Lifespan vs Healthspan, And The Spice Of Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Great newsletter. Am taking turmeric for inflammation of hips and feet. Works like magic. Would like to know how it works, and what tumeric is best combined with – also whether there any risks in longterm use.❞
Glad you’re enjoying! As for turmeric, it sure is great, isn’t it? To answer your questions in a brief fashion:
- How it works: it does a lot of things, but perhaps its most key feature is its autoxidative metabolites that mediate its anti-inflammatory effect. This, it slows or inhibits oxidative stress that would otherwise cause inflammation, increase cancer risk, and advance aging.
- Best combined with: black pepper
- Any risks in long-term use: there are no known risks in long-term use ← that’s just one study, but there are lots. Some studies were prompted by reported hepatotoxicity of curcumin supplements, but a) the reports themselves seem to be without evidence b) the reported hepatoxicity was in relation to contaminants in the supplements, not the curcumin itself c) clinical trials were unable to find any hepatotoxicity (or other) risks anyway. Here’s an example of such a study.
You might also like our previous main feature: Why Curcumin (Turmeric) Is Worth Its Weight In Gold
❝This push for longevity is appealing but watching my mother in her nineties is a life I’m not looking forward to. Healthy longevity, yes, but longevity for the sake of a longer life? No thank you.❞
Yes, you’re quite right, that’s exactly the point! Assuming we live to die of age-related conditions (i.e., we do not suffer a fatal accident or incident in our younger years), those unfun last years are coming whether they come at 75 or 95. Or earlier or later, because that can absolutely happen too!
For example: nearly 10% of Americans over 65 have difficulty with self-care
As a rule, and we’ve covered some of the science of this previously, having at least 4 out of 5 of the “big 5” lifestyle factors (diet, exercise, sleep, low-or-zero alcohol, not smoking) not only extends life, but specifically extends the healthspan, i.e. the count of healthy life-years that precedes final age-related decline.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Voluntary assisted dying is different to suicide. But federal laws conflate them and restrict access to telehealth
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Voluntary assisted dying is now lawful in every Australian state and will soon begin in the Australian Capital Territory.
However, it’s illegal to discuss it via telehealth. That means people who live in rural and remote areas, or those who can’t physically go to see a doctor, may not be able to access the scheme.
A federal private members bill, introduced to parliament last week, aims to change this. So what’s proposed and why is it needed?
What’s wrong with the current laws?
Voluntary assisted dying doesn’t meet the definition of suicide under state laws.
But the Commonwealth Criminal Code prohibits the discussion or dissemination of suicide-related material electronically.
This opens doctors to the risk of criminal prosecution if they discuss voluntary assisted dying via telehealth.
Successive Commonwealth attorneys-general have failed to address the conflict between federal and state laws, despite persistent calls from state attorneys-general for necessary clarity.
This eventually led to voluntary assistant dying doctor Nicholas Carr calling on the Federal Court of Australia to resolve this conflict. Carr sought a declaration to exclude voluntary assisted dying from the definition of suicide under the Criminal Code.
In November, the court declared voluntary assisted dying was considered suicide for the purpose of the Criminal Code. This meant doctors across Australia were prohibited from using telehealth services for voluntary assisted dying consultations.
Last week, independent federal MP Kate Chaney introduced a private members bill to create an exemption for voluntary assisted dying by excluding it as suicide for the purpose of the Criminal Code. Here’s why it’s needed.
Not all patients can physically see a doctor
Defining voluntary assisted dying as suicide in the Criminal Code disproportionately impacts people living in regional and remote areas. People in the country rely on the use of “carriage services”, such as phone and video consultations, to avoid travelling long distances to consult their doctor.
Other people with terminal illnesses, whether in regional or urban areas, may be suffering intolerably and unable to physically attend appointments with doctors.
The prohibition against telehealth goes against the principles of voluntary assisted dying, which are to minimise suffering, maximise quality of life and promote autonomy.
Some people aren’t able to attend doctors’ appointments in person.
Jeffrey M Levine/ShutterstockDoctors don’t want to be involved in ‘suicide’
Equating voluntary assisted dying with suicide has a direct impact on doctors, who fear criminal prosecution due to the prohibition against using telehealth.
Some doctors may decide not to help patients who choose voluntary assisted dying, leaving patients in a state of limbo.
The number of doctors actively participating in voluntary assisted dying is already low. The majority of doctors are located in metropolitan areas or major regional centres, leaving some locations with very few doctors participating in voluntary assisted dying.
It misclassifies deaths
In state law, people dying under voluntary assisted dying have the cause of their death registered as “the disease, illness or medical condition that was the grounds for a person to access voluntary assisted dying”, while the manner of dying is recorded as voluntary assisted dying.
In contrast, only coroners in each state and territory can make a finding of suicide as a cause of death.
In 2017, voluntary assisted dying was defined in the Coroners Act 2008 (Vic) as not a reportable death, and thus not suicide.
The language of suicide is inappropriate for explaining how people make a decision to die with dignity under the lawful practice of voluntary assisted dying.
There is ongoing taboo and stigma attached to suicide. People who opt for and are lawfully eligible to access voluntary assisted dying should not be tainted with the taboo that currently surrounds suicide.
So what is the solution?
The only way to remedy this problem is for the federal government to create an exemption in the Criminal Code to allow telehealth appointments to discuss voluntary assisted dying.
Chaney’s private member’s bill is yet to be debated in federal parliament.
If it’s unsuccessful, the Commonwealth attorney-general should pass regulations to exempt voluntary assisted dying as suicide.
A cooperative approach to resolve this conflict of laws is necessary to ensure doctors don’t risk prosecution for assisting eligible people to access voluntary assisted dying, regional and remote patients have access to voluntary assisted dying, families don’t suffer consequences for the erroneous classification of voluntary assisted dying as suicide, and people accessing voluntary assisted dying are not shrouded with the taboo of suicide when accessing a lawful practice to die with dignity.
Failure to change this will cause unnecessary suffering for patients and doctors alike.
Michaela Estelle Okninski, Lecturer of Law, University of Adelaide; Marc Trabsky, Associate professor, La Trobe University, and Neera Bhatia, Associate Professor in Law, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Hormones & Health, Beyond The Obvious
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Wholesome Health
This is Dr. Sara Gottfried, who some decades ago got her MD from Harvard and specialized as an OB/GYN at MIT. She’s since then spent the more recent part of her career educating people (mostly: women) about hormonal health, precision, functional, & integrative medicine, and the importance of lifestyle medicine in general.
What does she want us to know?
Beyond “bikini zone health”
Dr. Gottfried urges us to pay attention to our whole health, in context.
“Women’s health” is often thought of as what lies beneath a bikini, and if it’s not in those places, then we can basically treat a woman like a man.
And that’s often not actually true—because hormones affect every living cell in our body, and as a result, while prepubescent girls and postmenopausal women (specifically, those who are not on HRT) may share a few more similarities with boys and men of similar respective ages, for most people at most ages, men and women are by default quite different metabolically—which is what counts for a lot of diseases! And note, that difference is not just “faster” or “slower””, but is often very different in manner also.
That’s why, even in cases where incidence of disease is approximately similar in men and women when other factors are controlled for (age, lifestyle, medical history, etc), the disease course and response to treatment may vary considerable. For a strong example of this, see for example:
- The well-known: Heart Attack: His & Hers ← most people know these differences exist, but it’s always good to brush up on what they actually are
- The less-known: Statins: His & Hers ← most people don’t know these differences exist, and it pays to know, especially if you are a woman or care about one
Nor are brains exempt from his…
The female brain (kinda)
While the notion of an anatomically different brain for men and women has long since been thrown out as unscientific phrenology, and the idea of a genetically different brain is… Well, it’s an unreliable indicator, because technically the cells will have DNA and that DNA will usually (but not always; there are other options) have XX or XY chromosomes, which will usually (but again, not always) match apparent sex (in about 1/2000 cases there’s a mismatch, which is more common than, say, red hair; sometimes people find out about a chromosomal mismatch only later in life when getting a DNA test for some unrelated reason), and in any case, even for most of us, the chromosomal differences don’t count for much outside of antenatal development (telling the default genital materials which genitals to develop into, though this too can get diverted, per many intersex possibilities, which is also a lot more common than people think) or chromosome-specific conditions like colorblindness…
The notion of a hormonally different brain is, in contrast to all of the above, a reliable and easily verifiable thing.
See for example:
Alzheimer’s Sex Differences May Not Be What They Appear
Dr. Gottfried urges us to take the above seriously!
Because, if women get Alzheimer’s much more commonly than men, and the disease progresses much more quickly in women than men, but that’s based on postmenopausal women not on HRT, then that’s saying “Women, without women’s usual hormones, don’t do so well as men with men’s usual hormones”.
She does, by the way, advocate for bioidentical HRT for menopausal women, unless contraindicated for some important reason that your doctor/endocrinologist knows about. See also:
Menopausal HRT: A Tale Of Two Approaches (Bioidentical vs Animal)
The other very relevant hormone
…that Dr. Gottfried wants us to pay attention to is insulin.
Or rather, its scrubbing enzyme, the prosaically-named “insulin-degrading enzyme”, but it doesn’t only scrub insulin. It also scrubs amyloid beta—yes, the same that produces the amyloid beta plaques in the brain associated with Alzheimer’s. And, there’s only so much insulin-degrading enzyme to go around, and if it’s all busy breaking down excess insulin, there’s not enough left to do the other job too, and thus can’t break down amyloid beta.
In other words: to fight neurodegeneration, keep your blood sugars healthy.
This may actually work by multiple mechanisms besides the amyloid hypothesis, by the way:
The Surprising Link Between Type 2 Diabetes & Alzheimer’s
Want more from Dr. Gottfried?
You might like this interview with Dr. Gottfried by Dr. Benson at the IMCJ:
Integrative Medicine: A Clinician’s Journal | Conversations with Sara Gottfried, MD
…in which she discusses some of the things we talked about today, and also about her shift from a pharmaceutical-heavy approach to a predominantly lifestyle medicine approach.
Enjoy!
Share This Post
-
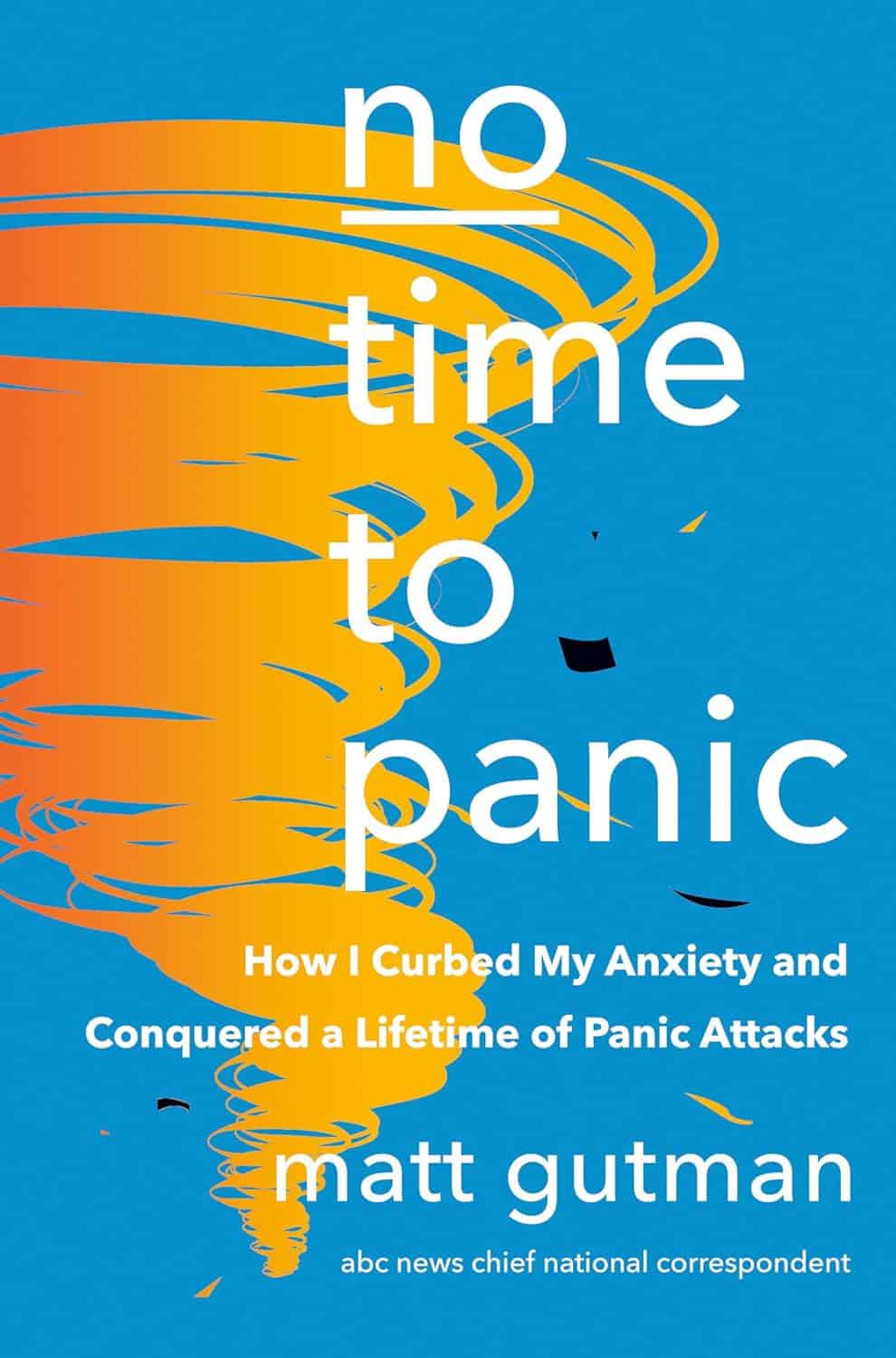
No Time to Panic – by Matt Gutman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Matt Gutman is not a doctor or a psychologist. He’s a journalist, accustomed to asking questions and then asking more probing questions, unrelenting until he gets the answers he’s looking for.
This book is the result of what happened when he needed to overcome his own anxiety and panic attacks, and went on an incisive investigative journey.
The style is as clear and accessible as you’d expect of a journalist, and presents a very human exploration, nonetheless organized in a way that will be useful to the reader.
It’s said that “experience is a great teacher, but she sends hefty bills”. In this case as in many, it’s good to learn from someone else’s experience!
By the end of the book, you’ll have a good grounding in most approaches to dealing with anxiety and panic attacks, and an idea of efficacy/applicability, and what to expect.
Bottom line: without claiming any magic bullet, this book presents six key strategies that Gutman found to work, along with his experiences of what didn’t. Valuable reading if you want to curb your own anxiety, or want to be able to help/support someone else with theirs.
Click here to check out No Time To Panic, and find the peace you deserve!
Share This Post
Related Posts
-
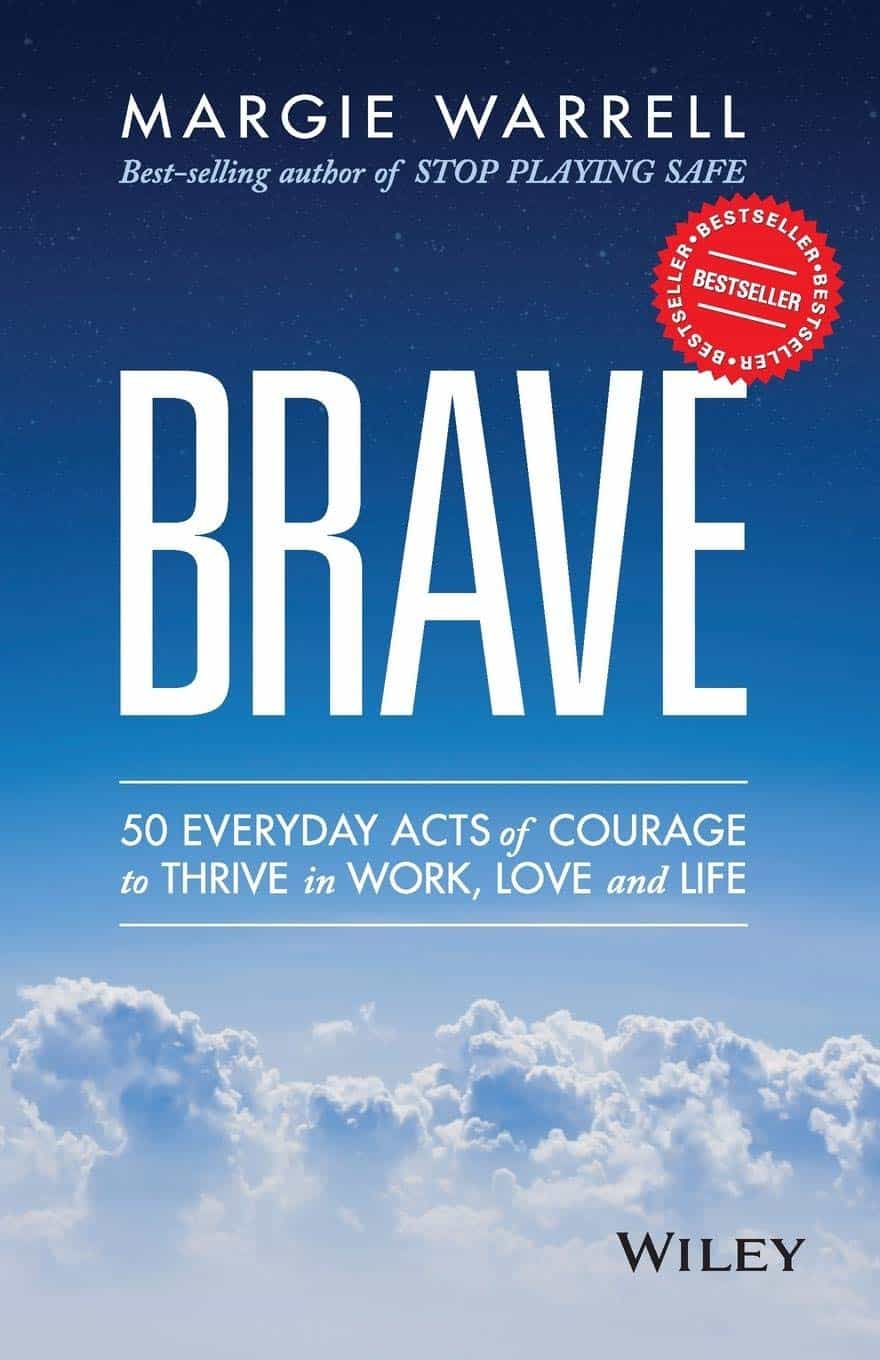
Brave – by Dr. Margie Warrell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whether it’s the courage to jump out of a plane or the courage to have a difficult conversation, bravery is an important quality that we often don’t go far out of our way to grow. At least, not as adults.
Rather than viewing bravery as a static attribute—you either have it or you don’t—psychologist Dr. Margie Warrell makes the case for its potential for lifelong development.
The book is divided into five sections:
- Live purposefully
- Speak bravely
- Work passionately
- Dig deep
- Dare boldly
…and each has approximately 10 chapters, each a few pages long, the kind that can easily make this a “chapter-a-day” daily reader.
As a quick clarification: that “speak bravely” section isn’t about public speaking, but is rather about speaking up when it counts. Life is too short for regrets, and our interactions with others tend to be what matters most in the long-run. It makes a huge difference to our life!
Dr. Warrell gives us tools to reframe our challenges and tackle them. Rather than just saying “Feel the fear and do it anyway”, she also delivers the how, in all aspects. This is one of the main values the book brings, as well as a sometimes-needed reminder of how and why being brave is something to which we should always aspire… and hold.
Bottom line: if you’d like to be more brave—in any context—this book can help. We only get one life; might as well live it.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
5 Self-Care Trends That Are Actually Ruining Your Mental Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ok, some of these are trends; some are more perennial to human nature. For example, while asceticism is not a new idea, the “dopamine detox” is, and “bed rotting” is not a trend that this writer has seen recommended anywhere, but on the other hand, there are medieval illustrations of it—there was no Netflix in sight in the medieval illustrations, but perhaps a label diagnosing it as “melancholy”, for example.
So without further ado, here are five things to not do…
Don’t fall into these traps
The 5 things to watch out for are:
- Toxic positivity: constantly promoting positivity regardless of the reality of a situation can shame or invalidate genuine emotions, preventing people from processing their real feelings and leading to negative mental health outcomes—especially if it involves a “head in sand” approach to external problems as well as internal ones (because then those problems will never actually get dealt with).
- Self-indulgence: excessive focus on personal desires can make you more self-centered, less disciplined, and ultimately dissatisfied, which hinders personal growth and mental wellness.
- Bed rotting: spending prolonged time in bed for relaxation or entertainment can decrease motivation, productivity, and lead to (or worsen) depression rather than promoting genuine rest and rejuvenation.
- Dopamine detox: abstaining from pleasurable activities to “reset” the brain simply does not work and can lead to loneliness, boredom, and worsen mental health, especially when done excessively.
- Over-reliance on self-help: consuming too much self-help content or relying on material possessions for well-being can lead to information overload, unrealistic expectations, and the constant need for self-fixing, rather than fostering self-acceptance and authentic growth. Useful self-help can be like taking your car in for maintenance—counterproductive self-help is more like having your car always in for maintenance and never actually on the road.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read, and yes these are pretty much one-for-one with the 5 items above, doing a deeper dive into each in turn,
- How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
- Self-Care That’s Not Just Self-Indulgence
- The Mental Health First-Aid That You’ll Hopefully Never Need
- The Dopamine Myth
- Behavioral Activation Against Depression & Anxiety
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
L-Theanine: What’s The Tea?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
L-Theanine: What’s The Tea?
We’ve touched previously on l-theanine, when this newsletter was new, and we had only a few hundred subscribers and the carefully organized format wasn’t yet what it is today.
So now it’s time to give this potent dietary compound / nutritional supplement the “Monday Research Review” treatment…
What is it?
L-theanine is an amino acid found in tea. The human body can’t produce it, and/but it’s not essential for humans. It does have a lot of benefits, though. See for example:
L-Theanine as a Functional Food Additive: Its Role in Disease Prevention and Health Promotion
How does it work?
L-theanine works by moderating and modulating the brain’s neurotransmitters.
This sounds fancy, but basically it means: it doesn’t actually add anything in the manner of a drug, but it changes how we use what we have naturally.
What does it do? Read on…
It increases mental focus
It has been believed that l-theanine requires the presence of caffeine to achieve this (i.e., it’s a combination-only effect). For example:
But as it turns out, when a group of researchers actually checked… This isn’t true, as Foxe et al. write:
❝We asked whether either compound alone, or both in combination, would affect performance of the task in terms of reduced error rates over time, and whether changes in alpha-band activity would show a relationship to such changes in performance. When treated with placebo, participants showed a rise in error rates, a pattern that is commonly observed with increasing time-on-task, whereas after caffeine and theanine ingestion, error rates were significantly reduced. The combined treatment did not confer any additional benefits over either compound alone, suggesting that the individual compounds may confer maximal benefits at the dosages employed❞
It promotes a calmly wakeful feeling of serenity
Those are not words typically found in biopharmaceutical literature, but they’re useful here to convey:
- L-theanine promotes relaxation without causing drowsiness
- L-theanine promotes mental alertness without being a stimulant
Here is where l-theanine really stands out from caffeine. If both substances promote mental focus, but one of them does it by making us “wired” and the other does it while simultaneously promoting calm, it makes the choice between them clearer!
Read more: L-theanine, a natural constituent in tea, and its effect on mental state
It relieves stress and anxiety
Building on from the above, but there’s more: l-theanine relieves stress and anxiety in people experiencing stressful situations, without any known harmful side effects… This is something that sets it apart from a lot of anxiolytic (antianxiety) drugs!
Here’s what a big systematic review of clinical trials had to say:
Theanine consumption, stress and anxiety in human clinical trials: A systematic review
L-theanine has other benefits too
We’ve talked about some of the most popular benefits of l-theanine, and we can’t make this newsletter too long, but research also suggests that it…
- Supports healthy weight management
- Reduces inflammation
- Supports immune health
- Helps fight cancer
- May extend lifespan ← this one’s a C. elegans study, but despite being a tiny worm, they actually function very similarly to humans on a cellular level; it’s why they’re used so much for anti-aging research
If you’re interested in this topic, we recommend also reading our previous article on l-theanine—pardon that we hadn’t really nailed down our style yet—but there’s a bunch of useful information about how l-theanine makes caffeine “better” in terms of benefits. We also talk dosage, and reference some other studies we didn’t have room to include today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: