Our blood-brain barrier stops bugs and toxins getting to our brain. Here’s how it works
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
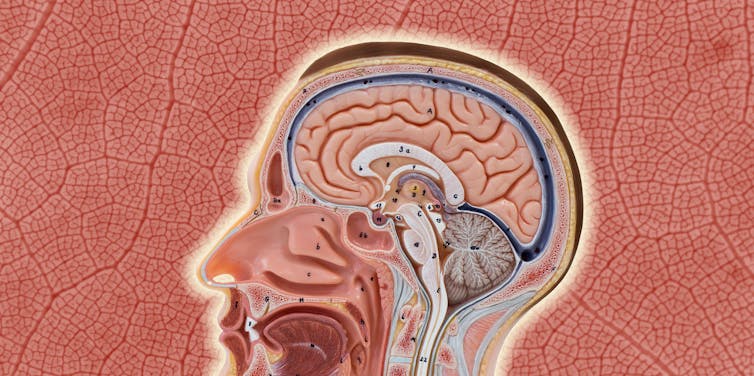
Our brain is an extremely complex and delicate organ. Our body fiercely protects it by holding onto things that help it and keeping harmful things out, such as bugs that can cause infection and toxins.
It does that though a protective layer called the blood-brain barrier. Here’s how it works, and what it means for drug design.
First, let’s look at the circulatory system
Adults have roughly 30 trillion cells in their body. Every cell needs a variety of nutrients and oxygen, and they produce waste, which needs to be taken away.
Our circulatory system provides this service, delivering nutrients and removing waste.
Where the circulatory system meets your cells, it branches down to tiny tubes called capillaries. These tiny tubes, about one-tenth the width of a human hair, are also made of cells.
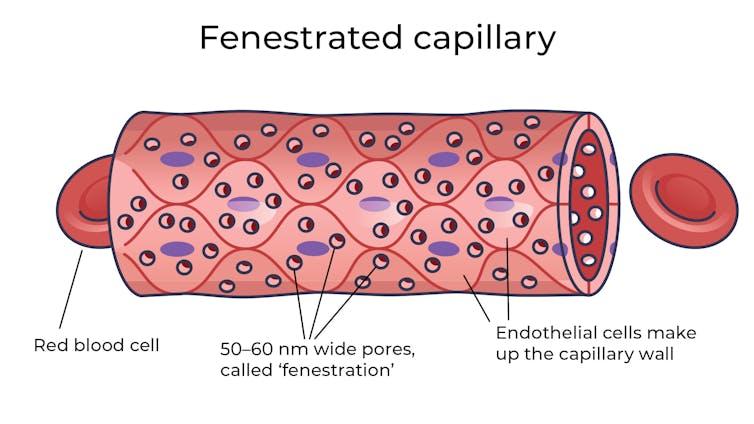
But in most capillaries, there are some special features (known as fenestrations) that allow relatively free exchange of nutrients and waste between the blood and the cells of your tissues.
It’s kind of like pizza delivery
One way to think about the way the circulation works is like a pizza delivery person in a big city. On the really big roads (vessels) there are walls and you can’t walk up to the door of the house and pass someone the pizza.
But once you get down to the little suburban streets (capillaries), the design of the streets means you can stop, get off your scooter and walk up to the door to deliver the pizza (nutrients).
We often think of the brain as a spongy mass without much blood in it. In reality, the average brain has about 600 kilometres of blood vessels.
The difference between the capillaries in most of the brain and those elsewhere is that these capillaries are made of specialised cells that are very tightly joined together and limit the free exchange of anything dissolved in your blood. These are sometimes called continuous capillaries.
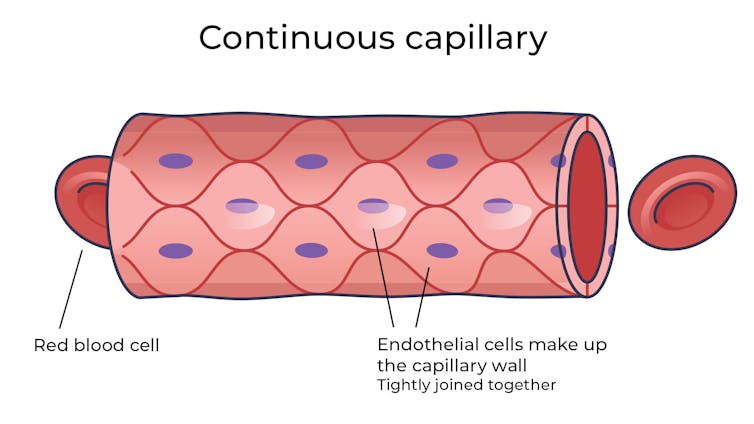
This is the blood brain barrier. It’s not so much a bag around your brain stopping things from getting in and out but more like walls on all the streets, even the very small ones.
The only way pizza can get in is through special slots and these are just the right shape for the pizza box.
The blood brain barrier is set up so there are specialised transporters (like pizza box slots) for all the required nutrients. So mostly, the only things that can get in are things that there are transporters for or things that look very similar (on a molecular scale).
The analogy does fall down a little bit because the pizza box slot applies to nutrients that dissolve in water. Things that are highly soluble in fat can often bypass the slots in the wall.
Why do we have a blood-brain barrier?
The blood brain barrier is thought to exist for a few reasons.
First, it protects the brain from toxins you might eat (think chemicals that plants make) and viruses that often can infect the rest of your body but usually don’t make it to your brain.
It also provides protection by tightly regulating the movement of nutrients and waste in and out, providing a more stable environment than in the rest of the body.
Lastly, it serves to regulate passage of immune cells, preventing unnecessary inflammation which could damage cells in the brain.
What it means for medicines
One consequence of this tight regulation across the blood brain barrier is that if you want a medicine that gets to the brain, you need to consider how it will get in.
There are a few approaches. Highly fat-soluble molecules can often pass into the brain, so you might design your drug so it is a bit greasy.

Another option is to link your medicine to another molecule that is normally taken up into the brain so it can hitch a ride, or a “pro-drug”, which looks like a molecule that is normally transported.
Using it to our advantage
You can also take advantage of the blood brain barrier.
Opioids used for pain relief often cause constipation. They do this because their target (opioid receptors) are also present in the nervous system of the intestines, where they act to slow movement of the intestinal contents.
Imodium (Loperamide), which is used to treat diarrhoea, is actually an opioid, but it has been specifically designed so it can’t cross the blood brain barrier.
This design means it can act on opioid receptors in the gastrointestinal tract, slowing down the movement of contents, but does not act on brain opioid receptors.
In contrast to Imodium, Ozempic and Victoza (originally designed for type 2 diabetes, but now popular for weight-loss) both have a long fat attached, to improve the length of time they stay in the body.
A consequence of having this long fat attached is that they can cross the blood-brain barrier, where they act to suppress appetite. This is part of the reason they are so effective as weight-loss drugs.
So while the blood brain barrier is important for protecting the brain it presents both a challenge and an opportunity for development of new medicines.
Sebastian Furness, ARC Future Fellow, School of Biomedical Sciences, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Lost Connections – by Johann Hari
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Johann Hari had a long journey through (and out of!) depression, and shares his personal findings, including his disappointment with medical options, and a focus on the external factors that lead to depression.
And that’s key to this book—while he acknowledges later in the book that there are physiological factors involved in depression, he wants to look past things we can’t change (like genes accounting for 37% of depression) or things that there may be unwanted side-effects to changing (as in the case of antidepressants, for many people), to things we genuinely can choose.
And no, it’s not a “think yourself happy” book either; rather, it looks at nine key external factorsthat a) influence depression b) can mostly be changed.
If the book has a downside, it’s that the author does tend to extrapolate his own experience a lot more than might be ideal. If SSRIs didn’t help him, they are useless, and also the only kind of antidepressant. If getting into a green space helped him, a Londoner, someone who lives in the countryside will not be depressed in the first place. And so forth. It can also be argued that he cherry-picked data to arrive at some of his pre-decided conclusions. He also misinterprets data sometimes; which is understandable; he is after all a journalist, not a scientist.
Nevertheless, he offers a fresh perspective with a lot of ideas, and whether or not we agree with them all, new ideas tend to be worth reading. And if even one of his nine ideas helps you, that’s a win.
Bottom line: if you’d like to explore the treatment of depression from a direction other than medicalization or psychotherapy, then this is will be a good book for you.
Click here to check out Lost Connections, and reforge yours!
Share This Post
-
Black Forest Chia Pudding
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This pudding tastes so decadent, it’s hard to believe it’s so healthy, but it is! Not only is it delicious, it’s also packed with nutrients including protein, carbohydrates, healthy fats (including omega-3s), fiber, vitamins, minerals, and assorted antioxidant polyphenols. Perfect dessert or breakfast!
You will need
- 1½ cups pitted fresh or thawed-from-frozen cherries
- ½ cup mashed banana
- 3 tbsp unsweetened cocoa powder
- 2 tbsp chia seeds, ground
- Optional: 2 pitted dates, soaked in hot water for 10 minutes and then drained (include these if you prefer a sweeter pudding)
- Garnish: a few almonds, and/or berries, and/or cherries and/or cacao nibs
Method
(we suggest you read everything at least once before doing anything)
1) Blend the ingredients except for the chia seeds and the garnish, with ½ cup of water, until completely smooth
2) Divide into two small bowls or glass jars
3) Add 1 tbsp ground chia seeds to each, and stir until evenly distributed
4) Add the garnish and refrigerate overnight or at least for some hours. There’s plenty of wiggle-room here, so make it at your convenience and serve at your leisure.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Cherries’ Very Healthy Wealth Of Benefits!
- If You’re Not Taking Chia, You’re Missing Out
- Cacao vs Carob – Which is Healthier?
Take care!
Share This Post
-
Foods Linked To Urinary Incontinence In Middle-Age (& Foods That Avert It)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Incontinence is an inconvenience associated with aging, especially for women. Indeed, as the study we’re going to talk about today noted:
❝Estrogen deficiency during menopause, aging, reproductive history, and factors increasing intra-abdominal pressure may lead to structural and functional failure in the pelvic floor.❞
However, that was just the “background”, before they got the study going, because…
❝Lifestyle choices, such as eating behavior, may contribute to pelvic floor disorders. The objective of the study was to investigate associations of eating behavior with symptoms of pelvic floor disorders, that is, stress urinary incontinence, urgency urinary incontinence, fecal incontinence, and constipation or defecation difficulties among middle-aged women.❞
~ Ibid.
How the study went
The researchers examined 1,098 Finnish women aged 47–55. It was a cross-sectional observational study, so no intervention was made, just: gathering data and analysing it. They examined:
- Eating behavior (i.e. what one’s diet is like; their questionnaire was quite comprehensive and the simplified conclusion doesn’t do that justice)
- Food consumption frequency (i.e. temporal patterns of eating)
- Demographic variables (e.g. age, education, etc)
- Gynecological variables (e.g. menopause status, hysterectomy, etc)
- Physical activity variables (e.g. light, moderate, heavy, previous history of no exercise, regular, competitive sport, etc)
With those things taken into account, the researchers crunched the numbers to assess the associations of dietary factors with pelvic floor disorders.
What they found
Adjusting for possible confounding variables…
- those with disordered eating patterns (e.g. overeating, restrictive eating, swinging between the two behaviors) were 50% higher chance of developing urinary incontinence than the norm
- those who more frequently consumed ready-made foods got 50% higher chance of developing urinary incontinence than the norm
- those who ate fruits daily enjoyed a 20% lower chance of urinary incontinence than the norm
So, in practical terms:
- practice mindful eating
- avoid ready-made foods
- enjoy fruit
You can read the paper in full here (it obviously goes into a lot more detail, and also covers other things beyond the scope of this article, such as fecal incontinence or, conversely, constipation—needless to say, the same advice stands in any case):
As for why this works the way it does: the study focused on the association and only hypothesized the question of “how”, but they did write a bit about that too, and it is almost certainly mostly a matter of gut health vs inflammation.
We really only have room for that kind of one-line summary here, but do read the paper if you’re interested, as it also talks about other dietary factors that had an impact, with the above-listed items being the topmost impactful factors, but for example (to take just one snippet of many possible ones):
❝In particular, saturated fatty acids (SFA) and cholesterol increased the risk for symptoms❞
~ Ibid. ← so do read it, for many more snippets like this!
What else does and doesn’t work
We covered a little while back the question of whether it is strengthening to hold one’s pee, or better to go whenever one feels the urge, and the answer is clear:
Meanwhile, supplements on the other hand are a mixed bag; there are some that probably help, and others, not so much:
What’s in the supplements that claim to help you cut down on bathroom breaks? And do they work?
Want to do more?
Check out these previous articles of ours:
Pelvic Floor Exercises (Not Kegels!) To Prevent Urinary Incontinence
and
Keeping Your Kidneys Happy: It’s About More Than Just Hydration! ← important at all ages, but especially relevant after 60
Take care!
Share This Post
Related Posts
-
Age & Aging: What Can (And Can’t) We Do About It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How old do you want to be?
We asked you how old you are, and got an interesting spread of answers. This wasn’t too surprising; of course we have a general idea of who our readership is and we write accordingly.
What’s interesting is the gap for “40s”.
And, this wasn’t the case of a broken poll button, it’s something that crops up a lot in health-related sociological research. People who are most interested in taking extra care of their body are often:
- Younger people full of optimism about maintaining this perfectly healthy body forever
- Older people realizing “if I don’t want to suffer avoidable parts of age-related decline, now is the time to address these things”
In between, we often have a gap whereby people no longer have the optimism of youth, but do not yet feel the pressure of older age.
Which is not to say there aren’t 40-somethings who do care! Indeed, we know for a fact we have some subscribers in their 40s (and some in their 90s, too), just, they evidently didn’t vote in this poll.
Anyway, let’s bust some myths…
Aging is inevitable: True or False?
False, probably. That seems like a bold (and fortune-telling) claim, so let’s flip it to deconstruct it more logically:
Aging is, and always will be, unstoppable: True or False?
That has to be “False, probably”. To say “true” now sounds like an even bolder claim. Just like “the moon will always be out of reach”.
- When CPR was first developed, first-aiders were arrested for “interfering with a corpse”.
- Many diseases used to be death sentences that are now “take one of these in the morning”
- If you think this is an appeal to distant history, HIV+ status was a death sentence in the 90s. Now it’s “take one of these in the morning”.
But, this is an appeal to the past, and that’s not always a guarantee of the future. Where does the science stand currently? How is the research and development doing on slowing, halting, reversing aging?
We can slow aging: True or False?
True! There’s a difference between chronological age (i.e., how much time has passed while we’ve been alive) and biological age (i.e., what our diverse markers of aging look like).
Biological age often gets talked about as a simplified number, but it’s more complex than that, as we can age in different ways at different rates, for example:
- Visual markers of aging (e.g. wrinkles, graying hair)
- Performative markers of aging (e.g. mobility tests)
- Internal functional markers of aging (e.g. tests for cognitive decline, eyesight, hearing, etc)
- Cellular markers or aging (e.g. telomere length)
- …and more, but we only have so much room here
There are things we can do to slow most of those, including:
- Good nutrition (e.g. collagen and lutein, to keep specific parts of the body functioning “like those of a younger person” ranging from the joints to the eyes and brain)
- Anti-oxidant activity (e.g. eating anti-oxidant foods, supplementing with anti-oxidants or other things that mitigate oxidative stress, and avoiding foods that hasten oxidative stress which causes many kinds of aging)
- Getting good sleep (not to be underestimated for its restorative importance)
- Taking care of our cognitive health
- Taking care of our mental health (especially: reducing stress)
- Taking care of our mobility (prevention is better than cure!)
In the case of cognitive decline particularly, check out our previous article:
How To Reduce Your Alzheimer’s Risk
It’s too early to worry about… / It’s too late to do anything about… True or False?
False and False!
Many things that affect our health later in life are based on early-life choices and events. So it’s important for young people to take advantage of that. The earlier one adopts a healthy lifestyle, the better, because, and hold onto your hats for the shocker here: aging is cumulative.
However, that doesn’t mean that taking up healthy practices (or dropping unhealthy ones) is pointless later in life, even in one’s 70s and beyond!
Read about this and more from the National Institute of Aging:
What Do We Know About Healthy Aging?
We can halt aging: True or False?
False, for now at least. Our bodies are not statues; they are living organisms, constantly rebuilding themselves, constantly changing, every second of every day, for better or for worse. Every healthy or unhealthy choice you make, every beneficial or adverse experience you encounter, affects your body on a cellular level.
Your body never, ever, stops changing for as long as you live.
But…
We can reverse aging: True or False?
True! Contingently and with limitations, for now at least.
Remember what we said about your body constantly rebuilding itself? That goes for making itself better as well as making itself worse.
- If yesterday you couldn’t touch your toes and today you can, congratulations, you just got younger by a biological marker of aging.
- If you stopped drinking/smoking/eating a certain way last year, and this year your skin has fewer wrinkles, congratulations, you got younger by a biological marker of aging.
- If you’ve been exercising and now your heart rate variability and VO2 max are better than last month, congratulations, you got younger by a biological marker aging.
- If you took supplements that reduce and/or mitigate oxidative stress (e.g. resveratrol, CoQ10, l-theanine, etc), and you took up intermittent fasting, and now your telomeres are longer than they were six months ago, congratulations, you got younger by a biological marker of aging.
But those aren’t really being younger, we’ll still die when our time is up: True or False?
False and True, respectively.
Those kinds of things are really being younger, biologically. What else do you think being biologically younger is?
We may indeed die when our time is up, but (unless we suffer fatal accident or incident first) “when our time is up” is something that is decided mostly by the above factors.
Genetics—the closest thing we have to biological “fate”—accounts for only about 25% of our longevity-related health*.
Genes predispose, but they don’t predetermine.
*Read more: Human longevity: Genetics or Lifestyle? It takes two to tango
(from the Journal of Immunity and Ageing)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Chia Seeds vs Sunflower Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chia seeds to sunflower, we picked the chia.
Why?
It was close, and they both have their merits!
In terms of macros, chia has more carbs and a lot more fiber, while sunflower has a little more protein and a lot more fat. While the fat (in the seeds, not processed seed oils!) is mostly healthy polyunsaturated fat in both cases, chia has a lot more omega-3. All in all, we’re calling it a win for chia on macros.
In the category of vitamins, chia has more of vitmains B3 and C, while sunflower has ore of vitamins B1, B2, B9, and E. Thus, a win for sunflower seeds this time.
When it comes to minerals, chia has more calcium, iron, magnesium, manganese, phosphorus, and selenium, while sunflower has more copper, potassium, and zinc. A 6:3 win for chia here.
Adding up the sections makes for an overall win for chia, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
The Tiniest Seeds With The Most Value: If You’re Not Taking Chia, You’re Missing Out!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Best Foods For Collagen Production
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Andrea Suarez gives us the low-down on collagen synthesis and maintenance. Collagen is the most abundant protein in our body, and it can be fairly described as “the stuff that holds us together”. It’s particularly important for joints and bones too, though many people’s focus on it is for the skin. Whatever your priorities, collagen levels are something it pays to be mindful of, as they usually drop quite sharply after a certain age. What certain age? Well, that depends a lot on you, and your diet and lifestyle. But it can start to decline from the age of 30 with often noticeable drop-offs in one’s mid-40s and again in one’s mid-60s.
Showing us what we’re made of
There’s a lot more to having good collagen levels than just how much collagen we consume (which for vegetarians/vegans, will be “none”, unless using the “except if for medical reasons” exemption, which is probably a little tenuous in the case of collagen but nevertheless it’s a possibility; this exemption is usually one that people use for, say, a nasal spray vaccine that contains gelatine, or a medicinal tablet that contains lactose, etc).
Rather, having good collagen levels is also a matter of what we eat that allows us to synthesize our own collagen (which includes: its ingredients, and various “helper” nutrients), as well as what dietary adjustments we make to avoid our extant collagen getting broken down, degraded, and generally lost.
Here’s what Dr. Suarez recommends:
Protein-rich foods (but watch out)
- Protein is essential for collagen production.
- Sources: fish, soy, lean meats (but not red meats, which—counterintuitively—degrade collagen), eggs, lentils.
- Egg whites are high in lysine, vital for collagen synthesis.
- Bone broth is a natural source of collagen.
Omega-3 fatty acids
- Omega-3s are anti-inflammatory and protect skin collagen.
- Sources: walnuts, chia seeds, flax seeds, fatty fish (e.g. mackerel, sardines).
Leafy greens
- Leafy dark green vegetables (e.g. kale, spinach) are rich in vitamins C and B9.
- Vitamin C is crucial for collagen synthesis and acts as an antioxidant.
- Vitamin B9 supports skin cell division and DNA repair.
Red fruits & vegetables
- Red fruits/vegetables (e.g. tomatoes, red bell peppers) contain lycopene, an antioxidant that protects collagen from UV damage (so, that aspect is mostly relevant for skin, but antioxidants are good things to have in all of the body in any case).
Orange-colored vegetables
- Carrots and sweet potatoes are rich in vitamin A, which helps in collagen repair and synthesis.
- Vitamin A is best from food, not supplements, to avoid potential toxicity.
Fruits rich in vitamin C
- Citrus fruits, kiwi, and berries are loaded with vitamin C and antioxidants, essential for collagen synthesis and skin health.
Soy
- Soy products (e.g. tofu, soybeans) contain isoflavones, which reduce inflammation and inhibit enzymes that degrade collagen.
- Soy is associated with lower risks of chronic diseases.
Garlic
- Garlic contains sulfur, taurine, and lipoic acid, important for collagen production and repair.
What to avoid:
- Reduce foods high in advanced glycation end products (AGEs), which damage collagen and promote inflammation.
- AGEs are found in fried, roasted, or grilled fatty proteinous foods (e.g. meat, including synthetic meat, and yes, including grass-fed nicely marketed meat—although processed meat such as bacon and sausages are even worse than steaks etc).
- Switch to cooking methods like boiling or steaming to reduce AGE levels.
- Processed foods, sugary pastries, and red meats contribute to collagen degradation.
General diet tips:
- Incorporate more plant-based, antioxidant-rich foods.
- Opt for slow cooking to reduce AGEs.
- Since sustainability is key, choose foods you enjoy for a collagen-boosting diet that you won’t seem like a chore a month later.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
We Are Such Stuff As Fish Are Made Of ← our main feature research review about collagen
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: