Ayurveda’s Contributions To Science
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ayurveda’s Contributions To Science (Without Being Itself Rooted in Scientific Method)
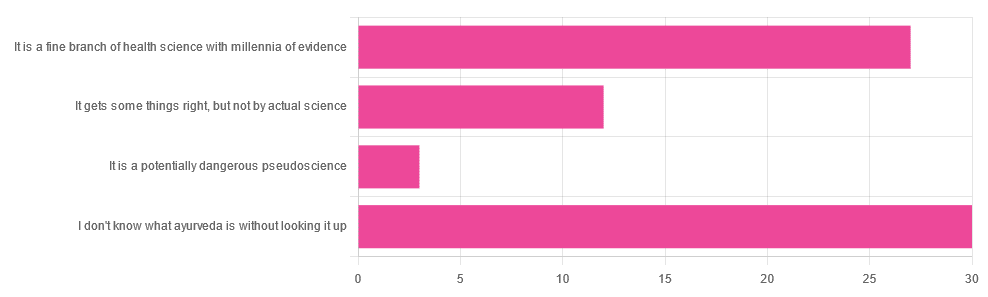
Yesterday, we asked you for your opinions on ayurveda, and got the above-depicted, below-described, set of responses. Of those who responded…
- A little over 41% said “I don’t know what ayurveda is without looking it up”
- A little over 37% said “It is a fine branch of health science with millennia of evidence”
- A little over 16% said “It gets some things right, but not by actual science”
- A little over 4% said “It is a potentially dangerous pseudoscience”
So, what does the science say?
Ayurveda is scientific: True or False?
False, simply. Let’s just rip the band-aid off in this case. That doesn’t mean it’s necessarily without merit, though!
Let’s put it this way:
- If you drink coffee to feel more awake because scientific method has discerned that caffeine has vasoconstrictive and adenosine-blocking effects while also promoting dopaminergic activity, then your consumption of coffee is evidence-based and scientific. Great!
- If you drink coffee to feel more awake because somebody told you that that somebody told them that it energizes you by balancing the elements fire (the heat of the coffee), air (the little bubbles on top), earth (the coffee grinds), water (the water), and ether (steam), then that isneither evidence-based nor scientific, but it will still work exactly the same.
Ayurveda is a little like that. It’s an ancient traditional Indian medicine, based on a combination of anecdotal evidence and supposition.
- The anecdotal evidence from ayurveda has often resulted in herbal remedies that, in modern scientific trials, have been found to have merit.
- Ayurvedic meditative practices also have a large overlap with modern mindfulness practices, and have also been found to have merit
- Ayurveda also promotes the practice of yoga, which is indeed a very healthful activity
- The supposition from ayurveda is based largely in those five elements we mentioned above, as well as a “balancing of humors” comparable to medieval European medicine, and from a scientific perspective, is simply a hypothesis with no evidence to support it.
Note: while ayurveda is commonly described as a science by its practitioners in the modern age, it did not originally claim to be scientific, but rather, wisdom handed down directly by the god Dhanvantari.
Ayurveda gets some things right: True or False?
True! Indeed, we covered some before in 10almonds; you may remember:
Bacopa Monnieri: A Well-Evidenced Cognitive Enhancer
(Bacopa monnieri is also known by its name in ayurveda, brahmi)
There are many other herbs that have made their way from ayurveda into modern science, but the above is a stand-out example. Others include:
- Ashwagandha: The Root of All Even-Mindedness?
- Boswellia serrata (Frankincense) Against Pain and Depression/Anxiety
Yoga and meditation are also great, and not only that, but great by science, for example:
- NCCIH | Yoga for Health: Clinical Guidelines, Scientific Literature, Info for Patients
- The Neuroscience of Mindfulness: How Mindfulness Alters the Brain and Facilitates Emotion Regulation
Ayurveda is a potentially dangerous pseudoscience: True or False?
Also True! We covered why it’s a pseudoscience above, but that doesn’t make it potentially dangerous, per se (you’ll remember our coffee example).
What does, however, make it potentially dangerous (dose-dependent) is its use of heavy metals such as lead, mercury, and arsenic:
Heavy Metal Content of Ayurvedic Herbal Medicine Products
Some final thoughts…
Want to learn more about the sometimes beneficial, sometimes uneasy relationship between ayurveda and modern science?
A lot of scholarly articles trying to bridge (or further separate) the two were very biased one way or the other.
Instead, here’s one that’s reasonably optimistic with regard to ayurveda’s potential for good, while being realistic about how it currently stands:
Development of Ayurveda—Tradition to trend
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

What You Don’t Know Can Kill You
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Knowledge Is Power!

This is Dr. Simran Malhotra. She’s triple board-certified (in lifestyle medicine, internal medicine, and palliative care), and is also a health and wellness coach.
What does she want us to know?
Three things:
Wellness starts with your mindset
Dr. Malhotra shifted her priorities a lot during the initial and perhaps most chaotic phase of the COVID pandemic:
❝My husband, a critical care physician, was consumed in the trenches of caring for COVID patients in the ICU. I found myself knee-deep in virtual meetings with families whose loved ones were dying of severe COVID-related illnesses. Between the two of us, we saw more trauma, suffering, and death, than we could have imagined.
The COVID-19 pandemic opened my eyes to how quickly life can change our plans and reinforced the importance of being mindful of each day. Harnessing the power to make informed decisions is important, but perhaps even more important is focusing on what is in our control and taking action, even if it is the tiniest step in the direction we want to go!❞
~ Dr. Simran Malhotra
We can only make informed decisions if we have good information. That’s one of the reasons we try to share as much information as we can each day at 10almonds! But a lot will always depend on personalized information.
There are one-off (and sometimes potentially life-saving) things like health genomics:
The Real Benefit Of Genetic Testing
…but also smaller things that are informative on an ongoing basis, such as keeping track of your weight, your blood pressure, your hormones, and other metrics. You can even get fancy:
Track Your Blood Sugars For Better Personalized Health
Lifestyle is medicine
It’s often said that “food is medicine”. But also, movement is medicine. Sleep is medicine. In short, your lifestyle is the most powerful medicine that has ever existed.
Lifestyle encompasses very many things, but fortunately, there’s an “80:20 rule” in play that simplifies it a lot because if you take care of the top few things, the rest will tend to look after themselves:
These Top Few Things Make The Biggest Difference To Overall Health
Gratitude is better than fear
If we receive an unfavorable diagnosis (and let’s face it, most diagnoses are unfavorable), it might not seem like something to be grateful for.
But it is, insofar as it allows us to then take action! The information itself is what gives us our best chance of staying safe. And if that’s not possible e.g. in the worst case scenario, a terminal diagnosis, (bearing in mind that one of Dr. Malhotra’s three board certifications is in palliative care, so she sees this a lot), it at least gives us the information that allows us to make the best use of whatever remains to us.
See also: Managing Your Mortality
Which is very important!
…and/but possibly not the cheeriest note on which to end, so when you’ve read that, let’s finish today’s main feature on a happier kind of gratitude:
How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
Want to hear more from Dr. Malhotra?
Showing how serious she is about how our genes do not determine our destiny and knowledge is power, here she talks about her “previvor’s journey”, as she puts it, with regard to why she decided to have preventative cancer surgery in light of discovering her BRCA1 genetic mutation:
Click Here If The Embedded Video Doesn’t Load Automatically
Take care!
Share This Post

What Happens To Your Body When You Stop Drinking Alcohol
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Immediately after we stop drinking is rarely when we feel our best. But how long is it before we can expect to see benefits, instead of just suffering?
Timeline
After stopping drinking alcohol for…
- Seconds: the liver starts making progress filtering out toxins and sugars; ethanol starts to leave the system
- 1 hour: fatigue sets in as the body uses a lot of energy to metabolize and eliminate alcohol. However, sleep quality (if one goes to sleep now) is low because alcohol disrupts the brain patterns required for restful sleep
- 6–12 hours: the immune system starts recovering from the suppression caused by alcohol
- 24 hours: immune system is back to normal; withdrawal symptoms may occur in the case of heavy drinkers
- 3–5 days: resting blood pressure begins to drop, as stress levels decrease (alcohol may seem anxiolytic, but it is actually anxiogenic; it just masks its own effect in this regard). Also, because of insulin responses improving, appetite reduces. The liver, once it has finished dealing your last drinking session (if you used to drink all the time, it probably had a backlog to clear), can now begin to make repairs on itself.
- 1 week: skin will start looking better, as antidiuretic hormone levels neutralize, leading to a healthier maintenance of hydration
- 2 weeks: cognitive abilities improve as the brain begins to make progress in repairing itself. At the same time, kidneys start to heal.
- 3–4 weeks: the liver begins to regenerate in earnest. You may wonder what took it so long given the liver’s famous regenerative abilities, but in this case, the liver was also the organ that took the most damage from drinking, so its regeneration gets off to a slow start (in contrast, if the liver had “merely” suffered physical trauma, such as being shot, stabbed,
or eaten by eagles,it’d start regenerating vigorously as soon as the immediate wound-response had been tended to). Once it is able to pick up the pace though, overall health improves, as the liver can focus on breaking down other toxins. - 1–2 months: the heart is able to repair itself, and start to become stronger again (dependent on other lifestyle factors, of course).
- 3 months and more: bodily repairs continue (for example, the damage to the liver is often so severe that it can take quite a bit longer to recover completely, and repairs in the brain are always slow, for reasons beyond the scope of this article). Looking at the big picture, at this point we also see other benefits, such as reduced cancer risks.
In short… It’s never too soon to stop, but it’s also never too late, unless you are going to die in the next few days. So long as you’ll be in the land of the living for a few days yet, there’s time to enjoy the benefits of stopping.
Most importantly: the timeline for the most important repairs is not as long as many people might think, and that itself can be very motivating.
For more detail on much of the above, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Can We Drink To Good Health?
- How To Reduce Or Quit Alcohol
- Addiction Myths That Are Hard To Quit
- How To Unfatty A Fatty Liver
Take care!
Share This Post

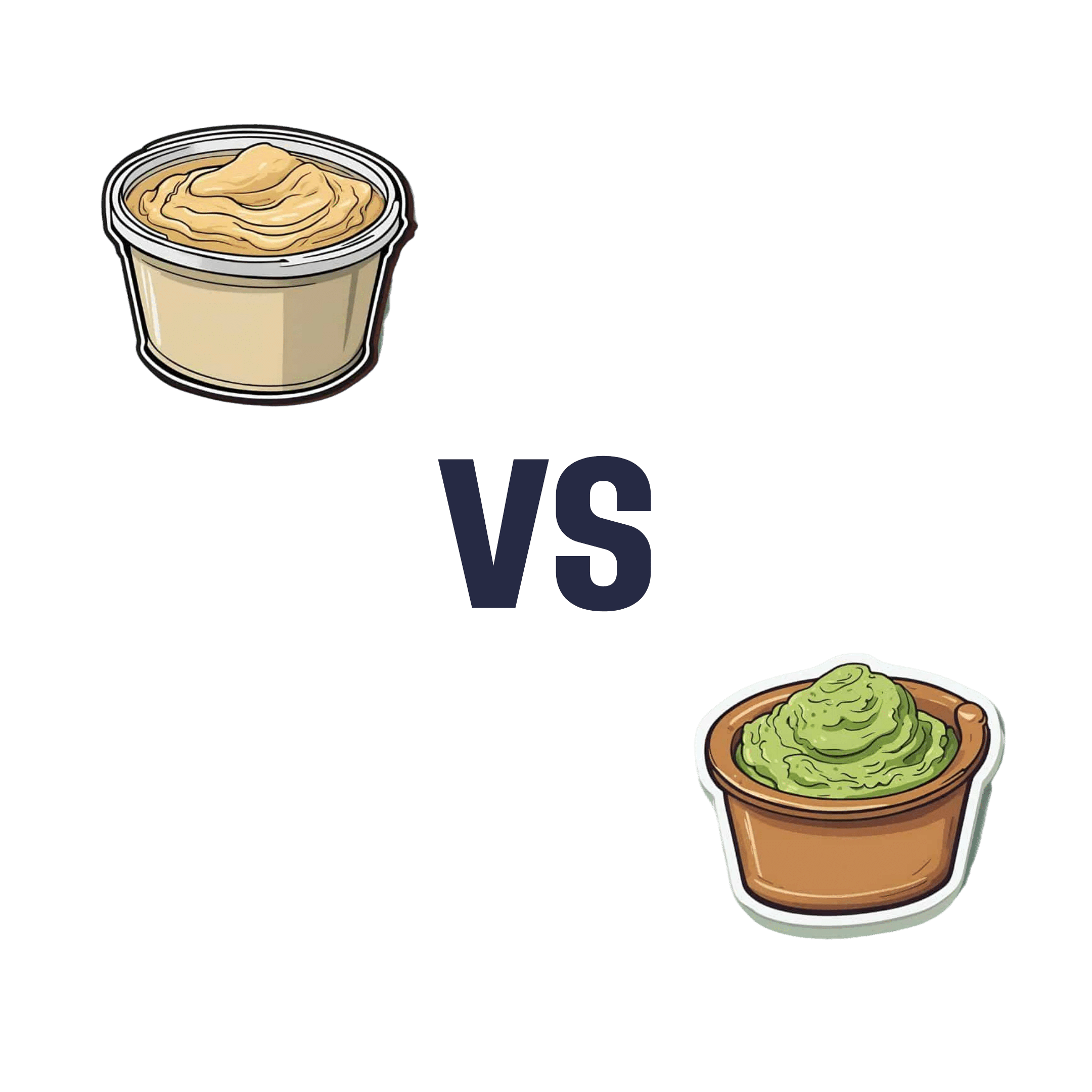
Hummus vs Guacamole – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing hummus to guacamole, we picked the guacamole.
Why?
First up, let’s assume that the standards are comparable, for example that both have been made with simple whole foods. The hummus is mostly chickpeas with tahini and a little olive oil and some seasoning; the guacamole is mostly avocado with a little lime juice and some seasoning.
In terms of macronutrients, hummus has slightly more protein and fiber, 2x the carbohydrates (but they are healthy carbs), and usually slightly less fat (but the fats are healthy in both cases).
In terms of micronutrients, the hummus is rich in iron and B vitamins, and the guacamole is rich in potassium, magnesium, vitamins C, E, and K.
So far, it’s pretty much tied. What else is there to consider?
We picked the guacamole because some of its nutrients (especially the potassium, magnesium, and vitamin K) are more common deficiencies in most people’s diets than iron and B vitamins. So, on average, it’s probably the one with the nutrients that you need more of at any given time.
So, it was very very close, and it came down to the above as the deciding factor.
However!
- If you like one and not the other? Eat that one; it’s good.
- If you like both but feel like eating one of them in particular? Eat that one; your body is probably needing those nutrients more right now.
- If you are catering for a group of people? Serve both!
- If you are catering for just yourself and would enjoy both? Serve both! There’s nobody to stop you!
Want to read more?
You might like: Avocado Oil vs Olive Oil – Which is Healthier?
Enjoy!
Share This Post
Related Posts

Jasmine McDonald’s Ballet Stretching Routine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Why Jasmine’s Video is Useful
Jasmine McDonald is not only a professional ballerina, but is also a certified personal trainer, so when it comes to keeping her body strong and flexible, she’s a wealth of knowledge. Her video (below) is a great example of this.
In case you’re interested in learning more, she currently (privately) tutors over 30 people on a day-to-day basis. You can contact her here!
Other Stretches?
If you think that Jasmine’s stretches may be out of your league, we recommend checking out our other articles on stretching, including:
- 11 Minutes to Pain-Free Hips
- How to Permanently Loosen a Tight Psoas
- Stretching Scientifically
- Stretching & Mobility
- Stretching to Stay Young
Otherwise, let loose on these dancer stretches and exercises:
How did you find that video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

In Plain English…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Time!
This is the bit whereby each week, we respond to subscriber questions/requests/etc
Have something you’d like to ask us, or ask us to look into? Hit reply to any of our emails, or use the feedback widget at the bottom, and a Real Human™ will be glad to read it!
Q: Love to have someone research all the additives in our medicines, (risk of birth control and breast cancer) and what goes in all of our food and beverages. So much info out there, but there are so many variations, you never know who to believe.
That’s a great idea! There are a lot of medicines and food and beverages out there, so that’s quite a broad brief, but! We could well do a breakdown of very common additives, and demystify them, sorting them into good/bad/neutral, e.g:
- Ascorbic acid—Good! This is Vitamin C
- Acetic acid—Neutral! This is vinegar
- Acetylsalicylic acid—Good or Bad! This is aspirin (a painkiller and blood-thinning agent, can be good for you or can cause more problems than it solves, depending on your personal medical situation. If in doubt, check with your doctor)
- Acesulfame K—Generally Neutral! This is a sweetener that the body can’t metabolize, so it’s also not a source of potassium (despite containing potassium) and will generally do nothing. Unless you have an allergy to it, which is rare but is a thing.
- Sucralose—Neutral! This is technically a sugar (as is anything ending in -ose), but the body can’t metabolize it and processes it as a dietary fiber instead. We’d list it as good for that reason, but honestly, we doubt you’re eating enough sucralose to make a noticeable difference to your daily fiber intake.
- Sucrose—Bad! This is just plain sugar
Sometimes words that sound the same can ring alarm bells when they need not, for example there’s a big difference between:
- Potassium iodide (a good source of potassium and iodine)
- Potassium cyanide (the famous poison; 300mg will kill you; half that dose will probably kill you)
- Cyanocobalamine (Vitamin B12)
Let us know if there are particular additives (or particular medications) you’d like us to look at!
While for legal reasons we cannot give medical advice, talking about common contraindications (e.g., it’s generally advised to not take this with that, as one will stop the other from working, etc) is definitely something we could do.
For example! St. John’s Wort, very popular as a herbal mood-brightener, is on the list of contraindications for so many medications, including:
- Antidepressants
- Birth control pills
- Cyclosporine, which prevents the body from rejecting transplanted organs
- Some heart medications, including digoxin and ivabradine
- Some HIV drugs, including indinavir and nevirapine
- Some cancer medications, including irinotecan and imatinib
- Warfarin, an anticoagulant (blood thinner)
- Certain statins, including simvastatin
Q: As I am a retired nurse, I am always interested in new medical technology and new ways of diagnosing. I have recently heard of using the eyes to diagnose Alzheimer’s. When I did some research I didn’t find too much. I am thinking the information may be too new or I wasn’t on the right sites.
(this is in response to last week’s piece on lutein, eyes, and brain health)
We’d readily bet that the diagnostic criteria has to do with recording low levels of lutein in the eye (discernible by a visual examination of macular pigment optical density), and relying on the correlation between this and incidence of Alzheimer’s, but we’ve not seen it as a hard diagnostic tool as yet either—we’ll do some digging and let you know what we find! In the meantime, we note that the Journal of Alzheimer’s Disease (which may be of interest to you, if you’re not already subscribed) is onto this:
See also:
- Journal of Alzheimer’s Disease (mixture of free and paid content)
- Journal of Alzheimer’s Disease Reports (open access—all content is free)
Q: As to specific health topics, I would love to see someone address all these Instagram ads targeted to women that claim “You only need to ‘balance your hormones’ to lose weight, get ripped, etc.” What does this mean? Which hormones are they all talking about? They all seem to be selling a workout program and/or supplements or something similar, as they are ads, after all. Is there any science behind this stuff or is it mostly hot air, as I suspect?
Thank you for asking this, as your question prompted yesterday’s main feature, What Does “Balancing Your Hormones” Even Mean?
That’s a great suggestion also about addressing ads (and goes for health-related things in general, not just hormonal stuff) and examining their claims, what they mean, how they work (if they work!), and what’s “technically true but may
be misleading* cause confusion”*We don’t want companies to sue us, of course.
Only, we’re going to need your help for this one, subscribers!
See, here at 10almonds we practice what we preach. We limit screen time, we focus on our work when working, and simply put, we don’t see as many ads as our thousands of subscribers do. Also, ads tend to be targeted to the individual, and often vary from country to country, so chances are good that we’re not seeing the same ads that you’re seeing.
So, how about we pull together as a bit of a 10almonds community project?
- Step 1: add our email address to your contacts list, if you haven’t already
- Step 2: When you see an ad you’re curious about, select “share” (there is usually an option to share ads, but if not, feel free to screenshot or such)
- Step 3: Send the ad to us by email
We’ll do the rest! Whenever we have enough ads to review, we’ll do a special on the topic.
We will categorically not be able to do this without you, so please do join in—Many thanks in advance!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Stop Sabotaging Your Gut
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.

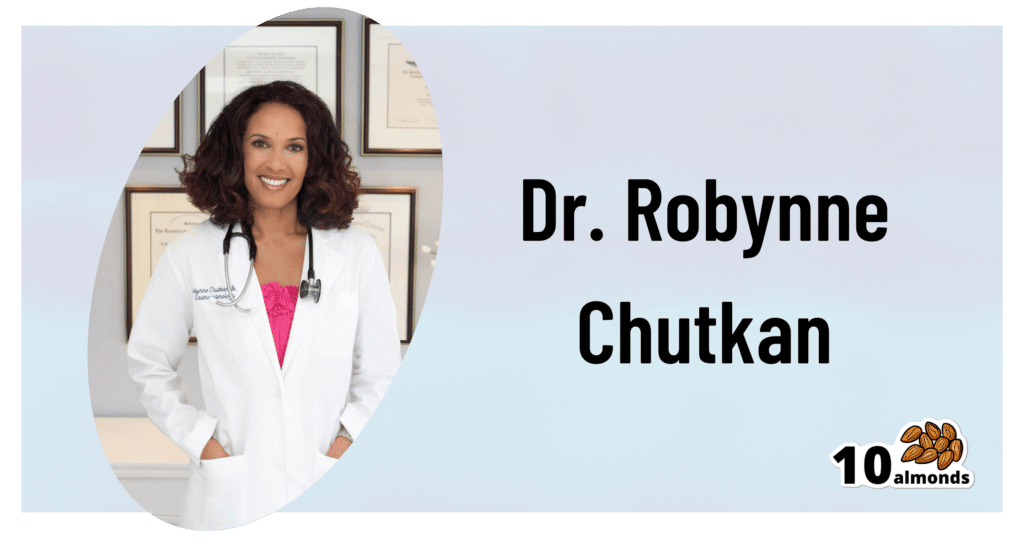
This is Dr. Robynne Chutkan. She’s an integrative gastroenterologist, and founder of the Digestive Center for Wellness, in Washington DC, which for the past 20 years has been dedicated to uncovering the root causes of gastrointestinal disorders, while the therapeutic side of things has been focused on microbial optimization, nutritional therapy, mind-body techniques, and lifestyle changes.
In other words, maximal health for minimal medicalization.
So… What does she want us to know?
Live dirty
While attentive handwashing is important to avoid the spread of communicable diseases*, excessive cleanliness in general can result in an immune system that has no idea how to deal with pathogens when exposure does finally occur.
*See also: The Truth About Handwashing
This goes doubly for babies: especially those who were born by c-section and thus missed out on getting colonized by vaginal bacteria, and especially those who are not breast-fed, and thus miss out on nutrients given in breast milk that are made solely for the benefit of certain symbiotic bacteria (humans can’t even digest those particular nutrients, we literally evolved to produce some nutrients solely for the bacteria).
See also: Breast Milk’s Benefits That Are (So Far) Not Replicable
However, it still goes for the rest of us who are not babies, too. We could, Dr. Chutkan tells us, stand to wash less in general, and definitely ease up on antibacterial soaps and so forth.
See also: Should You Shower Daily?
Take antibiotics only if absolutely necessary (and avoid taking them by proxy)
Dr. Chutkan describes antibiotics as the single biggest threat to our microbiome, not just because of overprescription, but also the antibiotics that are used in animal agriculture and thus enter the food chain (and thus, enter us, if we eat animal products).
Still, while the antibiotics meat/dairy-enjoyers will get from food are better avoided, antibiotics actually taken directly are even worse, and are absolutely a “scorched earth” tactic against whatever they’re being prescribed for.
See also: Antibiotics? Think Thrice ← which also brings up “Four Ways Antibiotics Can Kill You”; seriously, the risks of antibiotics are not to be underestimated, including the risks associated only with them working exactly as intended—let alone if something goes wrong.
Probiotics won’t save you
While like any gastroenterologist (or really, almost any person in general), she notes that probiotics can give a boost to health. However, she wants us to know about two shortcomings that are little-discussed:
1) Your body has a collection of microbiomes each with their own needs, and while it is possible to take “generally good” bacteria in probiotics and assume they’ll do good, taking Lactobacillus sp. will do nothing for a shortage of Bifidobacteria sp, and even taking the correct genus can have similar shortcomings if a different species of that genus is needed, e.g. taking L. acidophilus will do nothing for a shortage of L. reuteri.
It’d be like a person with a vitamin D deficiency taking vitamin B12 supplements and wondering why they’re not getting better.
2) Probiotics are often wasted if not taken mindfully of their recipient environment. For example, most gut bacteria only live for about 20 minutes in the gut. They’re usually inactive in the supplement form, they’re activated in the presence of heat and moisture and appropriate pH etc, and then the clock is ticking for them to thrive or die.
This means that if you take a supplement offering two billion strains of good gut bacteria, and you take it on an empty stomach, then congratulations, 20 minutes later, they’re mostly dead, because they had nothing to eat. Or if you take it after drinking a soda, congratulations, they’re mostly dead because not only were they starved, but also their competing “bad” microbes weren’t starved and changed the environment to make it worse for the “good” ones.
For this reason, taking probiotics with (or immediately after) plenty of fiber is best.
This is all accentuated if you’re recovering from using antibiotics, by the way.
Imagine: a nuclear war devastates the population of the Earth. Some astronauts manage to safely return, finding a mostly-dead world covered in nuclear winter. Is the addition of a few astronauts going to quickly repopulate the world? No, of course not. They are few, the death toll is many, and the environment is very hostile to life. A hundred years later, the population will be pretty much the same—a few straggling survivors.
It’s the same after taking antibiotics, just, generations pass in minutes instead of decades. You can’t wipe out almost everything beneficial in the gut, create a hostile environment there, throw in a couple of probiotic gummies, and expect the population to bounce back.
That said, although “probiotics will not save you”, they can help provided you give them a nice soft bed of fiber to land on, some is better than none, and guessing at what strains are needed is better than giving nothing.
See also: How Much Difference Do Probiotic Supplements Make, Really?
What she recommends
So to recap, we’ve had:
- Wash less, and/or with less harsh chemicals
- Avoid antibiotics like the plague, unless you literally have The Plague, for which the treatment is indeed antibiotics
- Avoid antibiotic-contaminated foods, which in the US is pretty much all animal products unless it’s, for example, your own back-yard hens whom you did not give antibiotics. Do not fall for greenwashing aesthetics in the packaging of “happy cows” and their beef, milk, etc, “happy hens” and their meat, eggs, etc… If it doesn’t explicitly claim to be free from the use of antibiotics, then antibiotics were almost certainly used.
- Dr. Chutkan herself is not even vegan, by the way, but very much wants us to be able to make informed choices about this, and does recommend at least a “plants-forward” diet, for the avoiding-antibiotics reason and for the plenty-of-fiber reason, amongst others.
- Consider probiotics, but don’t expect them to work miracles by themselves; you’ve got to help them to help you.
- Dr. Chutkan also recommends getting microbiome tests done if you think something might be amiss, and then you can supplement with probiotics in a more targetted fashion instead of guessing at what species is needed where.
She also recommends, of course, a good gut-healthy diet in general, especially “leafy green things that were recently alive; not powders”, beans, and nuts, while avoiding gut-unhealthy things such as sugars-without-fiber, alcohol, or some gut-harmful additives (such as most artificial sweeteners, although stevia is a gut-healthy exception, and sucralose is ok in moderation).
For more on gut-healthy eating, check out:
Make Friends With Your Gut (You Can Thank Us Later)
Want to know more from Dr. Chutkan?
We recently reviewed an excellent book of hers:
The Anti-Viral Gut: Tackling Pathogens From The Inside Out – by Dr. Robynne Chutkan
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: