This salt alternative could help reduce blood pressure. So why are so few people using it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One in three Australian adults has high blood pressure (hypertension). Excess salt (sodium) increases the risk of high blood pressure so everyone with hypertension is advised to reduce salt in their diet.
But despite decades of strong recommendations we have failed to get Australians to cut their intake. It’s hard for people to change the way they cook, season their food differently, pick low-salt foods off the supermarket shelves and accept a less salty taste.
Now there is a simple and effective solution: potassium-enriched salt. It can be used just like regular salt and most people don’t notice any important difference in taste.
Switching to potassium-enriched salt is feasible in a way that cutting salt intake is not. Our new research concludes clinical guidelines for hypertension should give patients clear recommendations to switch.
What is potassium-enriched salt?
Potassium-enriched salts replace some of the sodium chloride that makes up regular salt with potassium chloride. They’re also called low-sodium salt, potassium salt, heart salt, mineral salt, or sodium-reduced salt.
Potassium chloride looks the same as sodium chloride and tastes very similar.
Potassium-enriched salt works to lower blood pressure not only because it reduces sodium intake but also because it increases potassium intake. Insufficient potassium, which mostly comes from fruit and vegetables, is another big cause of high blood pressure.
What is the evidence?
We have strong evidence from a randomised trial of 20,995 people that switching to potassium-enriched salt lowers blood pressure and reduces the risks of stroke, heart attacks and early death. The participants had a history of stroke or were 60 years of age or older and had high blood pressure.
An overview of 21 other studies suggests much of the world’s population could benefit from potassium-enriched salt.
The World Health Organisation’s 2023 global report on hypertension highlighted potassium-enriched salt as an “affordable strategy” to reduce blood pressure and prevent cardiovascular events such as strokes.
What should clinical guidelines say?
We teamed up with researchers from the United States, Australia, Japan, South Africa and India to review 32 clinical guidelines for managing high blood pressure across the world. Our findings are published today in the American Heart Association’s journal, Hypertension.
We found current guidelines don’t give clear and consistent advice on using potassium-enriched salt.
While many guidelines recommend increasing dietary potassium intake, and all refer to reducing sodium intake, only two guidelines – the Chinese and European – recommend using potassium-enriched salt.
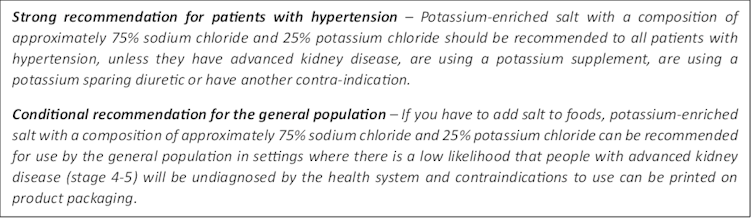
To help guidelines reflect the latest evidence, we suggested specific wording which could be adopted in Australia and around the world:
Why do so few people use it?
Most people are unaware of how much salt they eat or the health issues it can cause. Few people know a simple switch to potassium-enriched salt can help lower blood pressure and reduce the risk of a stroke and heart disease.
Limited availability is another challenge. Several Australian retailers stock potassium-enriched salt but there is usually only one brand available, and it is often on the bottom shelf or in a special food aisle.
Potassium-enriched salts also cost more than regular salt, though it’s still low cost compared to most other foods, and not as expensive as many fancy salts now available.

Jimmy Dean/Unsplash
A 2021 review found potassium-enriched salts were marketed in only 47 countries and those were mostly high-income countries. Prices ranged from the same as regular salt to almost 15 times greater.
Even though generally more expensive, potassium-enriched salt has the potential to be highly cost effective for disease prevention.
Preventing harm
A frequently raised concern about using potassium-enriched salt is the risk of high blood potassium levels (hyperkalemia) in the approximately 2% of the population with serious kidney disease.
People with serious kidney disease are already advised to avoid regular salt and to avoid foods high in potassium.
No harm from potassium-enriched salt has been recorded in any trial done to date, but all studies were done in a clinical setting with specific guidance for people with kidney disease.
Our current priority is to get people being managed for hypertension to use potassium-enriched salt because health-care providers can advise against its use in people at risk of hyperkalemia.
In some countries, potassium-enriched salt is recommended to the entire community because the potential benefits are so large. A modelling study showed almost half a million strokes and heart attacks would be averted every year in China if the population switched to potassium-enriched salt.
What will happen next?
In 2022, the health minister launched the National Hypertension Taskforce, which aims to improve blood pressure control rates from 32% to 70% by 2030 in Australia.
Potassium-enriched salt can play a key role in achieving this. We are working with the taskforce to update Australian hypertension management guidelines, and to promote the new guidelines to health professionals.
In parallel, we need potassium-enriched salt to be more accessible. We are engaging stakeholders to increase the availability of these products nationwide.
The world has already changed its salt supply once: from regular salt to iodised salt. Iodisation efforts began in the 1920s and took the best part of 100 years to achieve traction. Salt iodisation is a key public health achievement of the last century preventing goitre (a condition where your thyroid gland grows larger) and enhancing educational outcomes for millions of the poorest children in the world, as iodine is essential for normal growth and brain development.
The next switch to iodised and potassium-enriched salt offers at least the same potential for global health gains. But we need to make it happen in a fraction of the time.
Xiaoyue Xu (Luna), Scientia Lecturer, UNSW Sydney; Alta Schutte, SHARP Professor of Cardiovascular Medicine, UNSW Sydney, and Bruce Neal, Executive Director, George Institute Australia, George Institute for Global Health
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tight Hamstrings? Here’s A Test To Know If It’s Actually Your Sciatic Nerve
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tight hamstrings are often not actually due to hamstring issues, but rather, are often being limited by the sciatic nerve. This video offers a home test to determine if the sciatic nerve is causing mobility problems (and how to improve it, if so):
The Connection
Try this test:
- Sit down with a slumped posture.
- Extend one leg with the ankle flexed.
- Note any stretching or pulling sensation behind the knee or in the calf.
- Bring your head down to your chest
If this increases the sensation, it likely indicates sciatic nerve involvement.
If only the hamstrings are tight, head movement won’t change the stretch sensation.
This is because the nervous system is a continuous structure, so head movement can affect nerve tension throughout the body. While this can cause problems, it can also be integral in the solution. Here are two ways:
- Flossing method: sit with “poor” slumped posture, extend the knee, keep the ankle flexed, and lift the head to relieve nerve tension. This movement helps the sciatic nerve slide without stretching it.
- Even easier method: lie on your back, grab behind the knee, and extend the leg while extending the neck. This position avoids compression in the gluteal area, making it suitable for severely compromised nerves. Perform the movement without significant stretching or pain.
In both cases: move gently to avoid straining the nerve, which can worsen muscle tension. Do 10 repetitions per leg, multiple times a day; after a week, increase to 20 reps.
A word of caution: speak with your doctor before trying these exercises if you have underlying neurological diseases, cut or infected nerves, or other severe conditions.
For more on all of this, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Exercises for Sciatica Pain Relief
Take care!
Share This Post
-
Strong At Every Age: 15 Habits To Level Up Your Health & Fitness
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not every increase in health and fitness needs to look like a training montage from the “Rocky” movies!
Making progress every day
We’ll not keep the 15 habits a secret; they are:
- Follow the one-minute rule: commit to just one minute of action—this makes starting easier, and often you’ll end up doing more once you’ve got started.
- Make the habit exciting: add fun elements to make the habit more enjoyable, like using new gear or accessories.
- Do it first: prioritize new habits by doing them early in the day to ensure they get done.
- Share the love: pair new habits with activities you already enjoy, where practical, to do “temptation bundling”.
- Embrace the uncomfortable: get used to discomfort daily to grow and build resilience for bigger changes.
- Do as little as possible: start small with habits, to minimize resistance and focus on consistency.
- Think how to be lazy: simplify processes and use shortcuts; there are no extra prizes for it having been difficult!
- Make the appointment: schedule habits with set dates and times, to increase accountability.
- Let habits evolve: adapt habits to fit current circumstances; that way you can still stay consistent over time.
- Plan ahead: prepare in advance to avoid setbacks—what could stop you from succeeding, and how can you pre-empt that?
- Pause to reflect: regularly evaluate what works and what doesn’t, to adjust and improve.
- Shut off your brain: avoid overthinking and start taking action now, not later, to build momentum.
- Question and learn: stay curious and open to learning, or else you will plateau quickly!
- Ask why: understand the deeper reasons behind any resistance, and make clear for yourself the value of the habit.
- Love your failures: embrace any setbacks as learning opportunities and, as such, stepping stones to success.
For more on all of each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Really Pick Up (And Keep!) Those Habits
Take care!
Share This Post
-
What Are Nootropics, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What are nootropics, really?
A nootropic is anything that functions as a cognitive enhancer—in other words, improves our brainpower.
These can be sensationalized as “smart drugs”, misrepresented excitingly in science fiction, meme-ified in the mundane (“but first, coffee”), and reframed entirely, (“exercise is the best nootropic”).
So, clearly, “nootropics” can mean a lot of different things. Let’s look at some of the main categories…
The neurochemical modulators
These are what often get called “smart drugs”. They are literally drugs (have a chemical effect on the body that isn’t found in our diet), and they affect the levels of certain neurotransmitters in the brain, such as by:
- Adding more of that neurotransmitter (simple enough)
- Decreasing the rate at which we lose that neurotransmitter (re-uptake inhibitors)
- Antagonizing an unhelpful neurotransmitter (doing the opposite thing to it)
- Blocking an unhelpful neurotransmitter (stopping the receptors from receiving it)
“Unhelpful” here is relative and subjective, of course. We need all the neurotransmitters that are in our brain, after all, we just don’t need all of them all the time.
Examples: modafinil, a dopamine re-uptake inhibitor (mostly prescribed for sleep disorders), reduces the rate at which our brains scrub dopamine, resulting in a gradual build-up of dopamine that we naturally produced, so we get to enjoy that dopamine for longer. This will tend to promote wakefulness, and may also help with problem-solving and language faculties—as well as giving a mood boost. In other words, all things that dopamine is used for. Mirtazaрine, an adrenoreceptor agonist (mostly prescribed as an antidepressant), increases noradrenergic neurotransmission, thus giving many other brain functions a boost.
Why it works: our brains need healthy levels of neurotransmitters, in order to function well. Those levels are normally self-regulating, but can become depleted in times of stress or fatigue, for example.
The metabolic brain boosters
These are the kind of things that get included in nootropic stacks (stack = a collection of supplements and/or drugs that complement each other and are taken together—for example, a multivitamin tablet could be described as a vitamin stack) even though they have nothing specifically relating them to brain function. Why are they included?
The brain needs so much fuel. Metabolically speaking, it’s a gas-guzzler. It’s the single most resource-intensive organ of our body, by far. So, metabolic brain boosters tend to:
- Increase blood flow
- Increase blood oxygenation
- Increase blood general health
- Improve blood pressure (this is relative and subjective, since very obviously there’s a sweet spot)
Examples: B-vitamins. Yep, it can be that simple. A less obvious example might be Co-enzyme Q10, which supports energy production on a cellular level, and good cardiovascular health.
Why it works: you can’t have a healthy brain without a healthy heart!
We are such stuff as brains are made of
Our brains are made of mostly fat, water, and protein. But, not just any old fat and protein—we’re at least a little bit special! So, brain-food foods tend to:
- Give the brain the fats and proteins it’s made of
- Give the brain the stuff to make the fats and proteins it’s made of (simpler fats, and amino acids)
- Give the brain hydration! Just having water, and electrolytes as appropriate, does this
Examples: healthy fats from nuts, seeds, and seafood; also, a lot of phytonutrients from greens and certain fruits. Long-time subscribers may remember our article “Brain Food: The Eyes Have It!” on the importance of dietary lutein in reducing Alzheimer’s risk, for example
Why it works: this is matter of structural upkeep and maintenance—our brains don’t work fabulously if deprived of the very stuff they’re made of! Especially hydration is seriously underrated as a nootropic factor, by the way. Most people are dehydrated most of the time, and the brain dehydrates quickly. Fortunately, it rehydrates quickly as well when we take hydrating liquids.
Weird things that sound like ingredients in a witch’s potion
These are too numerous and too varied in how they work to cover here, but they do appear a lot in nootropic stacks and in popular literature on the subject.
Often they work by one of the mechanisms described above; sometimes we’re not entirely sure how they work, and have only measured their effects sufficiently to know that, somehow, they do work.
Examples: panax ginseng is one of the best-studied examples that still remains quite mysterious in many aspects of its mechanism. Lion’s Mane (the mushroom, not the jellyfish or the big cat hairstyle), meanwhile, is known to contain specific compounds that stimulate healthy brain cell growth.
Why it works: as we say, it varies so much from on ingredient to another in this category, so… Watch out for our Research Review Monday features, as we’ll be covering some of these in the coming weeks!
(PS, if there’s any you’d like us to focus on, let us know! We always love to hear from you. You can hit reply to any of our emails, or use the handy feedback widget at the bottom)
Share This Post
Related Posts
-
Aging with Grace – by Dr. David Snowdon
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this book is not: a book about Christianity. Don’t worry, we didn’t suddenly change the theme of 10almonds.
Rather, what this book is: a book about a famous large (n=678) study into the biology of aging, that took a population sample of women who had many factors already controlled-for, e.g. they ate the same food, had the same schedule, did the same activities, etc—for many years on end. In other words, a convent of nuns.
This allowed for a lot more to be learned about other factors that influence aging, such as:
- Heredity / genetics in general
- Speaking more than one language
- Supplementing with vitamins or not
- Key adverse events (e.g. stroke)
- Key chronic conditions (e.g. depression)
The book does also cover (as one might expect) the role that community and faith can play in healthy longevity, but since the subjects were 678 communally-dwelling people of faith (thus: no control group of faithless loners), this aspect is discussed only in anecdote, or in reference to other studies.
The author of this book, by the way, was the lead researcher of the study, and he is a well-recognised expert in the field of Alzheimer’s in particular (and Alzheimer’s does feature quite a bit throughout).
The writing style is largely narrative, and/but with a lot of clinical detail and specific data; this is by no means a wishy-washy book.
Bottom line: if you’d like to know what nuns were doing in the 1980s to disproportionally live into three-figure ages, then this book will answer those questions.
Click here to check out Aging with Grace, and indeed age with grace!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Science-Based Alternative Pain Relief
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Painkillers Aren’t Helping, These Things Might
Maybe you want to avoid painkillers, or maybe you’ve already maxed out what you can have, and want more options as an extra help against the pain.
Today we’ll look at some science-backed alternative pain relief methods:
First: when should we try to relieve pain?
There is no such thing as “this pain is not too much”. The correct amount of pain is zero. Maybe your body won’t let you reach zero, but more than that is “too much” already.
You don’t have to be suffering off the scale to deserve relief from pain!
So: if it hurts, then if you can safely get relief from the pain, it’s already wise to do so.
A couple of things we covered previously
CBD and THC are technically drugs, but are generally considered “alternative” pain relief, so we’ll give a quick mention here:
Short version:
- CBD can treat some kinds of treatment-resistant pain well (others, not so much—try it and find out if it works for you)
- THC can offer some people respite not found from other methods—but beware, because there are many health risks to consider.
Acupuncture
Pain relief appears to be its strongest suit:
Pinpointing The Usefulness Of Acupuncture
Cloves
Yes, just like you can get from the supermarket.
In its medicinal uses, it’s most well-known as a toothache remedy, but it has a local analgesic effect wherever you put it (i.e., apply it topically to where the pain is), thanks to its eugenol content:
Boswellia (frankincense)
The resin of the Boswellia serrata tree, this substance has an assortment of medicinal properties, including pain relief, anti-inflammatory effect, and psychoactive (anxiolytic and antidepressant) effects:
Frankincense is psychoactive: new class of antidepressants might be right under our noses
And as for physical pain? Here’s how it faired against the pain of osteoarthritis (and other OA symptoms, but we’re focusing on pain today), for example:
Here’s an example product on Amazon, but feel free to shop around as there are many options, including for example this handy roll-on
Further reading
Intended for chronic pain, but in large part applicable to acute pain also:
Managing Chronic Pain (Realistically!)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tasty Tofu Scramble
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’re trying to eat more plant-based, this is a great way to enjoy a culinary experience that hits the same notes as scrambled egg, with many similar nutritional benefits too, and some of its own!
You will need
- 1 cup (10oz) silken tofu
- ¼ bulb garlic, crushed
- 1 tbsp nutritional yeast
- 2 tsp chia seeds
- 2 tsp dried thyme, or 1 tsp fresh thyme, stripped (i.e. pulled off the stalks)
- 2 tsp turmeric
- 2 tsp black pepper, coarse ground
- 1 tsp red chili flakes
- ½ tsp MSG, or 1 tsp low-sodium salt
- Extra virgin olive oil, for frying
Method
(we suggest you read everything at least once before doing anything)
1) Heat a skillet with olive oil in it; if you want a low-calorie option, you can use quite little oil here; the tofu is a lot more forgiving than egg in this regard and is almost impossible to burn unless you actively try. If you don’t want a low-calorie option, feel free to be generous with the oil if you prefer; it’ll go into the tofu and make it fattier, much like egg.
2) Add the tofu. You can just drop it (carefully) straight in; you don’t need to press it or anything.
3) Scramble it with a spatula, just the same as you would if it were egg.
4) Add the rest of the ingredients, mixing them in as you continue to scramble it, until it reaches the desired consistency.
5) Serve! Serving it on wholegrain toast is a great option—but this dish can also be enjoyed any other way you might use scrambled eggs (including for making
egg-friedtofu-fried rice; just stir it into our Tasty Versatile Rice recipe!)Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Plant vs Animal Protein: Head to Head
- Black Pepper’s Impressive Anti-Cancer Arsenal
- Capsaicin For Weight Loss And Against Inflammation
- The Many Health Benefits Of Garlic
- Why Curcumin (Turmeric) Is Worth Its Weight In Gold
- If You’re Not Taking Chia, You’re Missing Out
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: