Wakefulness, Cognitive Enhancement, AND Improved Mood?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Old Drug, New Tricks?
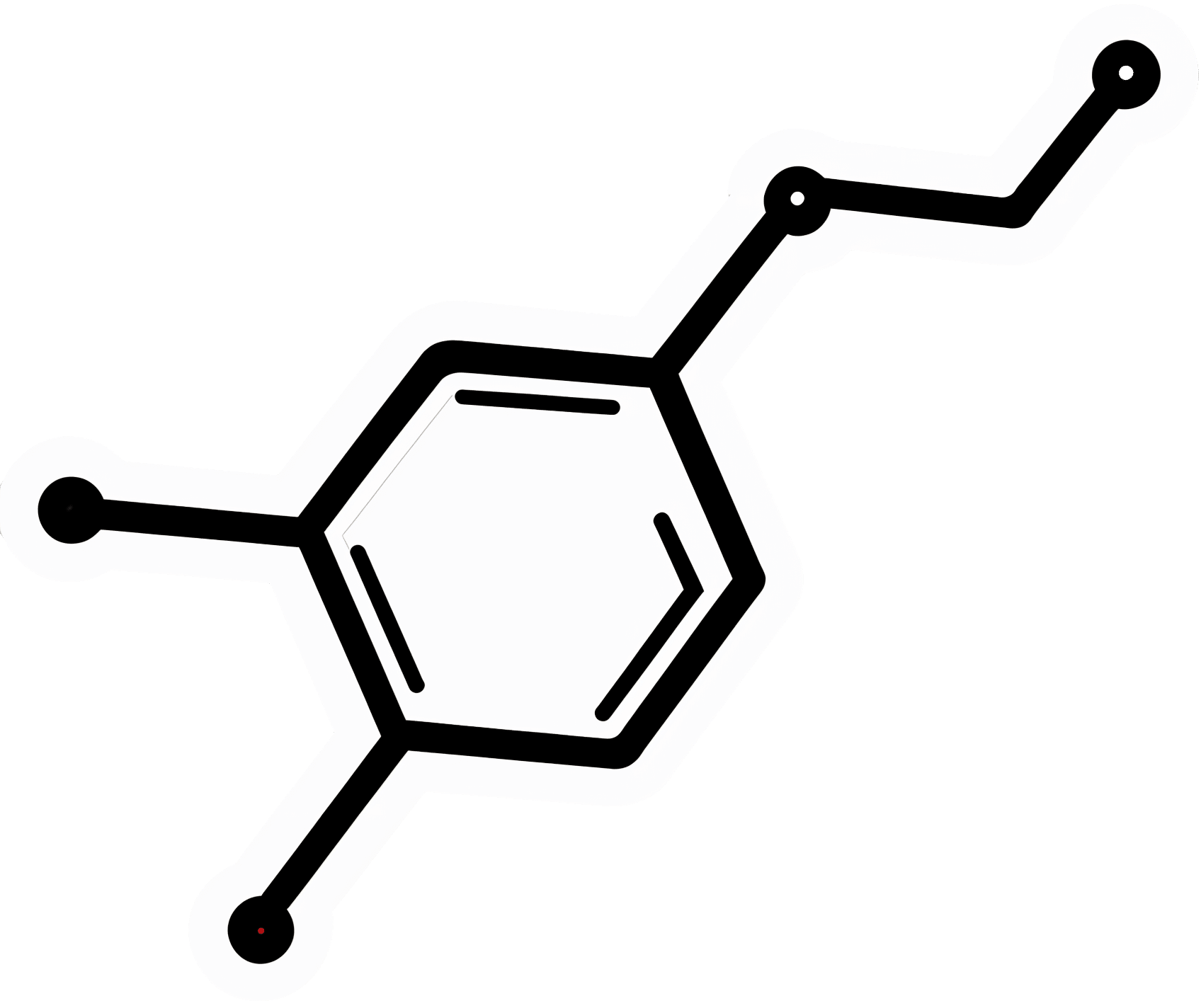
Modafinil (also known by brand names including Modalert and Provigil) is a dopamine uptake inhibitor.
What does that mean? It means it won’t put any extra dopamine in your brain, but it will slow down the rate at which your brain removes naturally-occuring dopamine.
The result is that your brain will get to make more use of the dopamine it does have.
(dopamine is a neutrotransmitter that allows you to feel wakeful and happy, and perform complex cognitive tasks)
Modafinil is prescribed for treatment of excessive daytime sleepiness. Often that’s caused by shift work sleep disorder, sleep apnea, restless leg syndrome, or narcolepsy.
Read: Overview of the Clinical Uses, Pharmacology, and Safety of Modafinil
Many studies done on humans (rather than rats) have been military experiments to reduce the effects of sleep deprivation:
Click Here To See A Military Study On Modafinil!
They’ve found modafinil to be helpful, and more effective and more long-lasting than caffeine, without the same “crash” later. This is for two reasons:
1) while caffeine works by blocking adenosine (so you don’t feel how tired you are) and by constricting blood vessels (so you feel more ready-for-action), modafinil works by allowing your brain to accumulate more dopamine (so you’re genuinely more wakeful, and you get to keep the dopamine)
2) the biological half-life of modafinil is 12–15 hours, as opposed to 4–8 hours* for caffeine.
*Note: a lot of sources quote 5–6 hours for caffeine, but this average is misleading. In reality, we are each genetically predetermined to be either a fast caffeine metabolizer (nearer 4 hours) or a slow caffeine metabolizer (nearer 8 hours).
What’s a biological half-life (also called: elimination half-life)?
A substance’s biological half-life is the time it takes for the amount in the body to be reduced by exactly half.
For example: Let’s say you’re a fast caffeine metabolizer and you have a double-espresso (containing 100mg caffeine) at 8am.
By midday, you’ll have 50mg of caffeine left in your body. So far, so simple.
By 4pm you might expect it to be gone, but instead you have 25mg remaining (because the amount halves every four hours).
By 8pm, you have 12.5mg remaining.
When midnight comes and you’re tucking yourself into bed, you still have 6.25mg of caffeine remaining from your morning coffee!
Use as a nootropic
Many healthy people who are not sleep-deprived use modafinil “off-label” as a nootropic (i.e., a cognitive enhancer).
Read: Modafinil for cognitive neuroenhancement in healthy non-sleep-deprived subjects: A systematic review
Important Note: modafinil is prescription-controlled, and only FDA-approved for sleep disorders.
To get around this, a lot of perfectly healthy biohackers describe the symptoms of sleep pattern disorder to their doctor, to get a prescription.
We do not recommend lying to your healthcare provider, and nor do we recommend turning to the online “grey market”.
Such websites often use anonymized private doctors to prescribe on an “informed consent” basis, rather than making a full examination. Those websites then dispense the prescribed medicines directly to the patient with no further questions asked (i.e. very questionable practices).
Caveat emptor!
A new mood-brightener?
Modafinil was recently tested head-to-head against Citalapram for the treatment of depression, and scored well:
See its head-to-head scores here!
How does it work? Modafinil does for dopamine what a lot of anti-depressants do for serotonin. Both dopamine and serotonin promote happiness and wakefulness.
This is very promising, especially as modafinil (in most people, at least) has fewer unwanted side-effects than a lot of common anti-depressant medications.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Needle Pain Is a Big Problem for Kids. One California Doctor Has a Plan.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Almost all new parents go through it: the distress of hearing their child scream at the doctor’s office. They endure the emotional torture of having to hold their child down as the clinician sticks them with one vaccine after another.
“The first shots he got, I probably cried more than he did,” said Remy Anthes, who was pushing her 6-month-old son, Dorian, back and forth in his stroller in Oakland, California.
“The look in her eyes, it’s hard to take,” said Jill Lovitt, recalling how her infant daughter Jenna reacted to some recent vaccines. “Like, ‘What are you letting them do to me? Why?’”
Some children remember the needle pain and quickly start to internalize the fear. That’s the fear Julia Cramer witnessed when her 3-year-old daughter, Maya, had to get blood drawn for an allergy test at age 2.
“After that, she had a fear of blue gloves,” Cramer said. “I went to the grocery store and she saw someone wearing blue gloves, stocking the vegetables, and she started freaking out and crying.”
Pain management research suggests that needle pokes may be children’s biggest source of pain in the health care system. The problem isn’t confined to childhood vaccinations either. Studies looking at sources of pediatric pain have included children who are being treated for serious illness, have undergone heart surgeries or bone marrow transplants, or have landed in the emergency room.
“This is so bad that many children and many parents decide not to continue the treatment,” said Stefan Friedrichsdorf, a specialist at the University of California-San Francisco’s Stad Center for Pediatric Pain, speaking at the End Well conference in Los Angeles in November.
The distress of needle pain can follow children as they grow and interfere with important preventive care. It is estimated that a quarter of all adults have a fear of needles that began in childhood. Sixteen percent of adults refuse flu vaccinations because of a fear of needles.
Friedrichsdorf said it doesn’t have to be this bad. “This is not rocket science,” he said.
He outlined simple steps that clinicians and parents can follow:
- Apply an over-the-counter lidocaine, which is a numbing cream, 30 minutes before a shot.
- Breastfeed babies, or give them a pacifier dipped in sugar water, to comfort them while they’re getting a shot.
- Use distractions like teddy bears, pinwheels, or bubbles to divert attention away from the needle.
- Don’t pin kids down on an exam table. Parents should hold children in their laps instead.
At Children’s Minnesota, Friedrichsdorf practiced the “Children’s Comfort Promise.” Now he and other health care providers are rolling out these new protocols for children at UCSF Benioff Children’s Hospitals in San Francisco and Oakland. He’s calling it the “Ouchless Jab Challenge.”
If a child at UCSF needs to get poked for a blood draw, a vaccine, or an IV treatment, Friedrichsdorf promises, the clinicians will do everything possible to follow these pain management steps.
“Every child, every time,” he said.
It seems unlikely that the ouchless effort will make a dent in vaccine hesitancy and refusal driven by the anti-vaccine movement, since the beliefs that drive it are often rooted in conspiracies and deeply held. But that isn’t necessarily Friedrichsdorf’s goal. He hopes that making routine health care less painful can help sway parents who may be hesitant to get their children vaccinated because of how hard it is to see them in pain. In turn, children who grow into adults without a fear of needles might be more likely to get preventive care, including their yearly flu shot.
In general, the onus will likely be on parents to take a leading role in demanding these measures at medical centers, Friedrichsdorf said, because the tolerance and acceptance of children’s pain is so entrenched among clinicians.
Diane Meier, a palliative care specialist at Mount Sinai, agrees. She said this tolerance is a major problem, stemming from how doctors are usually trained.
“We are taught to see pain as an unfortunate, but inevitable side effect of good treatment,” Meier said. “We learn to repress that feeling of distress at the pain we are causing because otherwise we can’t do our jobs.”
During her medical training, Meier had to hold children down for procedures, which she described as torture for them and for her. It drove her out of pediatrics. She went into geriatrics instead and later helped lead the modern movement to promote palliative care in medicine, which became an accredited specialty in the United States only in 2006.
Meier said she thinks the campaign to reduce needle pain and anxiety should be applied to everyone, not just to children.
“People with dementia have no idea why human beings are approaching them to stick needles in them,” she said. And the experience can be painful and distressing.
Friedrichsdorf’s techniques would likely work with dementia patients, too, she said. Numbing cream, distraction, something sweet in the mouth, and perhaps music from the patient’s youth that they remember and can sing along to.
“It’s worthy of study and it’s worthy of serious attention,” Meier said.
This article is from a partnership that includes KQED, NPR, and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Putting a Halt to Feeling Lost, Anxious, Stressed & Unhappy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Starting From the Middle
Today’s video (below) dives straight into the heart of the issue, examining the victim mindset, with Dr. Gabor Maté immediately, and quite vulnerably, sharing his personal experiences conquering feelings of despair and anxiety.
As one of the comments on the video says, Dr. Maté is a “person who teaches about something because they experience it themselves”. And it shows through his approach.
With raw honesty, Dr. Maté empathizes with those grappling with inner turmoil, offering hope by emphasizing the power of healing in the present moment.
What is His Method?
Explained simply, Dr. Maté urges individuals to seek trauma-informed care and therapies that address underlying wounds; he emphasizes the pitfalls of relying solely on medication, and instead highlights the idea that triggers can be seen as opportunities for self-reflection and growth. He urges individuals to approach their triggers with compassionate curiosity rather than self-judgment.
In short, Dr Maté’s empathetic approach immediately calms the viewer, whilst providing knowledge crucial to self-improvement.
Let this video act as a reminder that we should take our mental health as seriously as our general health.
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Share This Post
-
Blood-Brain Barrier Breach Blamed For Brain-Fog
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Move Over, Leaky Gut. Now It’s A Leaky Brain.
…which is not a headline that promises good news, and indeed, the only good news about this currently is “now we know another thing that’s happening, and thus can work towards a treatment for it”.
Back in February (most popular media outlets did not rush to publish this, as it rather goes against the narrative of “remember when COVID was a thing?” as though the numbers haven’t risen since the state of emergency was declared over), a team of Irish researchers made a discovery:
❝For the first time, we have been able to show that leaky blood vessels in the human brain, in tandem with a hyperactive immune system may be the key drivers of brain fog associated with long covid❞
~ Dr. Matthew Campbell (one of the researchers)
Let’s break that down a little, borrowing some context from the paper itself:
- the leaky blood vessels are breaching the blood-brain-barrier
- that’s a big deal, because that barrier is our only filter between our brain and Things That Definitely Should Not Go In The Brain™
- a hyperactive immune system can also be described as chronic inflammation
- in this case, that includes chronic neuroinflammation which, yes, is also a major driver of dementia
You may be wondering what COVID has to do with this, and well:
- these blood-brain-barrier breaches were very significantly associated (in lay terms: correlated, but correlated is only really used as an absolute in write-ups) with either acute COVID infection, or Long Covid.
- checking this in vitro, exposure of brain endothelial cells to serum from patients with Long Covid induced the same expression of inflammatory markers.
How important is this?
As another researcher (not to mention: professor of neurology and head of the school of medicine at Trinity) put it:
❝The findings will now likely change the landscape of how we understand and treat post-viral neurological conditions.
It also confirms that the neurological symptoms of long covid are measurable with real and demonstrable metabolic and vascular changes in the brain.❞
~ Dr. Colin Doherty (see mini-bio above)
You can read a pop-science article about this here:
Irish researchers discover underlying cause of “brain fog” linked with long covid
…and you can read the paper in full here:
Want to stay safe?
Beyond the obvious “get protected when offered boosters/updates” (see also: The Truth About Vaccines), other good practices include the same things most people were doing when the pandemic was big news, especially avoiding enclosed densely-populated places, washing hands frequently, and looking after your immune system. For that latter, see also:
Beyond Supplements: The Real Immune-Boosters!
Take care!
Share This Post
- the leaky blood vessels are breaching the blood-brain-barrier
Related Posts
-
From Lupus To Arthritis: New Developments
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This week’s health news round-up highlights some things that are getting better, and some things that are getting worse, and how to be on the right side of both:
New hope for lupus sufferers
Lupus is currently treated mostly with lifelong medications to suppress the immune system, which is not only inconvenient, but also can leave people more open to infectious diseases. The latest development uses CAR T-cell technology (as has been used in cancer treatment for a while) to genetically modify cells to enable the body’s own immune system to behave properly:
Read in full: Exciting new lupus treatment could end need for lifelong medication
Related: How to Prevent (Or Reduce The Severity Of) Inflammatory Diseases
It’s in the hips
There are a lot of different kinds of hip replacements, and those with either delta ceramic or oxidised zirconium head with a highly cross-linked polyethylene liner/cup have the lowest risk of need for revision in the 15 years after surgery. This is important, because obviously, once it’s in there, you want it to be able to stay in there and not have to be touched again any time soon:
Read in full: Study identifies hip implant materials with the lowest risk of needing revision
Related: Nobody Likes Surgery, But Here’s How To Make It Much Less Bad
Sooner is better than later
Often, people won’t know about an unwanted pregnancy in the first six weeks, but for those who are able to catch it early, Very Early Medical Abortion (VEMA) offers a safe an effective way of doing so, with success rate being linked to earliness of intervention:
Read in full: Very early medication abortion is effective and safe, study finds
Related: What Might A Second Trump Presidency Look Like for Health Care?
Increased infectious disease risks from cattle farms
Many serious-to-humans infectious diseases enter the human population via the animal food chain, and in this case, bird flu becoming more rampant amongst cows is starting to pose a clear threat to humans, so this is definitely something to be aware of:
Read in full: Bird flu infects 1 in 14 dairy workers exposed; CDC urges better protections
Related: With Only Gloves To Protect Them, Farmworkers Say They Tend Sick Cows Amid Bird Flu
Herald of woe
Gut health affects most of the rest of health, and there are a lot of links between gut and bone health. In this case, an association has been found between certain changes in the gut microbiome, and subsequent onset of rheumatoid arthritis:
Read in full: Changes in gut microbiome could signal onset of rheumatoid arthritis
Related: Stop Sabotaging Your Gut
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
28-Day FAST Start Day-by-Day – by Gin Stephens
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We have previously reviewed Gin Stephens’ other book, “Fast. Feast. Repeat.”, so what’s so special about this one that it deserves reviewing too?
This one is all about troubleshooting the pitfalls that many people find when taking up intermittent fasting.
To be clear: the goal here is not a “28 days and yay you did it, put that behind you now”, but rather “28 days and you are now intermittently fasting easily each day and can keep it up without difficulty”. As for the difficulties that may arise early in the 28 days…
Not just issues of willpower, but also the accidental breaks. For example, some artificial sweeteners, while zero-calorie, trigger an insulin response, which breaks the fast on the metabolic level (avoiding that is the whole point of IF). Lots of little tips like that peppered through the book help the reader to stop accidentally self-sabotaging their progress.
The author does talk about psychological issues too, and also how it will feel different at first while the liver is adapting, than later when it has already depleted its glycogen reserves and the body must burn body fat instead. Information like that makes it easier to understand that some initial problems (hunger, getting “hangry”, feeling twitchy, or feeling light-headed) will last only a few weeks and then disappear.
So, understanding things like that makes a big difference too.
The style of the book is simple and clear pop-science, with lots of charts and bullet points and callout-boxes and the like; it makes for very easy reading, and very quick learning of all the salient points, of which there are many.
Bottom line: if you’ve tried intermittent fasting but struggled to make it stick, this book can help you get to where you want to be.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tasty Tabbouleh with Tahini
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tabbouleh is a salad, but it’s not “just a salad”. It’s a special kind of salad that’s as exciting for the tastebuds as it is healthy for the body and brain. Its core ingredients have been traditional for about a dozen generations, and seasonings are always a personal matter (not to mention that Lebanese tabbouleh-makers centuries ago might not have used miso and nooch, as we will today), but the overall feel of the Gestalt of tabbouleh seasonings remains the same, and this recipe is true to that.
You will need
For the tabbouleh:
- 1 cup bulgur wheat
- 1 cup plum tomatoes, chopped
- 1 cucumber, peeled and chopped (add the peel to a jug of water and put it in the fridge; this will be refreshing cucumber water later!)
- 1 cup chickpeas, cooked without salt
- 1/2 cup parsley, chopped
- 1/2 cup mint, chopped
- 2 spring onions, finely chopped
- 2oz fresh lemon juice
- 1 tsp white miso paste
- 1 tsp garlic powder
- 1 tsp ground cumin
- 1 tsp ground celery seeds
- 1 tsp ground nigella seeds
- 1 tsp ground black pepper
- 1 tsp MSG, or 1/2 tsp low sodium salt (you can find it in supermarkets, the sodium chloride is cut with potassium chloride to make it have less sodium and more potassium)
- 1 tbsp nutritional yeast (nooch), ground (it comes in flakes; you will have to grind it in a spice grinder or with a pestle and mortar)
For the tahini sauce:
- 3 garlic cloves, crushed
- 3 tbsp tahini
- 1 tbsp fresh lemon juice
- 1 tbsp white miso paste
- 1 tsp ground cumin
To serve:
- A generous helping of leafy greens; we recommend collard greens, but whatever works for you is good; just remember that dark green is best. Consider cavolo nero, or even kale if that’s your thing, but to be honest this writer doesn’t love kale
- 1 tsp coarsely ground nigella seeds
- Balsamic vinegar, ideally aged balsamic vinegar (this is thicker and sweeter, but unlike most balsamic vinegar reductions, doesn’t have added sugar).
Method
(we suggest you read everything at least once before doing anything)
1) Rinse the bulgur wheat and then soak it in warm water. There is no need to boil it; the warm water is enough to soften it and you don’t need to cook it (bulgur wheat has already been parboiled before it got to you).
2) While you wait, take a small bowl and mix the rest of the ingredients from the tabbouleh section (so, the lemon juice, miso paste, and all those ground spices and MSG/salt and ground nutritional yeast); you’re making a dressing out of all the ingredients here.
3) When the bulgur wheat is soft (expect it to take under 15 minutes), drain it and put it in a big bowl. Add the tomatoes, cucumber, chickpeas, parsley, mint, and spring onions. This now technically qualifies as tabbouleh already, but we’re not done.
4) Add the dressing to the tabbouleh and mix thoroughly but gently (you don’t want to squash the tomatoes, cucumber, etc). Leave it be for at least 15 minutes while the flavors blend.
5) Take the “For the tahini sauce” ingredients (all of them) and blend them with 4 oz water, until smooth. You’re going to want to drizzle this sauce, so if the consistency is too thick for drizzling, add a little more water and/or lemon juice (per your preference), 1 tbsp at a time.
6) Roughly chop the leafy greens and put them in a bowl big enough for the tabbouleh to join them there. The greens will serve as a bed for the tabbouleh itself.
7) Drizzle the tahini over the tabbouleh, and drizzle a little of the aged balsamic vinegar too.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: