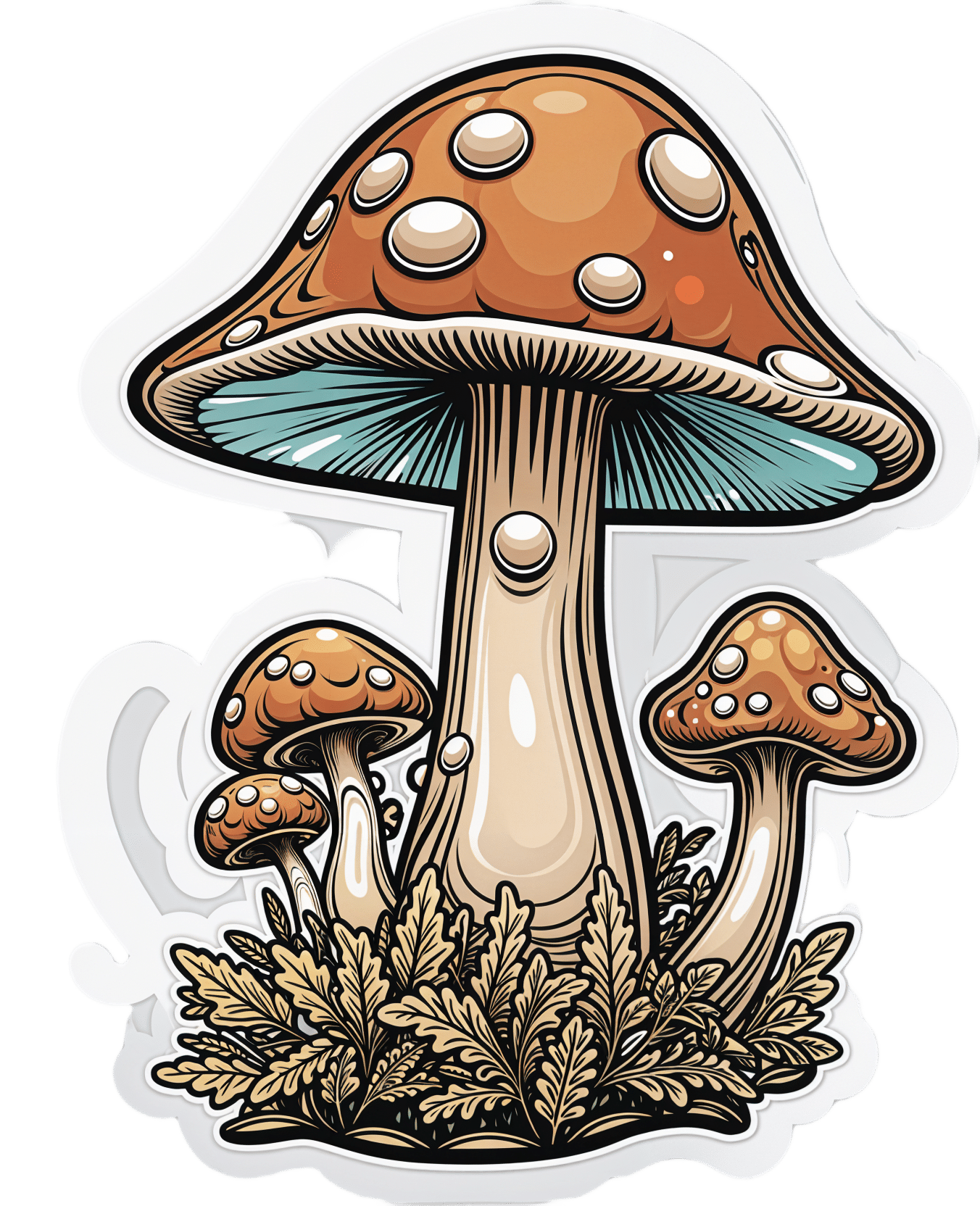
Magic mushrooms may one day treat anorexia, but not just yet
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Anorexia nervosa is a severe mental health disorder where people fear weight gain. Those with the disorder have distorted body image and hold rigid beliefs their body is too big. They typically manage this through restricted eating, leading to the serious medical consequences of malnutrition.
Anorexia has one of the highest death rates of any mental illness. Yet there are currently no effective drug treatments and the outcomes of psychotherapy (talk therapy) are poor. So we’re desperately in need of new and improved treatments.
Psilocybin, commonly known as magic mushrooms, is one such novel treatment. But while it shows early promise, you won’t see it used in clinical practice just yet – more research is needed to test if it’s safe and effective.

What does treatment involve?
The treatment involves the patient taking a dose of psilocybin in a safe environment, which is usually a specifically set up clinic. The patient undergoes preparation therapy before the dosing session and integration therapy after.
Psilocybin, extracted from mushrooms, is a psychedelic, which means it can produce altered thinking, sense of time and emotions, and can often result in hallucinations. It also has the potential to shift patients out of their rigid thinking patterns.
Psilocybin is not administered alone but instead with combined structured psychotherapy sessions to help the patient make sense of their experiences and the changes to their thinking. This is an important part of the treatment.
What does the research show?
Research has shown improved effects of psilocybin-assisted psychotherapy after one or two dosing sessions, a couple of weeks apart. Most research to date has targeted depression.
Psilocybin has been found to increase cognitive flexibility – our ability to adjust our thinking patterns according to changing environments or demands. This is one of the ways researchers believe psilocybin might improve symptoms for conditions such as depression and alcohol use disorder, which are marked by rigid thinking styles.
People with anorexia similarly struggle with rigid thinking patterns. So researchers and clinicians have recently turned their attention to anorexia.
In 2023, a small pilot study of ten women with anorexia was published in the journal Nature Medicine. It showed psilocybin-assisted psychotherapy (with 25mg of psilocybin) was safe and acceptable. There were no significant side effects and participants reported having valuable experiences.
Although the trial was not a formal efficacy trial, 40% of the patients did have significant drops in their eating disorder behaviour.
However, the trial only had one dosing session and no long-term follow up, so further research is needed.

A recent animal study using rats examined whether rigid thinking could be improved in rats when given psilocybin. After the psilocybin, rats gained weight and had more flexible thinking (using a reversal learning task).
These positive changes were related to the serotonin neurotransmitter system, which regulates mood, behaviour and satiety (feeling full).
Brain imaging studies in humans show serotonin disturbances in people with anorexia. Psilocybin-assisted psychotherapy is showing promise at modifying the serotonin disturbances and cognitive inflexibility that have been shown to be problematic in anorexia.
Research with animals can provide unique insights into the brain which can sometimes not be investigated in living humans. But animal models can never truly mimic human behaviour and the complex nature of chronic mental health conditions.
What’s next for research?
Further clinical trials in humans are very much needed – and are underway from a research team at the University of Sydney and ours at Swinburne.
Our trial will involve an initial 5mg dose followed by two subsequent doses of 25mg, several weeks apart. An initial low dose aims to help participants prepare for what is likely to be a new and somewhat unpredictable experience.
Our trial will examine the usefulness of providing psychotherapy that directly addresses body image disturbance. We are also investigating if including a family member or close friend in the treatment increases support for their loved one.

Data from other mental health conditions has suggested that not everyone sees benefits, with some people having bad trips and a deterioration in their mental health. So this treatment won’t be for everyone. It’s important to work out who is most likely to respond and under what conditions.
New trials and those underway will be critical in understanding whether psilocybin-assisted psychotherapy is a safe and effective treatment for anorexia, and the optimal conditions to improve the patient’s response. But we are some way off from seeing this treatment in the clinic. One of the big issues being the cost of this intervention and how this will be funded.
Susan Rossell, Director Clinical Trials and Professor Cognitive Neuropsychiatry Centre for Mental Health and Brain Sciences, Swinburne University of Technology and Claire Finkelstein, Clinical Psychologist and PhD candidate, Swinburne University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Quinoa vs Couscous – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing quinoa to couscous, we picked the quinoa.
Why?
Firstly, quinoa is the least processed by far. Couscous, even if wholewheat, has by necessity been processed to make what is more or less the same general “stuff” as pasta. Now, the degree to which something has or has not been processed is a common indicator of healthiness, but not necessarily declarative. There are some processed foods that are healthy (e.g. many fermented products) and there are some unprocessed plant or animal products that can kill you (e.g. red meat’s health risks, or the wrong mushrooms). But in this case—quinoa vs couscous—it’s all borne out pretty much as expected.
For the purposes of the following comparisons, we’ll be looking at uncooked/dry weights.
In terms of macros, quinoa has a little more protein, slightly lower carbs, and several times the fiber. The amino acids making up quinoa’s protein are also much more varied.
In the category of vitamins, quinoa has more of vitamins A, B1, B2, B6, and B9, while couscous boasts a little more of vitamins B3 and B5. Given the respective margins of difference, as well as the total vitamins contained, this category is an easy win for quinoa.
When it comes to minerals, this one’s not even more clear. Quinoa has a lot more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. Couscous, meanwhile has more of just one mineral: sodium. So, maybe not one you want more of.
All in all, today’s is an easy pick: quinoa!
Want to learn more?
You might like to read:
- Carbohydrate Mythbusting: Should You Go Light Or Heavy On Carbs?
- What’s The Real Deal With The Paleo Diet?
- Gluten Mythbusting: What’s The Truth? ← we didn’t mention it above, but couscous is by default gluten-free, and couscous, being made of wheat, is by default not gluten-free, which may be another reason for some to choose quinoa
Take care!
Share This Post
-
Sesame Chocolate Fudge
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’d like a sweet treat without skyrocketing your blood sugars with, well, rocket fuel… Today’s recipe can help you enjoy a taste of decadence that’s not bad for your blood sugars, and good for your heart and brain.
You will need
- ½ cup sesame seeds
- ¼ cup cocoa powder
- 3 tbsp maple syrup
- 1 tbsp coconut oil (plus a little extra for the pan)
Method
(we suggest you read everything at least once before doing anything)
1) Lightly toast the sesame seeds in a pan until golden brown. Remove from the heat and allow to cool.
2) Put them in a food processor, and blend on full speed until they start to form a dough-like mixture. This may take a few minutes, so be patient. We recommend doing it in 30-second sessions with a 30-second rest between them, to avoiding overheating the motor.
3) Add the rest of the ingredients and blend to combine thoroughly—this should go easily now and only take 10 seconds or so, but judge it by eye.
4) Grease an 8″ square baking tin with a little coconut oil, and add the mixture, patting it down to fill the tin, making sure it is well-compressed.
5) Allow to chill in the fridge for 6 hours, until firm.
6) Turn the fudge out onto a chopping board, and cut into the size squares you want. Serve, or store in the fridge until ready to serve.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Tasty Polyphenols For Your Heart & Brain
- Cacao vs Carob – Which is Healthier?
- Can Saturated Fats Be Healthy?
Take care!
Share This Post
-
Celery vs Chard – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to chard, we picked the chard.
Why?
In terms of macros, chard has more fiber, carbs, and protein, making it the more nutrient-dense option and thus the winner of the macros category.
In the category of vitamins, celery has more of vitamins B5 and B9, while chard has more of vitamins A, B1, B2, B3, B6, C, E, K, and choline—another win for chard.
When it comes to minerals, celery is not higher in any minerals, while chard has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. One more very clear win for chard!
Looking at polyphenols, celery has very little to boast, about 3mg/100g furanocoumarins and nothing else, while chard has an impressive array of polyphenols, with 9mg/100g kaempferol and 7.5mg/100g quercetin atop the list of 12 polyphenols. Yet another win for chard.
Adding up the sections is not difficult arithmetic today: chard sweeps every category. But by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Dr. Greger’s Daily Dozen ← the “dozen” in question includes getting a good amount of of leafy greens per day
Enjoy!
Share This Post
Related Posts
-
The Brain-Gut Highway: A Two-Way Street
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Brain-Gut Two-Way Highway
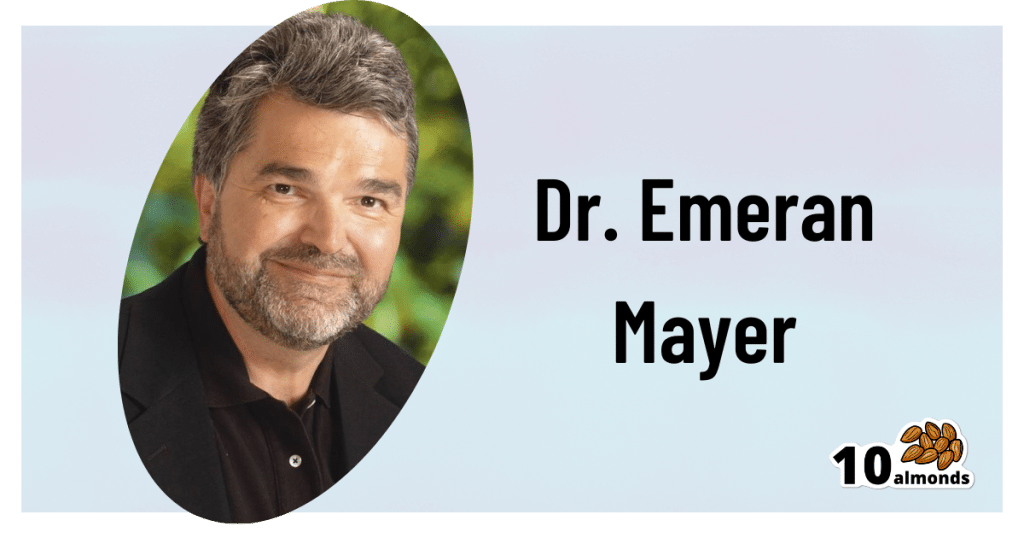
This is Dr. Emeran Mayer. He has the rather niche dual specialty of being a gastroenterologist and a neurologist. He has published over 353 peer reviewed scientific articles, and he’s a professor in the Departments of Medicine, Physiology, and Psychiatry at UCLA. Much of his work has been pioneering medical research into gut-brain interactions.
We know the brain and gut are connected. What else does he want us to know?
First, that it is a two-way interaction. It’s about 90% “gut tells the brain things”, but it’s also 10% “brain tells the gut things”, and that 10% can make more like a 20% difference, if for example we look at the swing between “brain using that 10% communication to tell gut to do things worse” or “brain using that 10% communication to tell gut to do things better”, vs the midpoint null hypothesis of “what the gut would be doing with no direction from the brain”.
For example, if we are experiencing unmanaged chronic stress, that is going to tell our gut to do things that had an evolutionary advantage 20,000–200,000 years ago. Those things will not help us now. We do not need cortisol highs and adrenal dumping because we ate a piece of bread while stressed.
Read more (by Dr. Mayer): The Stress That Evolution Has Not Prepared Us For
With this in mind, if we want to look after our gut, then we can start before we even put anything in our mouths. Dr. Mayer recommends managing stress, anxiety, and depression from the head downwards as well as from the gut upwards.
Here’s what we at 10almonds have written previously on how to manage those things:
- No-Frills, Evidence-Based Mindfulness
- How To Set Anxiety Aside
- The Mental Health First-Aid You’ll Hopefully Never Need
Do eat for gut health! Yes, even if…
Unsurprisingly, Dr. Mayer advocates for a gut-friendly, anti-inflammatory diet. We’ve written about these things before:
…but there’s just one problem:
For some people, such as with IBS, Crohn’s, and colitis, the Mediterranean diet that we (10almonds and Dr. Mayer) generally advocate for, is inaccessible. If you (if you have those conditions) eat as we describe, a combination of the fiber in many vegetables and the FODMAPs* in many fruits, will give you a very bad time indeed.
*Fermentable Oligo-, Di-, Monosaccharides And Polyols
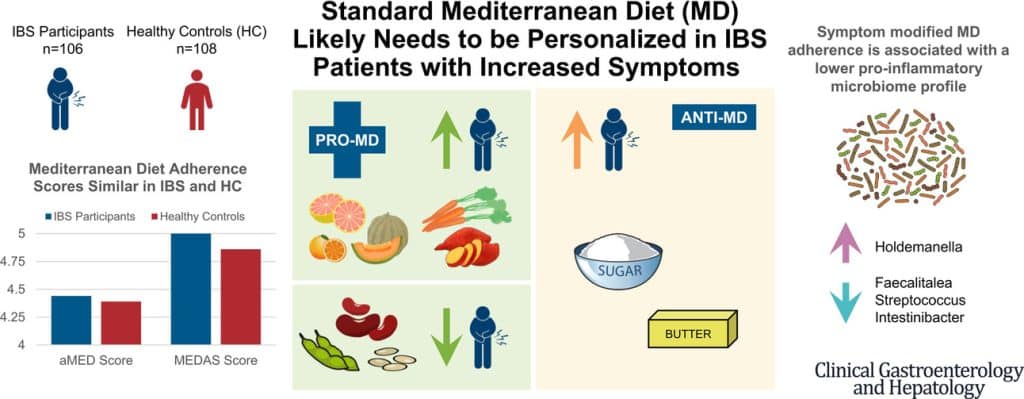
Dr. Mayer has the answer to this riddle, and he’s not just guessing; he and his team did science to it. In a study with hundreds of participants, he measured what happened with adherence (or not) to the Mediterranean diet (or modified Mediterranean diet) (or not), in participants with IBS (or not).
The results and conclusions from that study included:
❝Among IBS participants, a higher consumption of fruits, vegetables, sugar, and butter was associated with a greater severity of IBS symptoms. Multivariate analysis identified several Mediterranean Diet foods to be associated with increased IBS symptoms.
A higher adherence to symptom-modified Mediterranean Diet was associated with a lower abundance of potentially harmful Faecalitalea, Streptococcus, and Intestinibacter, and higher abundance of potentially beneficial Holdemanella from the Firmicutes phylum.
A standard Mediterranean Diet was not associated with IBS symptom severity, although certain Mediterranean Diet foods were associated with increased IBS symptoms. Our study suggests that standard Mediterranean Diet may not be suitable for all patients with IBS and likely needs to be personalized in those with increased symptoms.❞
In graphical form:
And if you’d like to read more about this (along with more details on which specific foods to include or exclude to get these results), you can do so…
- The study itself (full article): The Association Between a Mediterranean Diet and Symptoms of Irritable Bowel Syndrome
- Dr. Mayer’s blog (lay explanation): The Benefits of a Modified Mediterranean Diet for Irritable Bowel Syndrome
Want to know more?
Dr. Mayer offers many resources, including a blog, books, recipes, podcasts, and even a YouTube channel:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Sardinian Cholesterol Paradox
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Broadly speaking, low-density lipoprotein (LDL), or “bad” cholesterol, is generally considered to be… Well… Bad. Specifically because of how it can functionally narrow arteries, causing bits of floating detritus to get stuck in it, narrow it further, and eventually harden into atherosclerotic plaque, at which point it becomes even harder for the body to clear out.
We wrote about the process here: Demystifying Cholesterol
When it comes to cholesterol, the most common lay understanding (especially under a certain age) is “it’s bad”.
A more informed view (and more common after a certain age) is “LDL cholesterol is bad; HDL cholesterol is good”.
A more nuanced view is “LDL cholesterol is established as significantly associated with (and almost certainly a causal factor of) atherosclerotic cardiovascular disease and related mortality in men; in women it is less strongly associated and may or may not be a causal factor”
We wrote more about that, here: Statins: His & Hers? ← despite most research being on men, statins have very different effects (and side effects) for women, often being relatively less useful, and more dangerous. There are exceptions (for some women’s specific profiles they can still be worthwhile), but the trend is certainly troubling.
What, then, of Sardinia?
Sardinia is well-known for being one of the “Supercentenarian Blue Zones”, a place whose inhabitants enjoy (on average, statistically) unusually healthy longevity. These places have been looked to for clues as to how to live the healthiest life.
For example: From Blue To Green: News From The Centenarian Blue Zones
However, researchers recently were investigating life in a region of Sardinia where a lot of people are aged 90+, and followed the health of 168 of them for up to 6 years (because in the case of those who died during that time, obviously the time was less than 6 years).
Note: because this was specifically a Blue Zones study, they only included participants of whom all four grandparents were born within the Blue Zone—so not, for example, looking at the health of someone who just moved there from New York, say.
They collected a lot of interesting data (of course), but what we’re talking about today is that they found that participants with LDL levels above 130 mg/dL had a significantly longer average survival than those with LDL levels below this threshold. Specifically, a 40% lower mortality risk.
This is interesting, because LDL levels ≥130 mg/dL are considered moderate hypercholesterolemia (i.e., the LDL levels are a bit too high).
However, if the same participants had total cholesterol levels over 250mg/dL, they got no extra survival benefits, and very high cholesterol was still linked with shorter survival.
You can read the paper here: The Cholesterol Paradox in Long-Livers from a Sardinia Longevity Hot Spot (Blue Zone)
But before you reach for the butter…
The researchers have several hypotheses about why these results could be so, including:
- The longevity has less to do with LDL itself, and more to do with the diet, with the ratio of grain to olive oil.
- Most of the participants with higher LDL cholesterol were on antihypertensive drugs, which a) will obviously have a cardioprotective effect, and b) means that their heart health is probably enjoying greater scrutiny, and medical scrutiny can also have a protective effect (indeed, that’s the point of it).
- It was also speculated that the locals of that region may have a genetic defense against the harm of moderate hypercholesterolemia, due to historical exposure to malaria meaning that naturally slightly higher cholesterol levels without increased cardiovascular risk may have been naturally selected-for (i.e. those without it were more likely to die of malaria and not pass on their genes).
Thus, it may be that it’s not so applicable more generally. However, it is still reason to at least re-examine how bad LDL cholesterol actually is, and whether for some demographics it could have a protective factor (much like “overweight” BMI is a protective factor for people over 65).
Still, if you’d like to keep on top of your cholesterol levels, check out:
How To Lower Cholesterol Naturally, Without Statins
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Green Coffee Bean Extract: Coffee Benefits Without The Coffee?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Coffee is, on balance, very good for the health in moderation. We wrote about it here:
The Bitter Truth About Coffee (or is it?)
Some quick facts before moving on:
- Coffee is the world’s biggest source of antioxidants
- 65% reduced risk of Alzheimer’s for coffee-drinkers
- 67% reduced risk of type 2 diabetes for coffee-drinkers
- 43% reduced risk of liver cancer for coffee-drinkers
- 53% reduced suicide risk for coffee-drinkers
Those are some compelling statistics!
But what about the caffeine content?
Assuming one doesn’t have a caffeine sensitivity, caffeine is also healthy in moderation—but it is easy to accidentally become dependent on it, so it can be good to take a “tolerance break” once in a while, and then reintroduce it with more modest moderation:
Caffeine: Cognitive Enhancer Or Brain-Wrecker?
We also, for that matter, have discussed its impact on the gut:
Coffee & Your Gut ← surprise, it’s a positive impact
What if I don’t like coffee?
We suspect that, having seen the title of this article, you know what the answer’s going to be here:
Green coffee bean extract is the extract from green (i.e. unroasted) coffee beans. It has one or two advantages over drinking coffee:
- For those who do not like drinking coffee, this supplement sidesteps that neatly
- Roasting coffee beans destroys a lot (sometimes almost all; it depends on the temperature and duration) of their chlorogenic acid, a highly beneficial polyphenol; using unroasted (i.e. green) coffee beans avoids that
See: Role of roasting conditions in the level of chlorogenic acid content in coffee beans
All about GCE and CGA
That’s “green coffee extract” and “chlorogenic acid”, respectively, bearing in mind that the latter is found generously in the former.
As to what it does:
❝CGA is an important and biologically active dietary polyphenol, playing several important and therapeutic roles such as antioxidant activity, antibacterial, hepatoprotective, cardioprotective, anti-inflammatory, antipyretic, neuroprotective, anti-obesity, antiviral, anti-microbial, anti-hypertension, free radicals scavenger and a central nervous system (CNS) stimulator. Furthermore, CGA causes hepatoprotective effects.❞
👆 Those are the things we know for sure that it does. And it may do even more things:
❝In addition, it has been found that CGA could modulate lipid metabolism and glucose in both genetically and healthy metabolic related disorders. It is speculated that CGA can perform crucial roles in lipid and glucose metabolism regulation and thus help to treat many disorders such as hepatic steatosis, cardiovascular disease, diabetes, and obesity as well.❞
Read in full: Chlorogenic acid (CGA): A pharmacological review and call for further research
About lipid metabolism…
- Green coffee extract supplementation significantly reduces serum total cholesterol levels.
- Green coffee extract supplementation significantly reduces serum LDL (“bad” cholesterol) levels.
- Increases in HDL (“good” cholesterol) after green coffee bean extract consumption are significant in green coffee bean extract dosages ≥400mg/day.
About blood glucose and insulin…
- Green coffee extract supplementation significantly improved fasting blood sugar levels
- Green coffee extract supplementation at ≥400 mg/day significantly lowered postprandial insulin levels (that’s good)
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: