Cacao vs Carob – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cacao to carob, we picked the cacao.
Why?
It’s close, and may depend a little on your priorities!
In terms of macros, the cacao has more protein and fat, while the carob has more carbohydrates, mostly sugar. Since people will not generally eat this by the spoonful, and will instead either make drinks or cook with it, we can’t speak for the glycemic index or general health impact of the sugars. As for the fats, on the one hand the cacao does contain saturated fat; on the other, this merely means that different saturated fat will usually be added to the carob if making something with it. Still, slight win for the carob on the fat front. Protein, of course, is entirely in cacao’s favor.
In the category of vitamins and minerals, they’re about equal on vitamins, while cacao wins easily on the mineral front, boasting more copper, iron, magnesium, manganese, and phosphorus.
While both have a generous antioxidant content, this one’s another win for cacao, with about 3x the active polyphenols and flavonoids.
In short: both are good, consumed in moderation and before adding unhealthy extra ingredients—but we say cacao comes out the winner.
If you’re looking specifically for the above-depicted products, by the way, here they are:
Want to learn more?
You might like to read:
- Enjoy Bitter Foods For Your Heart & Brain
- Chocolate & Health
- The Truth About Chocolate & Skin Health
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
It’s A Wrap
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We hope all our readers have had a great and healthy week! Here are some selections from health news from around the world:
A lack of transparency
Thousands of chemicals blanket-approved for food contact in packaging, under the FDA’s “Generally Recognized As Safe” umbrella, have been found in humans.
This highlights a gap in the safeguarding system, because the GRAS classification is given when there’s no known significant association with disease—but in this case, a problem can occur when the build-up in the blood and brain cause problems much later.
Read in full: Thousands of toxins from food packaging found in humans – research
Learn more: We Are Such Stuff As Bottles Are Made Of (It’s Not Fantastic To Be Plastic)
Cafestol for weight loss?
Most coffee intervention studies use instant coffee. Which is understandable; they are scientists on a budget, not coffee shop baristas. But, instant coffee is low in some of coffee’s important compounds, such as cafestol—which as it turns out, can lower not only overall body fat, but also (importantly!) visceral fat.
Read in full: 12-week coffee compound study shows promising results for weight and fat reduction in at-risk individuals
Learn more: The Bitter Truth About Coffee (or is it?)
Doing something is better than doing nothing
While a lot of the bad news both locally and around the world can be infuriating and/or depressing, turning a blind eye may not be the best approach for dealing with it. This study was in teens, but it’s likely that the benefits are similar for other ages too:
Read in full: Racial justice activism, advocacy found to reduce depression, anxiety in some teens
Learn more: Make Social Media Work For Your Mental Health
A ray of hope!
Sometimes, the topic of sun and sunscreens can seem like “damned if you do; damned if you don’t”, with regard to the harmful effects of the sun, and in some cases, potentially harmful effects of some sunscreen chemicals. We’ve argued ultimately in favor of sunscreens in this tug-of-war, but it’s nice to see improvements being made, in this case, with lignin-based sunscreen (a plant-based by-product of the pulp industry).
Read in full: Researchers create high-performing, eco-friendly sunscreen
Learn more: Who Screens The Sunscreens?
All about the pores
Researchers have identified a protein, and from that, a stack of protein fragments, that are involved in the formation of large pores. This is important, as it’s pointing to a means of relief for a lot of inflammatory diseases.
Read in full: Scientists unravel the process of pore formation in cells
Learn more: Why Do We Have Pores, And Could We Not?
Getting to the bottom of Crohn’s
If you have Crohn’s, or perhaps someone close to you has it, then you’ll be familiar with the common medical refrain of “we don’t know”. While this honesty is laudable, it’s not reassuring. So, it’s good that researchers are making progress in understanding why many people with Crohn’s may respond differently not only to lifestyle interventions, but also to various relevant drugs—allowing doctors to prescribe the right treatment for the right person.
Read in full: Patient-derived gut organoids reveal new insights into Crohn’s disease subtypes
Learn more: Diet Tips for Crohn’s Disease
Another carotenoid that holds back Alzheimer’s
Phytoene is a carotenoid that is found in many red, orange, or yellow foods, including tomatoes, carrots, apricots, red peppers, oranges, mandarins and passion fruit, among others. Researchers have found that it slows the onset of symptoms associated with the formation of amyloid plaques, by 30–40%, and increases longevity by 10–19%:
Read in full: Carotenoid phytoene shows potential in slowing Alzheimer’s plaque formation and increasing lifespan
Learn more: Brain Food? The Eyes Have It! ← this is about a different carotenoid, lutein, found mostly in dark green leafy vegetables, but it’s best to enjoy both 😎
Take care!
Share This Post
-
What Is Making The Ringing In Your Ears Worse?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Rachael Cook, an audiologist at Applied Hearing Solutions in Phoenix, Arizona, shares her professional insights into managing tinnitus.
If you’re unfamiliar with Tinnitus, it is an auditory condition characterized by a ringing, buzzing, or humming sound, and ffects nearly 10% of the population. We’ve written on Tinnitus, and how it can disrupt your life, in this article.
Key Triggers for Tinnitus
Several everyday habits can make your tinnitus louder. Caffeine and nicotine increase blood pressure, restricting blood flow to the cochlea and worsening tinnitus. Common medications, such as pain relievers, high-dose antibiotics, and antidepressants, can also exacerbate tinnitus, especially with higher or long-term dosages.
Impact of Diet and Sleep
Dietary choices significantly impact tinnitus. Alcohol and salt alter the fluid balance in the cochlea, increasing tinnitus perception. Alcohol changes blood flow patterns and neurotransmitter production, while high salt intake has similar effects. Poor sleep quality elevates stress levels, making it harder to ignore tinnitus signals. Addressing sleep disorders like sleep apnea and insomnia can help manage tinnitus symptoms.
Importance of Treating Hearing Loss
Untreated hearing loss worsens tinnitus. Nearly 90% of individuals with tinnitus have some hearing loss. Hearing aids can reduce tinnitus perception by restoring missing sounds and reducing the brain’s internal compensatory signals. Combining hearing aids with sound therapy is said to provide even greater relief.
Read more about hearing loss in our article on the topic.
Otherwise, for a great guide on managing tinnitus, we recommend watching Dr. Cook’s video:
Here’s hoping your ear’s aren’t ringing too much whilst watching the video!
Share This Post
-
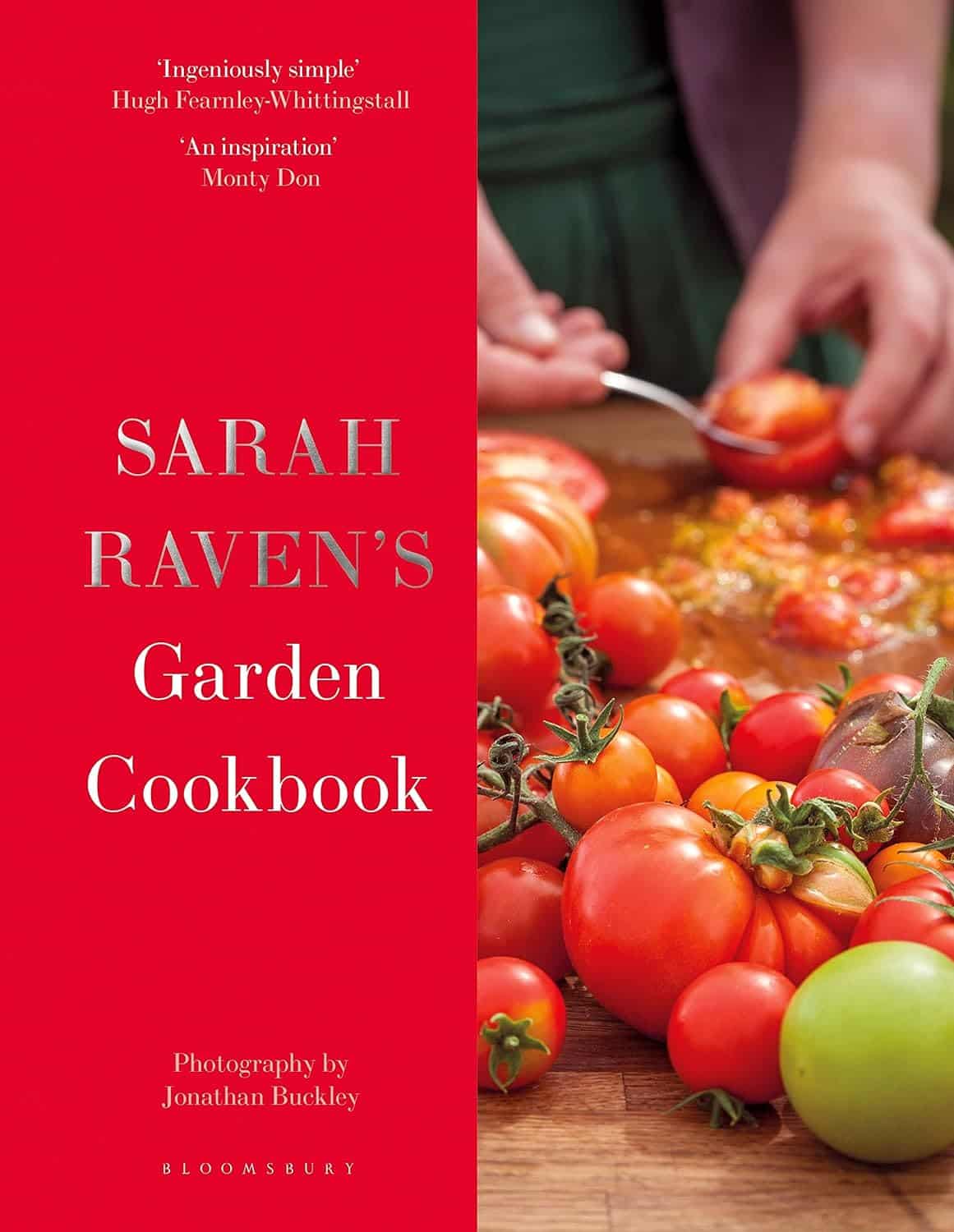
Sarah Raven’s Garden Cookbook – by Sarah Raven
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Note: the US Amazon site currently (incorrectly) lists the author as “Jonathan Buckley”. The Canadian, British, and Australian sites all list the author correctly as Sarah Raven, and some (correctly) credit Jonathan Buckley as the photographer she used.
First, what it’s not: a gardening book. Beyond a few helpful tips, pointers, and “plant here, harvest here” instructions, this book assumes you are already capable of growing your own vegetables.
She does assume you are in a temperate climate, so if you are not, this might not be the book for you. Although! The recipes are still great; it’s just you’d have to shop for the ingredients and they probably won’t be fresh local produce for the exact same reason that you didn’t grow them.
If you are in a temperate climate though, this will take you through the year of seasonal produce (if you’re in a temperate climate but it’s in for example Australia, you’ll need to make a six-month adjustment for being in the S. Hemisphere), with many recipes to use not just one ingredient from your garden at a time, but a whole assortment, consistent with the season.
About the recipes: they (which are 450 in number) are (as you might imagine) very plant-forward, but they’re generally not vegan and often not vegetarian. So, don’t expect that you’ll produce everything yourself—just most of the ingredients!
Bottom line: if you like cooking, and are excited by the idea of growing your own food but are unsure how regularly you can integrate that, this book will keep you happily busy for a very long time.
Click here to check out Sarah Raven’s Garden Cookbook, and level-up your home cooking!
Share This Post
Related Posts
-
15 Easy Japanese Habits That Will Transform Your Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The original title says “no-cost habits”, but in fairness, for most of us food is not usually free (alas). So, we will say “easy” instead, because they are indeed easy to build into your life:
15 Healthy Habits To Adopt
We’ll not keep them a mystery; they are:
- Intermittent fasting: naturally fasting for at least 12 hours overnight improves digestion and sleep quality.
- Fermented foods: regularly consuming fermented foods (like kimchi, or even just sauces like miso and shio koji) supports gut health.
- Rice & legumes over wheat: choosing wholegrain rice as a staple reduces bloating and benefits skin health (lentils are even better).
- Big breakfast, light dinner: eating a heavier breakfast and a lighter dinner gives energy in the morning and allows digestion to rest at night.
- Balancing indulgences: enjoying social meals without guilt and balancing food intake the next day.
- Daily gentle exercise: doing at least 15 minutes of yoga, Pilates, or light walking for long-term health.
- Daily baths: taking a warm bath boosts blood circulation and relaxation.
- Eating seasonal & diverse foods: including a variety of fresh, seasonal ingredients for balanced nutrition.
- Consistent morning routine: waking up at the same time, cleansing and moisturizing, and having a proper breakfast.
- Enjoying soup with meals: consuming nutrient-rich soups with vegetables and protein to prevent overeating.
- Chewing food thoroughly: eating slowly and chewing well aids digestion and enhances enjoyment.
- Light seasoning in food: avoiding overly salty or flavorful meals to appreciate natural tastes.
- Maintaining good posture: paying attention to posture during daily activities for better overall health.
- Prioritizing protein intake: eating protein-rich foods like tofu, beans, eggs, and fish, to maintain skin firmness as well as muscletone.
- Confidence in aging: focusing on internal well-being over external opinions and embracing health at every age.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hazelnuts vs Chestnuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing hazelnuts to chestnuts, we picked the hazelnuts.
Why?
This one’s not close.
In terms of macros, we have some big difference to start with, since chestnuts contain a lot more water and carbs whereas hazelnuts contain a lot more protein, fats, and fiber. The fats, as with most nuts, are healthy; in this case mostly being monounsaturated fat.
Because of the carbs and fiber being so polarized (i.e., chestnuts have most of the carbs and hazelnuts have most of the fiber), there’s a big difference in glycemic index; hazelnuts have a GI of 15 while chestnuts have a GI of 52.
In the category of vitamins, hazelnuts contain more of vitamins A, B1, B2, B3, B5, B6, and B9, while chestnuts contain more vitamin C.
When it comes to minerals, the story is similar: hazelnuts contain a lot more calcium, copper, iron, magnesium, manganese, phosphorus, and zinc, while chestnuts contain a tiny bit more potassium.
All in all, enjoy either or both, but nutritionally speaking, hazelnuts are a lot better in almost every way.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Which Magnesium? (And: When?)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Good morning! I have been waiting for this day to ask: the magnesium in my calcium supplement is neither of the two versions you mentioned in a recent email newsletter. Is this a good type of magnesium and is it efficiently bioavailable in this composition? I also take magnesium that says it is elemental (oxide, gluconate, and lactate). Are these absorbable and useful in these sources? I am not interested in taking things if they aren’t helping me or making me healthier. Thank you for your wonderful, informative newsletter. It’s so nice to get non-biased information❞
Thank you for the kind words! We certainly do our best.
For reference: the attached image showed a supplement containing “Magnesium (as Magnesium Oxide & AlgaeCal® l.superpositum)”
Also for reference: the two versions we compared head-to-head were these very good options:
Magnesium Glycinate vs Magnesium Citrate – Which is Healthier?
Let’s first borrow from the above, where we mentioned: magnesium oxide is probably the most widely-sold magnesium supplement because it’s cheapest to make. It also has woeful bioavailability, to the point that there seems to be negligible benefit to taking it. So we don’t recommend that.
As for magnesium gluconate and magnesium lactate:
- Magnesium lactate has very good bioavailability and in cases where people have problems with other types (e.g. gastrointestinal side effects), this will probably not trigger those.
- Magnesium gluconate has excellent bioavailability, probably coming second only to magnesium glycinate.
The “AlgaeCal® l.superpositum” supplement is a little opaque (and we did ntoice they didn’t specify what percentage of the magnesium is magnesium oxide, and what percentage is from the algae, meaning it could be a 99:1 ratio split, just so that they can claim it’s in there), but we can say Lithothamnion superpositum is indeed an algae and magnesium from green things is usually good.
Except…
It’s generally best not to take magnesium and calcium together (as that supplement contains). While they do work synergistically once absorbed, they compete for absorption first so it’s best to take them separately. Because of magnesium’s sleep-improving qualities, many people take calcium in the morning, and magnesium in the evening, for this reason.
Some previous articles you might enjoy meanwhile:
- Pinpointing The Usefulness Of Acupuncture
- Science-Based Alternative Pain Relief
- Peripheral Neuropathy: How To Avoid It, Manage It, Treat It
- What Does Lion’s Mane Actually Do, Anyway?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: