Use a handrail if available, even if you don’t think you need to.
You can also check out our previous article about falling (avoiding falling, minimizing the damage of falling, etc):
Fall Special: Some Fall-Themed Advice
Take care!
Share This Post
- Walk across icy patches with small steps in a flat-footed fashion like a penguin.
Related Posts

‘Free birthing’ and planned home births might sound similar but the risks are very different
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The death of premature twins in Byron Bay in an apparent “wild birth”, or free birth, last week has prompted fresh concerns about giving birth without a midwife or medical assistance.
This follows another case from Victoria this year, where a baby was born in a critical condition following a reported free birth.
It’s unclear how common free birthing is, as data is not collected, but there is some evidence free births increased during the COVID pandemic.
Planned home births also became more popular during the pandemic, as women preferred to stay away from hospitals and wanted their support people with them.
But while free births and home births might sound similar, they are a very different practice, with free births much riskier. So what’s the difference, and why might people opt for a free birth?
What are home births?
Planned home births involve care from midwives, who are registered experts in childbirth, in a woman’s home.
These registered midwives work privately, or are part of around 20 publicly funded home birth programs nationally that are attached to hospitals.
They provide care during the pregnancy, labour and birth, and in the first six weeks following the birth.
The research shows that for women with low risk pregnancies, planned home births attended by competent midwives (with links to a responsive mainstream maternity system) are safe.
Home births result in less intervention than hospital births and women perceive their experience more positively.
What are free births?
A free birth is when a woman chooses to have a baby, usually at home, without a registered health professional such as a midwife or doctor in attendance.
Different terms such as unassisted birth or wild pregnancy or birth are also used to refer to free birth.
The parents may hire an unregulated birth worker or doula to be a support at the birth but they do not have the training or medical equipment needed to manage emergencies.
Women may have limited or no health care antenatally, meaning risk factors such as twins and breech presentations (the baby coming bottom first) are not detected beforehand and given the right kind of specialist care.
Why do some people choose to free birth?
We have been studying the reasons women and their partners choose to free birth for more than a decade. We found a previous traumatic birth and/or feeling coerced into choices that are not what the woman wants were the main drivers for avoiding mainstream maternity care.
Australia’s childbirth intervention rates – for induction or augmentation of labour, episiotomy (cutting the tissue between the vaginal opening and the anus) and caesarean section – are comparatively high.
One in ten women report disrespectful or abusive care in childbirth and some decide to make different choices for future births.
Lack of options for a natural birth and birth choices such as home birth or birth centre birth also played a major role in women’s decision to free birth.
Publicly funded home birth programs have very strict criteria around who can be accepted into the program, excluding many women.
In other countries such as the United Kingdom, Netherlands and New Zealand, publicly funded home births are easier to access.

It can be difficult to access home birth services in Australia.
Ink Drop/ShutterstockOnly around 200 midwives provide private midwifery services for home births nationally. Private midwives are yet to obtain insurance for home births, which means they are risking their livelihoods if something goes wrong and they are sued.
The cost of a home birth with a private midwife is not covered by Medicare and only some health funds rebate some of the cost. This means women can be out of pocket A$6-8,000.
Access to home birth is an even greater issue in rural and remote Australia.
How to make mainstream care more inclusive
Many women feel constrained by their birth choices in Australia. After years of research and listening to thousands of women, it’s clear more can be done to reduce the desire to free birth.
As my co-authors and I outline in our book, Birthing Outside the System: The Canary in the Coal Mine, this can be achieved by:
- making respectful care a reality so women aren’t traumatised and alienated by maternity care and want to engage with it
- supporting midwifery care. Women are seeking more physiological and social ways of birthing, minimising birth interventions, and midwives are the experts in this space
- supporting women’s access to their chosen place of birth and model of care and not limiting choice with high out-of-pocket expenses
- providing more flexible, acceptable options for women experiencing risk factors during pregnancy and/or birth, such as having a previous caesarean birth, having twins or having a baby in breech position. Women experiencing these complications experience pressure to have a caesarean section
- getting the framework right with policies, guidelines, education, research, regulation and professional leadership.
Ensuring women’s rights and choices are informed and respected means they’re less likely to feel they’re left with no other option.

Hannah Dahlen, Professor of Midwifery, Associate Dean Research and HDR, Midwifery Discipline Leader, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

More research shows COVID-19 vaccines are safe for young adults
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- Myocarditis, or inflammation of the heart muscle, is most commonly caused by a viral infection like COVID-19, not by vaccination.
- In line with previous research, a recent CDC study found no association between COVID-19 vaccination and sudden cardiac death in previously healthy young people.
- A COVID-19 infection is much more likely to cause inflammation of the heart muscle than a COVID-19 vaccine, and those cases are typically more severe.
Since the approval of the first COVID-19 vaccines, anti-vaccine advocates have raised concerns about heart muscle inflammation, also called myocarditis, after vaccination to suggest that vaccines are unsafe. They’ve also used concerns about myocarditis to spread false claims that vaccines cause sudden deaths, which is not true.
Research has consistently shown that cases of myocarditis after vaccination are extremely rare and usually mild, and a new study from the CDC found no association between sudden cardiac death and COVID-19 vaccination in young adults.
Read on to learn more about myocarditis and what the latest research says about COVID-19 vaccine safety.
What is myocarditis?
Myocarditis is inflammation of the myocardium, or the middle muscular layer of the heart wall. This inflammation weakens the heart’s ability to pump blood. Symptoms may include fatigue, shortness of breath, chest pain, rapid or irregular heartbeat, and flu-like symptoms.
Myocarditis may resolve on its own. In rare cases, it may lead to stroke, heart failure, heart attack, or death.
What causes myocarditis?
Myocarditis is typically caused by a viral infection like COVID-19. Bacteria, parasites, fungi, chemicals, and certain medications can also cause myocarditis.
In very rare cases, some people develop myocarditis after receiving a COVID-19 vaccine, but these cases are usually mild and resolve on their own. In contrast, a COVID-19 infection is much more likely to cause myocarditis, and those cases are typically more severe.
Staying up to date on vaccines reduces your risk of developing myocarditis from a COVID-19 infection.
Are COVID-19 vaccines safe for young people?
Yes. COVID-19 vaccines have been rigorously tested and monitored over the past three years and have been determined to be safe for everyone 6 months and older. A recent CDC study found no association between COVID-19 vaccination and sudden cardiac death in previously healthy young adults.
The benefits of vaccination outweigh any potential risks. Staying up to date on COVID-19 vaccines reduces your risk of severe illness, hospitalization, death, long COVID, and COVID-19-related complications, such as myocarditis.
The CDC recommends people 65 and older and immunocompromised people receive an additional dose of the updated COVID-19 vaccine this spring—if at least four months have passed since they received a COVID-19 vaccine.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.

Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

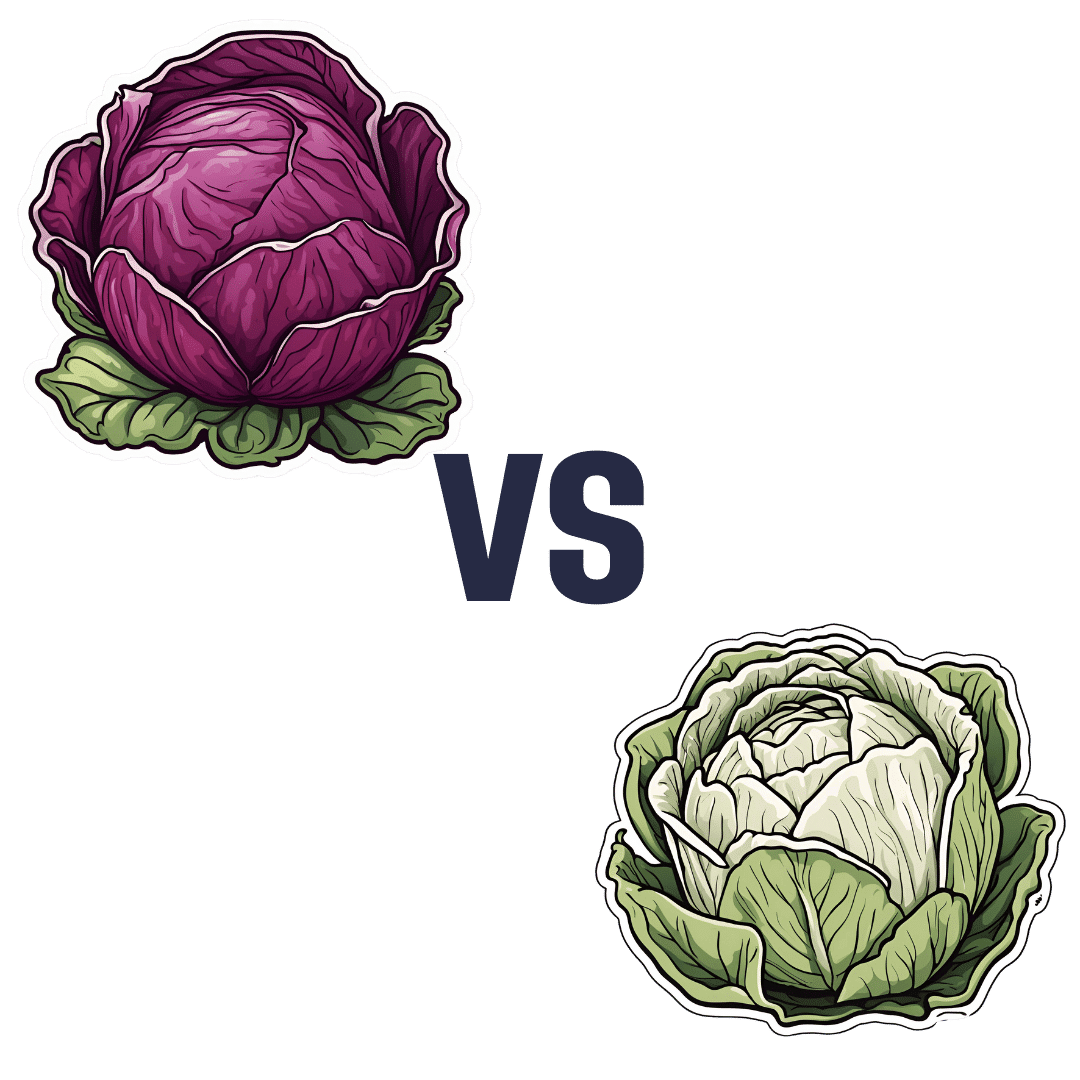
Red Cabbage vs White Cabbage – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing red cabbage to white cabbage, we picked the red.
Why?
Perhaps you guessed this one, based on the “darker and/or more colorful foods are usually more nutritionally dense” dictum. That’s not always true, by the way, but it is a good rule of thumb and it is correct here. In the case of cabbages, each type is a nutritional powerhouse, but red does beat white:
In terms of macros, they’re quite comparable. They’re both >90% water with just enough other stuff (carbs, fiber, protein) to hold them together, and the “other stuff” in question is quite similarly proportioned in both cases. Within the carbs, even the sugar breakdown is similar. There are slight differences, but the differences are not only tiny, but also they balance out in any case.
When it comes to vitamins, as you might expect, the colorful red cabbage does better with more of vitamins A, B1, B2, B3, B6, C, and choline, while white has more of vitamins B5, B9, E, and K. So, a 7:4 win for red.
In the category of minerals, it’s even more polarized; red cabbage has more calcium, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. On the other hand, white contains a tiny amount more copper.
In short, both are great (red just makes white look bad by standing next to it, but honestly, white has lots of all those same things too, just not quite as much as red), and this writer will continue to use white when making her favorite shchi, but if you’re looking for the most nutritionally dense option, it’s red.
Want to learn more?
You might like to read:
Enjoy Bitter Foods For Your Heart & Brain
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: