An Addiction Expert’s Insights On Festive Drinking
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Christopher Kahler. He’s Professor of Behavioral and Social Sciences, Director of Alcohol and Addiction Studies, Professor of Psychiatry and Human Behavior, all at Brown University.
What does he want us to know?
It’s the trickiest time of the year
Per stats, alcohol sales peak in December, with the heaviest drinking being from mid-December (getting an early start on the Christmas cheer) to New Year’s Eve. As for why, there’s a collection of reasons, as he notes:
❝The main challenge is there’s an extra layer of stress, with a lot of obligations and expectations from friends and family. We’re around people who maybe we’re not usually around, and in larger groups. It’s also a time of heightened emotion and, for some people, loneliness.
On top of that, alcohol use is built into a lot of our winter holiday traditions. It’s often marketed as part of the “good life.” We’re expected to have alcohol when we celebrate.❞
As for how much alcohol is safe to drink… According to the World Health Organization, the only safe amount of alcohol is zero:
Dr. Kahler acknowledges, however, that many people will wish to imbibe anyway, and indeed, he himself does drink a little, but endeavours to do so mindfully, and as such, he recommends that we…
HALT!
Dr. Kahler counsels us against making decisions (including the decision to drink alcohol), on occasions when we are one or more of the following:
- Hungry
- Angry
- Lonely
- Tired
He also notes that around this time of year, often our normal schedules and habits are disrupted, which introduces more microdecisions to our daily lives, which in turn means more “decision fatigue”, and the greater chance of making bad decisions.
We share some practical tips on how to reduce the chances of thusly erring, here:
Set your intentions now
He bids us figure out what our goal is, and really think it through, including not just “how many drinks to have” if we’re drinking, but also such things as “what feelings are likely to come up”. Because, if we’ve historically used alcohol as a maladaptive coping mechanism, we’re going to need a different, better, healthier coping mechanism (we talked more about that in our above-linked article about reducing or quitting alcohol, too, with some examples).
He also suggests that we memorize our social responses—exactly what we’re going to say if offered a drink, for example:
❝It’s important to know what you’re going to say about your alcohol use. If someone asks if they can get you a drink, good responses could be: “A glass of water would be great” or “Do you have any non-alcoholic cider?” You don’t have to explain yourself. Just ask for what you want, because saying no to someone can be difficult.❞
See also:
December’s Traps To Plan Around
Mix it up and slow it down
No, that doesn’t mean mix yourself a sloe gin cocktail. But rather, it’s about alternating alcoholic and non-alcoholic drinks, to give your body half a chance to process the alcohol, and also to rehydrate a little along the way.
We talk about this and other damage-limitation methods, here:
How To Reduce The Harm Of Festive Drinking (Without Abstaining)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
9 Little Habits To Have A Better Day
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Practically gift-wrapped, here are 9 key things to improve any day!
Mindfully does it
These are all things that seem obvious when you read them, but take a moment to consider: how many do you actually do on a daily basis, really? And could you implement the others?
- Remember to be thankful: train your brain to focus on the good in life, either in the morning to start the day positively or at night to unload stress. Or both!
- Change your scenery: visiting new places, even just a walk in the park, can refresh your mind and improve your mood.
- Do one thing at a time: multitasking leads to unfinished, low-quality work. Focusing on one task at a time all but ensures better results.
- Laugh: laughter releases feel-good hormones of various kinds, spreads joy, and relieves tension, making the day more enjoyable. It has longevity-boosting effects too!
- Help someone: helping others boosts happiness, enhances self-worth, and might even provide insights into your own problems. As a bonus, it actually helps the other person, too—so “pay it forward” and all that 🙂
- Prepare the night before: prepping ahead prevents morning stress, making for a smoother and more confident start to the day—which sets the tone of the rest of the day.
- Hype yourself up: even temporary self-belief can boost confidence and its effects are incrementally cumulative over time.
- Relaxation: establish an evening routine (like reading or listening to calming music) to de-stress and improve sleep quality.
- Take your time: being present in the moment enhances enjoyment, improves focus, and cultivates gratitude—which takes us back to #1!
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Are You Flourishing? (There’s a Scale)
Take care!
Share This Post
-
Mediterranean Air Fryer Cookbook – by Naomi Lane
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are Mediterranean Diet cookbooks, and there are air fryer cookbooks. And then there are (a surprisingly large intersection of!) Mediterranean Diet air fryer cookbooks. We wanted to feature one of them in today’s newsletter… And as part of the selection process, looked through quite a stack of them, and honestly, were quite disappointed with many. This one, however, was one of the ones that stood out for its quality of both content and clarity, and after a more thorough reading, we now present it to you:
Naomi Lane is a professional dietician, chef, recipe developer, and food writer… And it shows, on all counts.
She covers what the Mediterranean diet is, and she covers far more than this reviewer knew it was even possible to know about the use of an air fryer. That alone would make the book a worthy purchase already.
The bulk of the book is the promised 200 recipes. They cover assorted dietary requirements (gluten-free, dairy-free, etc) while keeping to the Mediterranean Diet.
The recipes are super clear, just what you need to know, no reading through a nostalgic storytime first to find things. Also no pictures, which will be a plus for some readers and a minus for others. The recipes also come complete with nutritional information for each meal (including sodium), so you don’t have to do your own calculations!
Bottom line: this is the Mediterranean Diet air fryer cook book. Get it, thank us later!
Get your copy of “Mediterranean Air Fryer Cookbook” on Amazon today!
Share This Post
-
The Brain-Gut Highway: A Two-Way Street
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Brain-Gut Two-Way Highway
This is Dr. Emeran Mayer. He has the rather niche dual specialty of being a gastroenterologist and a neurologist. He has published over 353 peer reviewed scientific articles, and he’s a professor in the Departments of Medicine, Physiology, and Psychiatry at UCLA. Much of his work has been pioneering medical research into gut-brain interactions.
We know the brain and gut are connected. What else does he want us to know?
First, that it is a two-way interaction. It’s about 90% “gut tells the brain things”, but it’s also 10% “brain tells the gut things”, and that 10% can make more like a 20% difference, if for example we look at the swing between “brain using that 10% communication to tell gut to do things worse” or “brain using that 10% communication to tell gut to do things better”, vs the midpoint null hypothesis of “what the gut would be doing with no direction from the brain”.
For example, if we are experiencing unmanaged chronic stress, that is going to tell our gut to do things that had an evolutionary advantage 20,000–200,000 years ago. Those things will not help us now. We do not need cortisol highs and adrenal dumping because we ate a piece of bread while stressed.
Read more (by Dr. Mayer): The Stress That Evolution Has Not Prepared Us For
With this in mind, if we want to look after our gut, then we can start before we even put anything in our mouths. Dr. Mayer recommends managing stress, anxiety, and depression from the head downwards as well as from the gut upwards.
Here’s what we at 10almonds have written previously on how to manage those things:
- No-Frills, Evidence-Based Mindfulness
- How To Set Anxiety Aside
- The Mental Health First-Aid You’ll Hopefully Never Need
Do eat for gut health! Yes, even if…
Unsurprisingly, Dr. Mayer advocates for a gut-friendly, anti-inflammatory diet. We’ve written about these things before:
…but there’s just one problem:
For some people, such as with IBS, Crohn’s, and colitis, the Mediterranean diet that we (10almonds and Dr. Mayer) generally advocate for, is inaccessible. If you (if you have those conditions) eat as we describe, a combination of the fiber in many vegetables and the FODMAPs* in many fruits, will give you a very bad time indeed.
*Fermentable Oligo-, Di-, Monosaccharides And Polyols
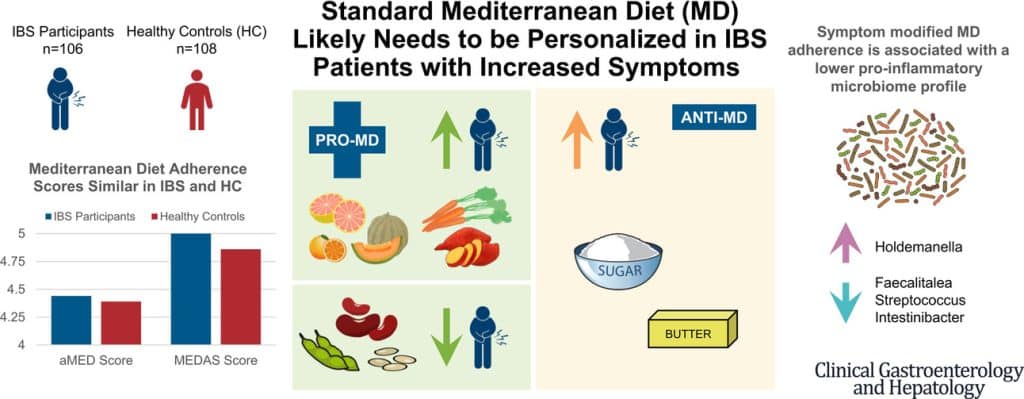
Dr. Mayer has the answer to this riddle, and he’s not just guessing; he and his team did science to it. In a study with hundreds of participants, he measured what happened with adherence (or not) to the Mediterranean diet (or modified Mediterranean diet) (or not), in participants with IBS (or not).
The results and conclusions from that study included:
❝Among IBS participants, a higher consumption of fruits, vegetables, sugar, and butter was associated with a greater severity of IBS symptoms. Multivariate analysis identified several Mediterranean Diet foods to be associated with increased IBS symptoms.
A higher adherence to symptom-modified Mediterranean Diet was associated with a lower abundance of potentially harmful Faecalitalea, Streptococcus, and Intestinibacter, and higher abundance of potentially beneficial Holdemanella from the Firmicutes phylum.
A standard Mediterranean Diet was not associated with IBS symptom severity, although certain Mediterranean Diet foods were associated with increased IBS symptoms. Our study suggests that standard Mediterranean Diet may not be suitable for all patients with IBS and likely needs to be personalized in those with increased symptoms.❞
In graphical form:
And if you’d like to read more about this (along with more details on which specific foods to include or exclude to get these results), you can do so…
- The study itself (full article): The Association Between a Mediterranean Diet and Symptoms of Irritable Bowel Syndrome
- Dr. Mayer’s blog (lay explanation): The Benefits of a Modified Mediterranean Diet for Irritable Bowel Syndrome
Want to know more?
Dr. Mayer offers many resources, including a blog, books, recipes, podcasts, and even a YouTube channel:
Share This Post
Related Posts
-
It’s On Me – by Dr. Sara Kuburic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This isn’t about bootstrapping and nor is it a motivational pep talk. What it is, however, is a wake-up call for the wayward, and that doesn’t mean “disaffected youth” or such. Rather, therapist Dr. Sara Kuburic tackles the problem of self-loss.
It’s about when we get so caught up in what we need to do, should do, are expected to do, are in a rut of doing… That we forget to also live. After all, we only get one shot at life so far as we know, so we might as well live it in whatever way is right for us.
That probably doesn’t mean a life of going through the motions.
The writing style here is personal and direct, and it makes for quite compelling reading from start to finish.
Bottom line: if ever you find yourself errantly sleepwalking through life and would like to change that, this is a book for you.
Click here to check out It’s On Me, and take control of what’s yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Meningitis Outbreak
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Don’t Let Your Guard Down
In the US, meningitis is currently enjoying a 10-year high, with its highest levels of infection since 2014.
This is a big deal, given the 10–15% fatality rate of meningitis, even with appropriate medical treatment.
But of course, not everyone gets appropriate medical treatment, especially because symptoms can become life-threatening in a matter of hours.
Most recent stats gave an 18% fatality rate for the cases with known outcomes in the last year:
CDC Emergency | Increase in Invasive Serogroup Y Meningococcal Disease in the United States
The quick facts:
❝Meningococcal disease most often presents as meningitis, with symptoms that may include fever, headache, stiff neck, nausea, vomiting, photophobia, or altered mental status.
[It can also present] as meningococcal bloodstream infection, with symptoms that may include fever and chills, fatigue, vomiting, cold hands and feet, severe aches and pains, rapid breathing, diarrhea, or, in later stages, a dark purple rash.
While initial symptoms of meningococcal disease can at first be non-specific, they worsen rapidly, and the disease can become life-threatening within hours. Immediate antibiotic treatment for meningococcal disease is critical.
Survivors may experience long-term effects such as deafness or amputations of the extremities.❞
~ Ibid.
The good news (but still don’t let your guard down)
Meningococcal bacteria are, happily, not spread as easily as cold and flu viruses.
The greatest risks come from:
- Close and enduring proximity (e.g. living together)
- Oral, or close-to-oral, contact (e.g. kissing, or coughing nearby)
Read more:
CDC | Meningococcal Disease: Causes & How It Spreads
Is there a vaccine?
There is, but it’s usually only offered to those most at risk, which is usually:
- Children
- Immunocompromised people, especially if HIV+
- People taking certain medications (e.g. Solaris or Ultomiris)
Read more:
CDC | Meningococcal Vaccine Recommendations
Will taking immune-boosting supplements help?
Honestly, probably not, but they won’t harm either. The most important thing is: don’t rely on them—too many people pop a vitamin C supplement and then assume they are immune to everything, and it doesn’t work like that.
On a tangential note, for more general immune health, you might also want to check out:
Beyond Supplements: The Real Immune-Boosters!
The short version:
If you or someone you know experiences the above-mentioned symptoms, even if it does not seem too bad, get thee/them to a doctor, and quickly, because the (very short) clock may be ticking already.
Better safe than sorry.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healthy Butternut Macaroni Cheese
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A comfort food classic, healthy and plant-based, without skimping on the comfort.
You will need
- ½ butternut squash, peeled and cut into small pieces (if buying ready-chopped, this should be about 1 lb)
- 1 onion, chopped
- ¼ bulb garlic
- 2 tbsp extra virgin olive oil
- 12 oz (or thereabouts) wholegrain macaroni, or similar pasta shape (even penne works fine—which is good, as it’s often easier to buy wholegrain penne than wholegrain macaroni) (substitute with a gluten-free pasta such as buckwheat pasta, if avoiding gluten)
- 6 oz (or thereabouts) cashews, soaked in hot water for at least 15 minutes (but longer is better)
- ½ cup milk (your preference what kind; we recommend hazelnut for its mellow nutty flavor)
- 3 tbsp nutritional yeast
- Juice of ½ lemon
- 2 tsp black pepper, coarse ground
- ½ tsp MSG, or 1 tsp low-sodium salt
- Optional: smoked paprika, to serve
Note: if you are allergic to nuts, please accept our apologies that there’s no substitution available in this one. Simply put, removing the cashews would mean changing most of the rest of the recipe to compensate, so there’s no easy “or substitute with…” that we can mention. We’ll have to find/develop a good healthy plant-based no-nuts recipe for you at a later date.
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400℉ / 200℃.
2) Combine the butternut squash, onion, and garlic with the olive oil, in a large roasting tin, tossing thoroughly to ensure an even coat of oil. Roast them for about 25 minutes until soft.
3) Cook the macaroni while you wait (this should take about 10 minutes or so in salted water), drain, and rinse thoroughly in cold water, before setting aside. This cooling increases the pasta’s resistant starch content (that’s good, for your gut and for your blood sugars, and thus also for your heart and brain), and it will maintain this benefit even when we reheat it later.
4) Drain the cashews, and tip them into a high-speed blender with the milk, and process until smooth. Add the roasted vegetables and the remaining ingredients apart from the pasta, and continue to process until again smooth. You can add a little more milk if you need to, but go easy with it.
5) Heat the sauce (that you just made in the food processor) gently in a saucepan, and refresh the pasta by pouring a kettle of boiling water through it in a colander.
6) Optional: combine the pasta and sauce in an ovenproof dish or cast iron pan, and give it a few minutes under the hottest grill (or browning iron, if you have such) your oven can muster. Alternatively, use a culinary blowtorch, if you have one.
7) Serve; and if you didn’t do the optional step above, this means combining the pasta and sauce. You can also dust the top with some extra seasonings if you like. Smoked paprika works well for this.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Butternut Squash vs Pumpkin – Which is Healthier?
- Cashew Nuts vs Coconut – Which is Healthier?
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Sea Salt vs MSG – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: