The Brain-Gut Two-Way Highway
This is Dr. Emeran Mayer. He has the rather niche dual specialty of being a gastroenterologist and a neurologist. He has published over 353 peer reviewed scientific articles, and he’s a professor in the Departments of Medicine, Physiology, and Psychiatry at UCLA. Much of his work has been pioneering medical research into gut-brain interactions.
We know the brain and gut are connected. What else does he want us to know?
First, that it is a two-way interaction. It’s about 90% “gut tells the brain things”, but it’s also 10% “brain tells the gut things”, and that 10% can make more like a 20% difference, if for example we look at the swing between “brain using that 10% communication to tell gut to do things worse” or “brain using that 10% communication to tell gut to do things better”, vs the midpoint null hypothesis of “what the gut would be doing with no direction from the brain”.
For example, if we are experiencing unmanaged chronic stress, that is going to tell our gut to do things that had an evolutionary advantage 20,000–200,000 years ago. Those things will not help us now. We do not need cortisol highs and adrenal dumping because we ate a piece of bread while stressed.
Read more (by Dr. Mayer): The Stress That Evolution Has Not Prepared Us For
With this in mind, if we want to look after our gut, then we can start before we even put anything in our mouths. Dr. Mayer recommends managing stress, anxiety, and depression from the head downwards as well as from the gut upwards.
Here’s what we at 10almonds have written previously on how to manage those things:
- No-Frills, Evidence-Based Mindfulness
- How To Set Anxiety Aside
- The Mental Health First-Aid You’ll Hopefully Never Need
Do eat for gut health! Yes, even if…
Unsurprisingly, Dr. Mayer advocates for a gut-friendly, anti-inflammatory diet. We’ve written about these things before:
…but there’s just one problem:
For some people, such as with IBS, Crohn’s, and colitis, the Mediterranean diet that we (10almonds and Dr. Mayer) generally advocate for, is inaccessible. If you (if you have those conditions) eat as we describe, a combination of the fiber in many vegetables and the FODMAPs* in many fruits, will give you a very bad time indeed.
*Fermentable Oligo-, Di-, Monosaccharides And Polyols
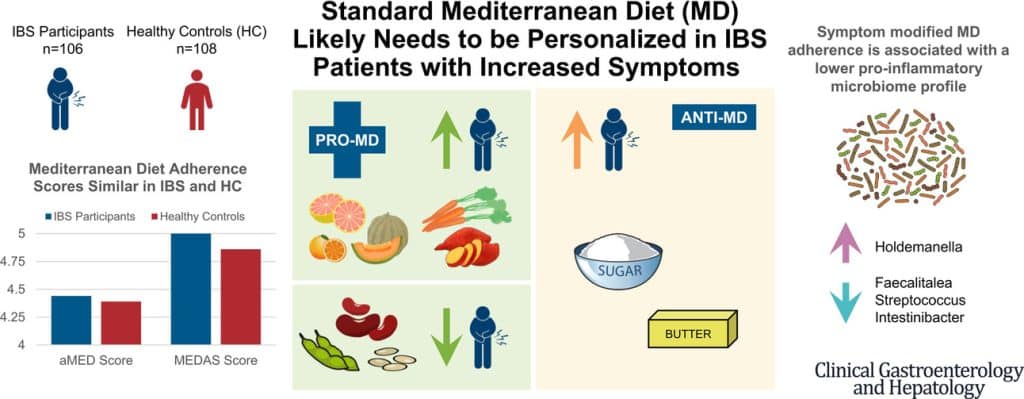
Dr. Mayer has the answer to this riddle, and he’s not just guessing; he and his team did science to it. In a study with hundreds of participants, he measured what happened with adherence (or not) to the Mediterranean diet (or modified Mediterranean diet) (or not), in participants with IBS (or not).
The results and conclusions from that study included:
❝Among IBS participants, a higher consumption of fruits, vegetables, sugar, and butter was associated with a greater severity of IBS symptoms. Multivariate analysis identified several Mediterranean Diet foods to be associated with increased IBS symptoms.
A higher adherence to symptom-modified Mediterranean Diet was associated with a lower abundance of potentially harmful Faecalitalea, Streptococcus, and Intestinibacter, and higher abundance of potentially beneficial Holdemanella from the Firmicutes phylum.
A standard Mediterranean Diet was not associated with IBS symptom severity, although certain Mediterranean Diet foods were associated with increased IBS symptoms. Our study suggests that standard Mediterranean Diet may not be suitable for all patients with IBS and likely needs to be personalized in those with increased symptoms.❞
In graphical form:
And if you’d like to read more about this (along with more details on which specific foods to include or exclude to get these results), you can do so…
- The study itself (full article): The Association Between a Mediterranean Diet and Symptoms of Irritable Bowel Syndrome
- Dr. Mayer’s blog (lay explanation): The Benefits of a Modified Mediterranean Diet for Irritable Bowel Syndrome
Want to know more?
Dr. Mayer offers many resources, including a blog, books, recipes, podcasts, and even a YouTube channel:





