Hormones & Health, Beyond The Obvious
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Wholesome Health

This is Dr. Sara Gottfried, who some decades ago got her MD from Harvard and specialized as an OB/GYN at MIT. She’s since then spent the more recent part of her career educating people (mostly: women) about hormonal health, precision, functional, & integrative medicine, and the importance of lifestyle medicine in general.
What does she want us to know?
Beyond “bikini zone health”
Dr. Gottfried urges us to pay attention to our whole health, in context.
“Women’s health” is often thought of as what lies beneath a bikini, and if it’s not in those places, then we can basically treat a woman like a man.
And that’s often not actually true—because hormones affect every living cell in our body, and as a result, while prepubescent girls and postmenopausal women (specifically, those who are not on HRT) may share a few more similarities with boys and men of similar respective ages, for most people at most ages, men and women are by default quite different metabolically—which is what counts for a lot of diseases! And note, that difference is not just “faster” or “slower””, but is often very different in manner also.
That’s why, even in cases where incidence of disease is approximately similar in men and women when other factors are controlled for (age, lifestyle, medical history, etc), the disease course and response to treatment may vary considerable. For a strong example of this, see for example:
- The well-known: Heart Attack: His & Hers ← most people know these differences exist, but it’s always good to brush up on what they actually are
- The less-known: Statins: His & Hers ← most people don’t know these differences exist, and it pays to know, especially if you are a woman or care about one
Nor are brains exempt from his…
The female brain (kinda)
While the notion of an anatomically different brain for men and women has long since been thrown out as unscientific phrenology, and the idea of a genetically different brain is… Well, it’s an unreliable indicator, because technically the cells will have DNA and that DNA will usually (but not always; there are other options) have XX or XY chromosomes, which will usually (but again, not always) match apparent sex (in about 1/2000 cases there’s a mismatch, which is more common than, say, red hair; sometimes people find out about a chromosomal mismatch only later in life when getting a DNA test for some unrelated reason), and in any case, even for most of us, the chromosomal differences don’t count for much outside of antenatal development (telling the default genital materials which genitals to develop into, though this too can get diverted, per many intersex possibilities, which is also a lot more common than people think) or chromosome-specific conditions like colorblindness…
The notion of a hormonally different brain is, in contrast to all of the above, a reliable and easily verifiable thing.
See for example:
Alzheimer’s Sex Differences May Not Be What They Appear
Dr. Gottfried urges us to take the above seriously!
Because, if women get Alzheimer’s much more commonly than men, and the disease progresses much more quickly in women than men, but that’s based on postmenopausal women not on HRT, then that’s saying “Women, without women’s usual hormones, don’t do so well as men with men’s usual hormones”.
She does, by the way, advocate for bioidentical HRT for menopausal women, unless contraindicated for some important reason that your doctor/endocrinologist knows about. See also:
Menopausal HRT: A Tale Of Two Approaches (Bioidentical vs Animal)
The other very relevant hormone
…that Dr. Gottfried wants us to pay attention to is insulin.
Or rather, its scrubbing enzyme, the prosaically-named “insulin-degrading enzyme”, but it doesn’t only scrub insulin. It also scrubs amyloid beta—yes, the same that produces the amyloid beta plaques in the brain associated with Alzheimer’s. And, there’s only so much insulin-degrading enzyme to go around, and if it’s all busy breaking down excess insulin, there’s not enough left to do the other job too, and thus can’t break down amyloid beta.
In other words: to fight neurodegeneration, keep your blood sugars healthy.
This may actually work by multiple mechanisms besides the amyloid hypothesis, by the way:
The Surprising Link Between Type 2 Diabetes & Alzheimer’s
Want more from Dr. Gottfried?
You might like this interview with Dr. Gottfried by Dr. Benson at the IMCJ:
Integrative Medicine: A Clinician’s Journal | Conversations with Sara Gottfried, MD
…in which she discusses some of the things we talked about today, and also about her shift from a pharmaceutical-heavy approach to a predominantly lifestyle medicine approach.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Can a drug like Ozempic help treat addictions to alcohol, opioids or other substances?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Semaglutide (sold as Ozempic, Wegovy and Rybelsus) was initially developed to treat diabetes. It works by stimulating the production of insulin to keep blood sugar levels in check.
This type of drug is increasingly being prescribed for weight loss, despite the fact it was initially approved for another purpose. Recently, there has been growing interest in another possible use: to treat addiction.
Anecdotal reports from patients taking semaglutide for weight loss suggest it reduces their appetite and craving for food, but surprisingly, it also may reduce their desire to drink alcohol, smoke cigarettes or take other drugs.
But does the research evidence back this up?
Animal studies show positive results
Semaglutide works on glucagon-like peptide-1 receptors and is known as a “GLP-1 agonist”.
Animal studies in rodents and monkeys have been overwhelmingly positive. Studies suggest GLP-1 agonists can reduce drug consumption and the rewarding value of drugs, including alcohol, nicotine, cocaine and opioids.
Out team has reviewed the evidence and found more than 30 different pre-clinical studies have been conducted. The majority show positive results in reducing drug and alcohol consumption or cravings. More than half of these studies focus specifically on alcohol use.
However, translating research evidence from animal models to people living with addiction is challenging. Although these results are promising, it’s still too early to tell if it will be safe and effective in humans with alcohol use disorder, nicotine addiction or another drug dependence.
What about research in humans?
Research findings are mixed in human studies.
Only one large randomised controlled trial has been conducted so far on alcohol. This study of 127 people found no difference between exenatide (a GLP-1 agonist) and placebo (a sham treatment) in reducing alcohol use or heavy drinking over 26 weeks.
In fact, everyone in the study reduced their drinking, both people on active medication and in the placebo group.
However, the authors conducted further analyses to examine changes in drinking in relation to weight. They found there was a reduction in drinking for people who had both alcohol use problems and obesity.
For people who started at a normal weight (BMI less than 30), despite initial reductions in drinking, they observed a rebound increase in levels of heavy drinking after four weeks of medication, with an overall increase in heavy drinking days relative to those who took the placebo.
There were no differences between groups for other measures of drinking, such as cravings.
Some studies show a rebound increase in levels of heavy drinking. Deman/Shutterstock In another 12-week trial, researchers found the GLP-1 agonist dulaglutide did not help to reduce smoking.
However, people receiving GLP-1 agonist dulaglutide drank 29% less alcohol than those on the placebo. Over 90% of people in this study also had obesity.
Smaller studies have looked at GLP-1 agonists short-term for cocaine and opioids, with mixed results.
There are currently many other clinical studies of GLP-1 agonists and alcohol and other addictive disorders underway.
While we await findings from bigger studies, it’s difficult to interpret the conflicting results. These differences in treatment response may come from individual differences that affect addiction, including physical and mental health problems.
Larger studies in broader populations of people will tell us more about whether GLP-1 agonists will work for addiction, and if so, for whom.
How might these drugs work for addiction?
The exact way GLP-1 agonists act are not yet well understood, however in addition to reducing consumption (of food or drugs), they also may reduce cravings.
Animal studies show GLP-1 agonists reduce craving for cocaine and opioids.
This may involve a key are of the brain reward circuit, the ventral striatum, with experimenters showing if they directly administer GLP-1 agonists into this region, rats show reduced “craving” for oxycodone or cocaine, possibly through reducing drug-induced dopamine release.
Using human brain imaging, experimenters can elicit craving by showing images (cues) associated with alcohol. The GLP-1 agonist exenatide reduced brain activity in response to an alcohol cue. Researchers saw reduced brain activity in the ventral striatum and septal areas of the brain, which connect to regions that regulate emotion, like the amygdala.
In studies in humans, it remains unclear whether GLP-1 agonists act directly to reduce cravings for alcohol or other drugs. This needs to be directly assessed in future research, alongside any reductions in use.
Are these drugs safe to use for addiction?
Overall, GLP-1 agonists have been shown to be relatively safe in healthy adults, and in people with diabetes or obesity. However side effects do include nausea, digestive troubles and headaches.
And while some people are OK with losing weight as a side effect, others aren’t. If someone is already underweight, for example, this drug might not be suitable for them.
In addition, very few studies have been conducted in people with addictive disorders. Yet some side effects may be more of an issue in people with addiction. Recent research, for instance, points to a rare risk of pancreatitis associated with GLP-1 agonists, and people with alcohol use problems already have a higher risk of this disorder.
Other drugs treatments are currently available
Although emerging research on GLP-1 agonists for addiction is an exciting development, much more research needs to be done to know the risks and benefits of these GLP-1 agonists for people living with addiction.
In the meantime, existing effective medications for addiction remain under-prescribed. Only about 3% of Australians with alcohol dependence, for example, are prescribed medication treatments such as like naltrexone, acamprosate or disulfiram. We need to ensure current medication treatments are accessible and health providers know how to prescribe them.
Continued innovation in addiction treatment is also essential. Our team is leading research towards other individualised and effective medications for alcohol dependence, while others are investigating treatments for nicotine addiction and other drug dependence.
Read the other articles in The Conversation’s Ozempic series here.
Shalini Arunogiri, Addiction Psychiatrist, Associate Professor, Monash University; Leigh Walker, , Florey Institute of Neuroscience and Mental Health, and Roberta Anversa, , The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
An Addiction Expert’s Insights On Festive Drinking
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Christopher Kahler. He’s Professor of Behavioral and Social Sciences, Director of Alcohol and Addiction Studies, Professor of Psychiatry and Human Behavior, all at Brown University.
What does he want us to know?
It’s the trickiest time of the year
Per stats, alcohol sales peak in December, with the heaviest drinking being from mid-December (getting an early start on the Christmas cheer) to New Year’s Eve. As for why, there’s a collection of reasons, as he notes:
❝The main challenge is there’s an extra layer of stress, with a lot of obligations and expectations from friends and family. We’re around people who maybe we’re not usually around, and in larger groups. It’s also a time of heightened emotion and, for some people, loneliness.
On top of that, alcohol use is built into a lot of our winter holiday traditions. It’s often marketed as part of the “good life.” We’re expected to have alcohol when we celebrate.❞
As for how much alcohol is safe to drink… According to the World Health Organization, the only safe amount of alcohol is zero:
Dr. Kahler acknowledges, however, that many people will wish to imbibe anyway, and indeed, he himself does drink a little, but endeavours to do so mindfully, and as such, he recommends that we…
HALT!
Dr. Kahler counsels us against making decisions (including the decision to drink alcohol), on occasions when we are one or more of the following:
- Hungry
- Angry
- Lonely
- Tired
He also notes that around this time of year, often our normal schedules and habits are disrupted, which introduces more microdecisions to our daily lives, which in turn means more “decision fatigue”, and the greater chance of making bad decisions.
We share some practical tips on how to reduce the chances of thusly erring, here:
Set your intentions now
He bids us figure out what our goal is, and really think it through, including not just “how many drinks to have” if we’re drinking, but also such things as “what feelings are likely to come up”. Because, if we’ve historically used alcohol as a maladaptive coping mechanism, we’re going to need a different, better, healthier coping mechanism (we talked more about that in our above-linked article about reducing or quitting alcohol, too, with some examples).
He also suggests that we memorize our social responses—exactly what we’re going to say if offered a drink, for example:
❝It’s important to know what you’re going to say about your alcohol use. If someone asks if they can get you a drink, good responses could be: “A glass of water would be great” or “Do you have any non-alcoholic cider?” You don’t have to explain yourself. Just ask for what you want, because saying no to someone can be difficult.❞
See also:
December’s Traps To Plan Around
Mix it up and slow it down
No, that doesn’t mean mix yourself a sloe gin cocktail. But rather, it’s about alternating alcoholic and non-alcoholic drinks, to give your body half a chance to process the alcohol, and also to rehydrate a little along the way.
We talk about this and other damage-limitation methods, here:
How To Reduce The Harm Of Festive Drinking (Without Abstaining)
Take care!
Share This Post
-
What’s the difference between burnout and depression?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If your summer holiday already feels like a distant memory, you’re not alone. Burnout – a state of emotional, physical and mental exhaustion following prolonged stress – has been described in workplaces since a 5th century monastery in Egypt.
Burnout and depression can look similar and are relatively common conditions. It’s estimated that 30% of the Australian workforce is feeling some level of burnout, while almost 20% of Australians are diagnosed with depression at some point in their lives.
So what’s the difference between burnout and depression?
Burnout is marked by helplessness and depression by hopelessness. They can have different causes and should also be managed differently.
Yuri A/Shutterstock What is burnout?
The World Health Organization defines burnout as an “occupational phenomenon” resulting from excessively demanding workload pressures. While it is typically associated with the workplace, carers of children or elderly parents with demanding needs are also at risk.
Our research created a set of burnout symptoms we captured in the Sydney Burnout Measure to assist self-diagnosis and clinicians undertaking assessments. They include:
- exhaustion as the primary symptom
- brain fog (poor concentration and memory)
- difficulty finding pleasure in anything
- social withdrawal
- an unsettled mood (feeling anxious and irritable)
- impaired work performance (this may be result of other symptoms such as fatigue).
People can develop a “burning out” phase after intense work demands over only a week or two. A “burnout” stage usually follows years of unrelenting work pressure.
What is depression?
A depressive episode involves a drop in self-worth, increase in self-criticism and feelings of wanting to give up. Not everyone with these symptoms will have clinical depression, which requires a diagnosis and has an additional set of symptoms.
Clinically diagnosed depression can vary by mood, how long it lasts and whether it comes back. There are two types of clinical depression:
- melancholic depression has genetic causes, with episodes largely coming “out of the blue”
- non-melancholic depression is caused by environmental factors, often triggered by significant life events which cause a drop in self-worth.
When we created our burnout measure, we compared burnout symptoms with these two types of depression.
Burnout shares some features with melancholic depression, but they tend to be general symptoms, such as feeling a loss of pleasure, energy and concentration skills.
We found there were more similarities between burnout and non-melancholic (environmental) depression. This included a lack of motivation and difficulties sleeping or being cheered up, perhaps reflecting the fact both have environmental causes.
Looking for the root cause
The differences between burnout and depression become clearer when we look at why they happen.
Personality comes into play. Our work suggests a trait like perfectionism puts people at a much higher risk of burnout. But they may be less likely to become depressed as they tend to avoid stressful events and keep things under control.
Excessive workloads can contribute to burnout. tartanparty/Shutterstock Those with burnout generally feel overwhelmed by demands or deadlines they can’t meet, creating a sense of helplessness.
On the other hand, those with depression report lowered self-esteem. So rather than helpless they feel that they and their future is hopeless.
However it is not uncommon for someone to experience both burnout and depression at once. For example, a boss may place excessive work demands on an employee, putting them at risk of burnout. At the same time, the employer may also humiliate that employee and contribute to an episode of non-melancholic depression.
What can you do?
A principal strategy in managing burnout is identifying the contributing stressors. For many people, this is the workplace. Taking a break, even a short one, or scheduling some time off can help.
Australians now have the right to disconnect, meaning they don’t have to answer work phone calls or emails after hours. Setting boundaries can help separate home and work life.
Burnout can be also be caused by compromised work roles, work insecurity or inequity. More broadly, a dictatorial organisational structure can make employees feel devalued. In the workplace, environmental factors, such as excessive noise, can be a contributor. Addressing these factors can help prevent burnout.
As for managing symptoms, the monks had the right idea. Strenuous exercise, meditation and mindfulness are effective ways to deal with everyday stress.
Regular exercise can help manage symptoms of burnout. alexei_tm/Shutterstock Deeper contributing factors, including traits such as perfectionism, should be managed by a skilled clinical psychologist.
For melancholic depression, clinicians will often recommend antidepressant medication.
For non-melancholic depression, clinicians will help address and manage triggers that are the root cause. Others will benefit from antidepressants or formal psychotherapy.
While misdiagnosis between depression and burnout can occur, burnout can mimic other medical conditions such as anemia or hypothyroidism.
For the right diagnosis, it’s best to speak to your doctor or clinician who should seek to obtain a sense of “the whole picture”. Only then, once a burnout diagnosis has been affirmed and other possible causes ruled out, should effective support strategies be put in place.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Correction: This article originally stated that depression is marked by helplessness and burnout by hopelessness, when in fact it is vice versa. This has been amended.
Gordon Parker, Scientia Professor of Psychiatry, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
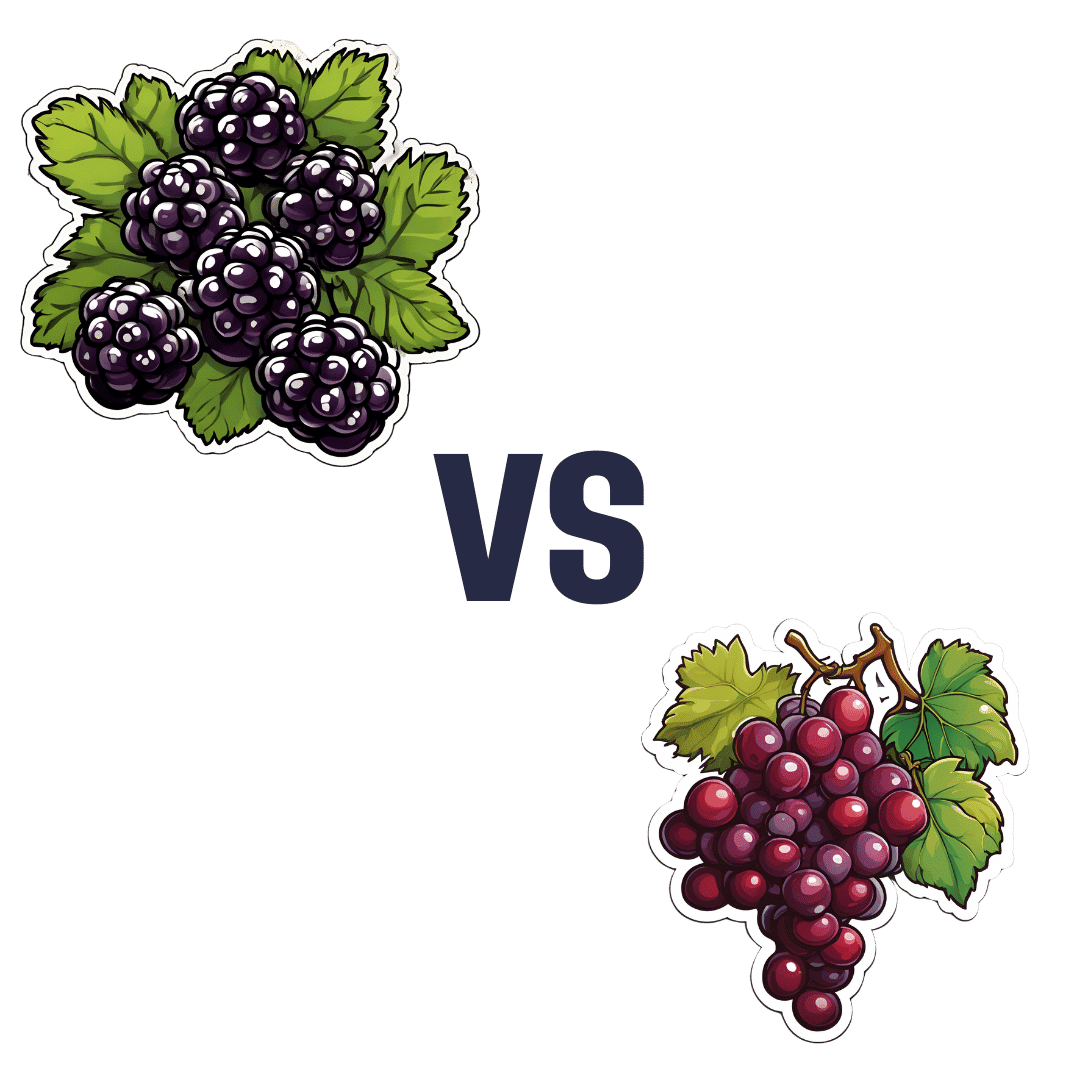
Blackberries vs Grapes – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing blackberries to grapes, we picked the blackberries.
Why?
It’s not even close:
In terms of macros, blackberries have more than 5x the fiber, for about half the carbs, resulting in a notably lower glycemic index. They also have more than 2x the protein, but unlike the fiber, it’s not much in either fruit, so we might disregard it. Still, an easy win for blackberries either way.
In the category of vitamins, blackberries have more of vitamins A, B3, B5, B9, C, E, K, and choline, while grapes have more of vitamins B1, B2, and B6. Another clear win for blackberries.
When it comes to minerals, blackberries have a lot more calcium, copper, iron, magnesium, phosphorus, selenium, and zinc, while grapes have slightly more manganese and potassium. Once again, blackberries emerge victorious.
Looking at polyphenols, both have an abundance of many polyphenols, but blackberries have more, both in types and in total mass (mg/100g).
Thus, blackberries overwhelmingly win the day, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Can We Drink To Good Health? ← while there are polyphenols such as resveratrol in red wine that per se would boost heart health, there’s so little per glass that you may need 100–1000 glasses per day to get the dosage that provides benefits in mouse studies.
If you’re not a mouse, you might even need more than that!
To this end, many people prefer resveratrol supplementation ← link is to an example product on Amazon, but there are plenty more so feel free to shop around 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Women take more antidepressants after divorce than men but that doesn’t mean they’re more depressed
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Research out today from Finland suggests women may find it harder to adjust to later-life divorce and break-ups than men.
The study used population data from 229,000 Finns aged 50 to 70 who had undergone divorce, relationship break-up or bereavement and tracked their use of antidepressants before and after their relationship ended.
They found antidepressant use increased in the four years leading to the relationship dissolution in both genders, with women experiencing a more significant increase.
But it’s too simplistic to say women experience poorer mental health or tend to be less happy after divorce than men.
Remind me, how common is divorce?
Just under 50,000 divorces are granted each year in Australia. This has slowly declined since the 1990s.
More couple are choosing to co-habitate, instead of marry, and the majority of couples live together prior to marriage. Divorce statistics don’t include separations of cohabiting couples, even though they are more likely than married couples to separate.
Those who divorce are doing so later in life, often after their children grow up. The median age of divorce increased from 45.9 in 2021 to 46.7 in 2022 for men and from 43.0 to 43.7 for women.
The trend of late divorces also reflects people deciding to marry later in life. The median duration from marriage to divorce in 2022 was around 12.8 years and has remained fairly constant over the past decade.
Why do couples get divorced?
Changes in social attitudes towards marriage and relationships mean divorce is now more accepted. People are opting not to be in unhappy marriages, even if there are children involved.
Instead, they’re turning the focus on marriage quality. This is particularly true for women who have established a career and are financially autonomous.
Similarly, my research shows it’s particularly important for people to feel their relationship expectations can be fulfilled long term. In addition to relationship quality, participants reported needing trust, open communication, safety and acceptance from their partners.
“Grey divorce” (divorce at age 50 and older) is becoming increasingly common in Western countries, particularly among high-income populations. While factors such as an empty nest, retirement, or poor health are commonly cited predictors of later-in-life divorce, research shows older couples divorce for the same reasons as younger couples.
What did the new study find?
The study tracked antidepressant use in Finns aged 50 to 70 for four years before their relationship breakdown and four years after.
They found antidepressant use increased in the four years leading to the relationship break-up in both genders. The proportion of women taking antidepressants in the lead up to divorce increased by 7%, compared with 5% for men. For de facto separation antidepressant use increased by 6% for women and 3.2% for men.
Within a year of the break-up, antidepressant use fell back to the level it was 12 months before the break-up. It subsequently remained at that level among the men.
But it was a different story for women. Their use tailed off only slightly immediately after the relationship breakdown but increased again from the first year onwards.
Women’s antidepressant use increased again.
sk/UnsplashThe researchers also looked at antidepressant use after re-partnering. There was a decline in the use of antidepressants for men and women after starting a new relationship. But this decline was short-lived for women.
But there’s more to the story
Although this data alone suggest women may find it harder to adjust to later-life divorce and break-ups than men, it’s important to note some nuances in the interpretation of this data.
For instance, data suggesting women experience depression more often than men is generally based on the rate of diagnoses and antidepressant use, which does not account for undiagnosed and unmedicated people.
Women are generally more likely to access medical services and thus receive treatment. This is also the case in Australia, where in 2020–2022, 21.6% of women saw a health professional for their mental health, compared with only 12.9% of men.
Why women might struggle more after separating
Nevertheless, relationship dissolution can have a significant impact on people’s mental health. This is particularly the case for women with young children and older women.
So what factors might explain why women might experience greater difficulties after divorce later in life?
Research investigating the financial consequences of grey divorce in men and women showed women experienced a 45% decline in their standard of living (measured by an income-to-needs ratio), whereas men’s dropped by just 21%. These declines persisted over time for men, and only reversed for women following re-partnering.
Another qualitative study investigating the lived experiences of heterosexual couples post-grey divorce identified financial worries as a common theme between female participants.
A female research participant (age 68) said:
[I am most worried about] the money, [and] what I’m going to do when the little bit of money I have runs out […] I have just enough money to live. And, that’s it, [and if] anything happens I’m up a creek. And Medicare is incredibly expensive […] My biggest expense is medicine.
Another factor was loneliness. One male research participant (age 54) described he preferred living with his ex-wife, despite not getting along with her, than being by himself:
It was still [good] knowing that [the] person was there, and now that’s gone.
Other major complications of later-life divorce are possible issues with inheritance rights and next-of-kin relationships for medical decision-making.
Separation can be positive
For some people, divorce or separation can lead to increased happiness and feeling more independent.
And the mental health impact and emotional distress of a relationship dissolution is something that can be counterattacked with resilience. Resilience to dramatic events built from life experience means older adults often do respond better to emotional distress and might be able to adjust better to divorce than their younger counterparts.
Raquel Peel, Adjunct Senior Lecturer, University of Southern Queensland and Senior Lecturer, RMIT University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
This Book May Save Your Life – by Dr. Karan Rajan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The title is a bold sell, but the book does include a lot of information about what can go wrong in your body, and how those things can be avoided.
What it’s not: a reiteration of Dr. Michael Greger’s “How Not To Die“. It’s not dense medical information, and it doesn’t cite papers at a rate of ten per page.
What it is: an easy-reading tour guide of the human body and its many quirks and foibles, and how we can leverage those to our benefit. On which note…
Hopefully, your insides will never see the light of day, but this author is a general surgeon and as such, is an experienced and well-qualified tour guide. Here, we learn about everything from the long and interesting journey through our gut, to the unique anatomical features and liabilities of the brain. From the bizarre oddities of the genitals, to things most people don’t know about the process of death.
The style of the book is very casual, with lots of short sections (almost mini chapters-within-chapters, really) making for very light reading—and certainly enjoyable reading too, unless you are inclined to squeamishness.
Bottom line: in honesty, the book is more informative than it is instructional, though it does contain the promised health tips too. With that in mind, it’s a very enjoyable and educational read, and we do recommend it.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: