How To Improve Your Heart Rate Variability
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How’s your heart rate variability?
The hallmarks of a good, strong cardiovascular system include a medium-to-low resting heart rate (for adults: under 60 beats per minute is good; under 50 is typical of athletes), and healthy blood pressure (for adults: under 120/80, while still above 90/60, is generally considered good).
Less talked-about is heart rate variability, but it’s important too…
What is heart rate variability?
Heart rate variability is a measure of how quickly and easily your heart responds to changes in demands placed upon it. For example:
- If you’re at rest and then start running your fastest (be it for leisure or survival or anything in between), your heart rate should be able to jump from its resting rate to about 180% of that as quickly as possible
- When you stop, your heart rate should be able to shift gears back to your resting rate as quickly as possible
The same goes, to a commensurately lesser extent, to changes in activity between low and moderate, or between moderate and high.
- When your heart can change gears quickly, that’s called a high heart rate variability
- When your heart is sluggish to get going and then takes a while to return to normal after exertion, that’s called a low heart rate variability.
The rate of change (i.e., the variability) is measured in microseconds per beat, and the actual numbers will vary depending on a lot of factors, but for everyone, higher is better than lower.
Aside from quick response to crises, why does it matter?
If heart rate variability is low, it means the sympathetic nervous system is dominating the parasympathetic nervous system, which means, in lay terms, your fight-or-flight response is overriding your ability to relax.
See for example: Stress and Heart Rate Variability: A Meta-Analysis and Review of the Literature
This has a lot of knock-on effects for both physical and mental health! Your heart and brain will take the worst of this damage, so it’s good to improve things for them impossible.
This Saturday’s Life Hacks: how to improve your HRV!
Firstly, the Usual Five Things™:
- A good diet (that avoids processed foods)
- Good exercise (that includes daily physical activity—more often is more important than more intense!)
- Good sleep (7–9 hours of good quality sleep per night)
- Reduce or eliminate alcohol consumption (this is dose-dependent; any reduction is an improvement)
- Don’t smoke (just don’t)
Additional regular habits that help a lot:
- Breathing exercises, mindfulness, meditation
- Therapy, especially CBT and DBT
- Stress-avoidance strategies, for example:
- Get (and maintain) your finances in good order
- Get (and maintain) your relationship(s) in good order
- Get (and maintain) your working* life in good order
*Whatever this means to you. If you’re perhaps retired, or otherwise a home-maker, or even a student, the things you “need to do” on a daily basis are your working life, for these purposes.
In terms of simple, quick-fix, physical tweaks to focus on if you’re already broadly leading a good life, two great ones are:
- Exercise: get moving! Walk to the store even if you buy nothing but a snack or drink to enjoy while walking back. If you drove, make more trips with the shopping bags rather than fewer. If you like to watch TV, consider an exercise bike or treadmill to use while watching. If you have a partner, double-up and make it a thing you do together! Take the stairs instead of the elevator. Take the scenic route when walking someplace. Go to the bathroom that’s further away. Every little helps!
- Breathe: even just a couple of times a day, practice mindful breathing. Start with even just a minute a day, to get the habit going. What breathing exercise you do isn’t so important as that you do it. Notice your breathing; count how long each breath takes. Don’t worry about “doing it right”—you’re doing great, just observe, just notice, just slowly count. We promise that regular practice of this will have you feeling amazing
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Nicotine Benefits (That We Don’t Recommend)!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Does nicotine have any benefits at all? I know it’s incredibly addictive but if you exclude the addiction, does it do anything?❞
Good news: yes, nicotine is a stimulant and can be considered a performance enhancer, for example:
❝Compared with the placebo group, the nicotine group exhibited enhanced motor reaction times, grooved pegboard test (GPT) results on cognitive function, and baseball-hitting performance, and small effect sizes were noted (d = 0.47, 0.46 and 0.41, respectively).❞
Read in full: Acute Effects of Nicotine on Physiological Responses and Sport Performance in Healthy Baseball Players
However, another study found that its use as a cognitive enhancer was only of benefit when there was already a cognitive impairment:
❝Studies of the effects of nicotinic systems and/or nicotinic receptor stimulation in pathological disease states such as Alzheimer’s disease, Parkinson’s disease, attention deficit/hyperactivity disorder and schizophrenia show the potential for therapeutic utility of nicotinic drugs.
In contrast to studies in pathological states, studies of nicotine in normal-non-smokers tend to show deleterious effects.
This contradiction can be resolved by consideration of cognitive and biological baseline dependency differences between study populations in terms of the relationship of optimal cognitive performance to nicotinic receptor activity.
Although normal individuals are unlikely to show cognitive benefits after nicotinic stimulation except under extreme task conditions, individuals with a variety of disease states can benefit from nicotinic drugs❞
Read in full: Effects of nicotinic stimulation on cognitive performance
Bad news: its addictive qualities wipe out those benefits due to tolerance and thus normalization in short order. So you may get those benefits briefly, but then you’re addicted and also lose the benefits, as well as also ruining your health—making it a lose/lose/lose situation quite quickly.
As an aside, while nicotine is poisonous per se, in the quantities taken by most users, the nicotine itself is not usually what kills. It’s mostly the other stuff that comes with it (smoking is by far and away the worst of all; vaping is relatively less bad, but that’s not a strong statement in this case) that causes problems.
See also: Vaping: A Lot Of Hot Air?
However, this is still not an argument for, say, getting nicotine gum and thinking “no harmful effects” because then you’ll be get a brief performance boost yes before it runs out and being addicted to it and now being in a position whereby if you stop, your performance will be lower than before you started (since you now got used to it, and it became your new normal), before eventually recovering:
In summary
We recommend against using nicotine in the first place, and for those who are addicted, we recommend quitting immediately if not contraindicated (check with your doctor if unsure; there are some situations where it is inadvisable to take away something your body is dependent on, until you correct some other thing first).
For more on quitting in general, see:
Addiction Myths That Are Hard To Quit
Take care!
Share This Post
-
Margarine vs Butter – Which is Healthier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing margarine to butter, we picked the butter.
Why?
Once upon a time, when margarines were filled with now-banned trans fats, this would have been an easy win for butter.
Nowadays, the macronutrient/lipid profiles are generally more similar (although margarine often has a little less saturated fat), except one thing that butter has in its favor:
More micronutrients. What exactly they are (and how much) depends on the diet and general health of the cows from whom the milk to make the butter came, but they’re not something found in plant-based butter alternatives at this time.
Nevertheless, because of the saturated fat content, it’s not advisable to use more than a very small amount of either (two tablespoons of butter would put one at the daily limit already, without eating any other saturated fat that day).
Read more: Butter vs Margarine
Share This Post
-
Adult Children of Emotionally Immature Parents – by Dr. Lindsay Gibson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
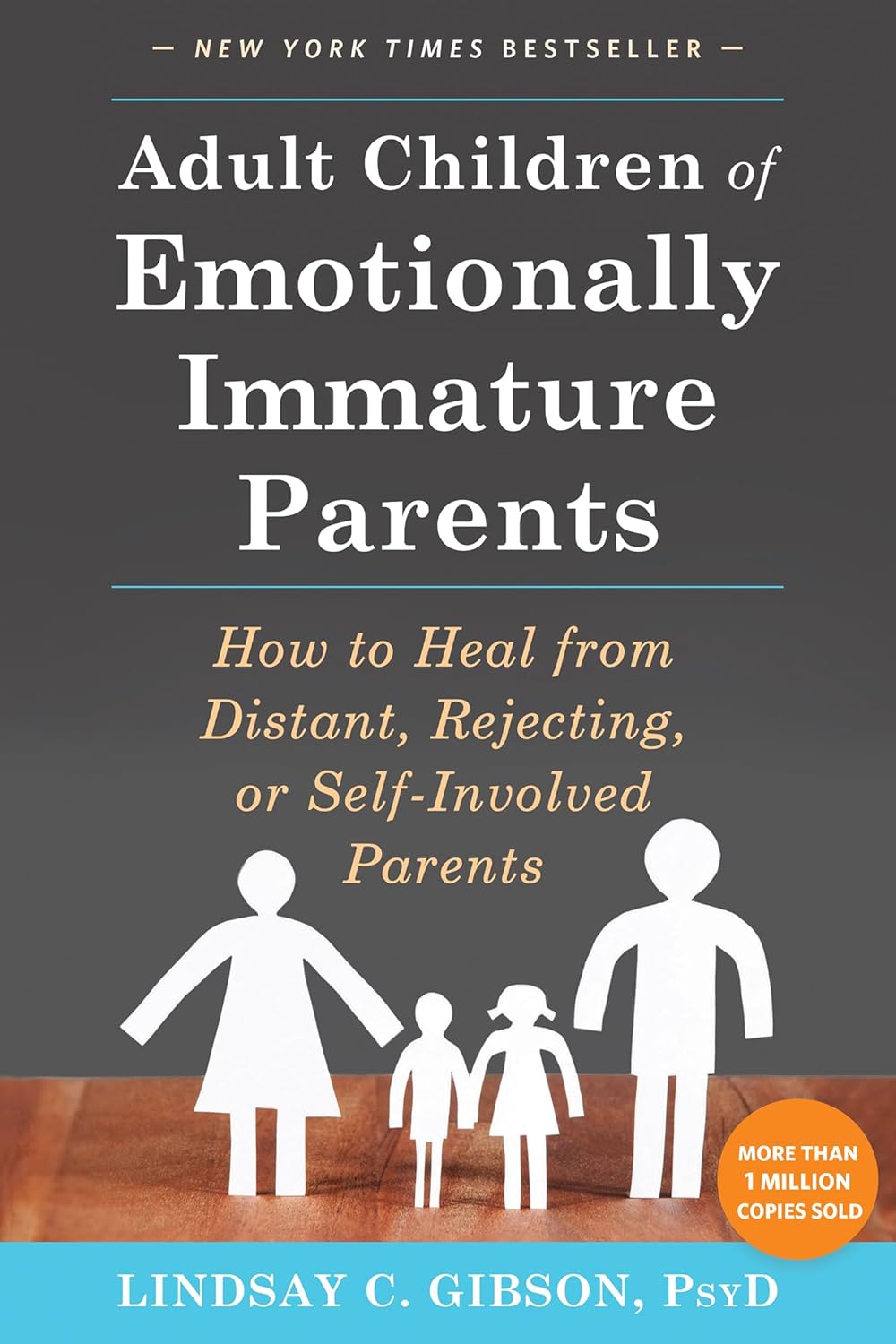
Not everyone had the best of parents, and the harm done can last well beyond childhood. This book looks at healing that.
Dr. Gibson talks about four main kinds of “difficult” parents, though of course they can overlap:
- The emotional parent, with their unpredictable outbursts
- The driven parent, with their projected perfectionism
- The passive parent, with their disinterest and unreliability
- The rejecting parent, with their unavailability and insults
For all of them, it’s common that nothing we could do was ever good enough, and that leaves a deep scar. To add to it, the unfavorable dynamic often persists in adult life, assuming everyone involved is still alive and in contact.
So, what to do about it? Dr. Gibson advocates for first getting a good understanding of what wasn’t right/normal/healthy, because it’s easy for a lot of us to normalize the only thing we’ve ever known. Then, beyond merely noting that no child deserved that lack of compassion, moving on to pick up the broken pieces one by one, and address each in turn.
The style of the book is anecdote-heavy (case studies, either anonymized or synthesized per common patterns) in a way that will probably be all-too-relatable to a lot of readers (assuming that if you buy this book, it’s for a reason), science-moderate (references peppered into the text; three pages of bibliography), and practicality-dense—that is to say, there are lots of clear usable examples, there are self-assessment questionnaires, there are worksheets for now making progress forward, and so forth.
Bottom line: if one or more of the parent types above strikes a chord with you, there’s a good chance you could benefit from this book.
Click here to check out Adult Children of Emotionally Immature Parents, and rebuild yourself!
Share This Post
Related Posts
-
Feeding your baby butter won’t help them sleep through the night, whatever TikTok says
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sleep is the holy grail for new parents. So no wonder many tired parents are looking for something to help their babies sleep.
A TikTok trend claims giving your baby a tablespoon or two of butter in the evening will help them sleep more at night.
As we’ll see, butter is just the latest food that promises to help babies sleep at night. But no single food can do this.
So if you’re a new parent and desperate for a good night’s sleep, here’s what to try instead.
BaLL LunLa/Shutterstock Is my baby’s sleep normal?
Babies need help to fall asleep, through feeding, movement (like rocking) or touch (like a cuddle or massage).
Newborn babies also do not know night from day. Melatonin in breastmilk helps babies sleep more at night until they start to make this sleep-inducing hormone themselves. Bottlefed newborn babies do not have access to this melatonin. Regardless of how you feed your baby, it can take several months for them to develop a sleep pattern with longer stretches at night.
Babies also sleep lighter than older children and adults. Light sleep helps ensure they continue breathing, protecting them from SIDS (sudden infant death syndrome). It also means they wake easily and often.
The idea that babies should sleep deeply, alone and for long stretches, goes against their physiology. So “sleeping like a baby” usually means waking quite a lot at night.
Yet, many parents have been asked whether their baby is sleeping through the night and is a “good baby”. The perception is that if a baby doesn’t sleep for long stretches at night, it must be “bad”.
This may lead parents to say their babies sleep longer than they really do, setting unrealistic expectations for other new parents.
Could feeding butter do any harm?
The social pressure around baby sleep can add stress and anxiety for new parents. So the Tiktok trend about feeding babies butter may seem tempting.
But giving babies any solid food before they are around six months old is not recommended. Babies’ digestive systems are not ready for solid food until they are around six months and feeding them before this can cause constipation or make them more likely to catch an illness. For this reason alone, you should not give your young baby butter.
From about six months old, babies should be offered nutritious, iron-rich solid foods. Butter doesn’t fit this bill because it is almost all saturated fat. If butter replaces more nutritious foods, babies may not get the vitamins and minerals they need.
Butter is just the latest food claimed to help babies sleep better at night. Pixel-Shot/Shutterstock Butter is the latest in a long line of beliefs about certain foods making babies sleep longer at night. It was once thought that adding cereal or crushed arrowroot biscuits in bottle of milk before bedtime would make them sleep longer. Research found this did not increase sleep at all.
Similarly, there is no evidence that giving babies butter before bed makes them sleep longer.
In fact, research shows the foods babies eat make no difference to night waking.
What else can I try?
Waking overnight doesn’t necessarily mean a baby is hungry. And stopping breastfeeds or bottle feeds overnight doesn’t necessarily reduce night waking.
Your baby could be too hot or cold, or need a nappy change. But some babies continue to wake at night even without an obvious problem.
The good news is, sleeping is a skill babies develop naturally as they grow.
Behavioural sleep interventions, known as “sleep training”, are not very effective in increasing overnight sleep. In one study, sleep training did not reduce the number of night wakes and only increased the length of the longest sleep by about 16 minutes. Sleep training is especially not recommended for babies under six months.
The good news is that babies do eventually get the hang of sleeping at night. Miljan Zivkovic/Shutterstock Look after yourself
If you’re missing out on sleep at night, try to have small naps during the day while your baby sleeps. Ask friends and family to do some chores to allow you to nap.
If your baby is crying and you find yourself getting overwhelmed it is OK to put your baby down somewhere safe (like a cot or baby mat) and take some time to settle yourself.
If your baby’s sleep pattern changes significantly or they haven’t slept at all for more than a day, or if your baby seems to have pain or a fever see your doctor, or family and child health nurse, as soon as possible.
Some helpful resources
If you think your baby is not sleeping well because of a breastfeeding problem, the Australian Breastfeeding Association has a national helpline. The association can also advise on co-sleeping.
The charity Little Sparklers provides peer support for parents, including someone to chat to, about baby sleep. It also has helpful resources.
UNICEF has resources about caring for your baby at night. And the UK-based Baby Sleep Info Source (Basis) provides evidence-based information about babies and sleep.
Karleen Gribble, Adjunct Professor, School of Nursing and Midwifery, Western Sydney University; Naomi Hull, PhD candidate, Sydney School of Public Health, University of Sydney, and Nina Jane Chad, Research Fellow, University of Sydney School of Public Health, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Okra vs Asparagus – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing okra to asparagus, we picked the okra.
Why?
Both are great! But…
In terms of macros, okra has more fiber and carbs, making it the more nutrient dense option, for a similar glycemic index.
In the category of vitamins, okra has more of vitamins B1, B3, B6, B9, and C, while asparagus has more of vitamins B2, B5, E, K, and choline, making for a 5:5 tie, with similar margins of difference too. Thus, definitely a tie on vitamins.
When it comes to minerals, okra has more calcium, magnesium, manganese, phosphorus, potassium, and zinc, while asparagus has more copper, iron, and selenium. An easy 6:3 win for okra.
Both of these on-the-cusp-of-being-pungent vegetables have beneficial antioxidant polyphenols (especially various forms of quercetin), but okra has more.
Adding up the sections makes for an overall win for okra, but by all means enjoy either both; diversity is good!
Want to learn more?
You might like to read:
Enjoy Bitter/Astringent/Pungent Foods For Your Heart & Brain
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A new emergency procedure for cardiac arrests aims to save more lives – here’s how it works
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As of January this year, Aotearoa New Zealand became just the second country (after Canada) to adopt a groundbreaking new procedure for patients experiencing cardiac arrest.
Known as “double sequential external defibrillation” (DSED), it will change initial emergency response strategies and potentially improve survival rates for some patients.
Surviving cardiac arrest hinges crucially on effective resuscitation. When the heart is working normally, electrical pulses travel through its muscular walls creating regular, co-ordinated contractions.
But if normal electrical rhythms are disrupted, heartbeats can become unco-ordinated and ineffective, or cease entirely, leading to cardiac arrest.
Defibrillation is a cornerstone resuscitation method. It gives the heart a powerful electric shock to terminate the abnormal electrical activity. This allows the heart to re-establish its regular rhythm.
Its success hinges on the underlying dysfunctional heart rhythm and the proper positioning of the defibrillation pads that deliver the shock. The new procedure will provide a second option when standard positioning is not effective.
Using two defibrillators
During standard defibrillation, one pad is placed on the right side of the chest just below the collarbone. A second pad is placed below the left armpit. Shocks are given every two minutes.
Early defibrillation can dramatically improve the likelihood of surviving a cardiac arrest. However, around 20% of patients whose cardiac arrest is caused by “ventricular fibrillation” or “pulseless ventricular tachycardia” do not respond to the standard defibrillation approach. Both conditions are characterised by abnormal activity in the heart ventricles.
DSED is a novel method that provides rapid sequential shocks to the heart using two defibrillators. The pads are attached in two different locations: one on the front and side of the chest, the other on the front and back.
A single operator activates the defibrillators in sequence, with one hand moving from the first to the second. According to a recent randomised trial in Canada, this approach could more than double the chances of survival for patients with ventricular fibrillation or pulseless ventricular tachycardia who are not responding to standard shocks.
The second shock is thought to improve the chances of eliminating persistent abnormal electrical activity. It delivers more total energy to the heart, travelling along a different pathway closer to the heart’s left ventricle.
Evidence of success
New Zealand ambulance data from 2020 to 2023 identified about 1,390 people who could potentially benefit from novel defibrillation methods. This group has a current survival rate of only 14%.
Recognising the potential for DSED to dramatically improve survival for these patients, the National Ambulance Sector Clinical Working Group updated the clinical procedures and guidelines for emergency medical services personnel.
The guidelines now specify that if ventricular fibrillation or pulseless ventricular tachycardia persist after two shocks with standard defibrillation, the DSED method should be administered. Two defibrillators need to be available, and staff must be trained in the new approach.
Though the existing evidence for DSED is compelling, until recently it was based on theory and a small number of potentially biased observational studies. The Canadian trial was the first to directly compare DSED to standard treatment.
From a total of 261 patients, 30.4% treated with this strategy survived, compared to 13.3% when standard resuscitation protocols were followed.
The design of the trial minimised the risk of other factors confounding results. It provides confidence that survival improvements were due to the defibrillation approach and not regional differences in resources and training.
The study also corroborates and builds on existing theoretical and clinical scientific evidence. As the trial was stopped early due to the COVID-19 pandemic, however, the researchers could recruit fewer than half of the numbers planned for the study.
Despite these and other limitations, the international group of experts that advises on best practice for resuscitation updated its recommendations in 2023 in response to the trial results. It suggested (with caution) that emergency medical services consider DSED for patients with ventricular fibrillation or pulseless ventricular tachycardia who are not responding to standard treatment.
Training and implementation
Although the evidence is still emerging, implementation of DSED by emergency services in New Zealand has implications beyond the care of patients nationally. It is also a key step in advancing knowledge about optimal resuscitation strategies globally.
There are always concerns when translating an intervention from a controlled research environment to the relative disorder of the real world. But the balance of evidence was carefully considered before making the decision to change procedures for a group of patients who have a low likelihood of survival with current treatment.
Before using DSED, emergency medical personnel undergo mandatory education, simulation and training. Implementation is closely monitored to determine its impact.
Hospitals and emergency departments have been informed of the protocol changes and been given opportunities to ask questions and give feedback. As part of the implementation, the St John ambulance service will perform case reviews in addition to wider monitoring to ensure patient safety is prioritised.
Ultimately, those involved are optimistic this change to cardiac arrest management in New Zealand will have a positive impact on survival for affected patients.
Vinuli Withanarachchie, PhD candidate, College of Health, Massey University; Bridget Dicker, Associate Professor of Paramedicine, Auckland University of Technology, and Sarah Maessen, Research Associate, Auckland University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: