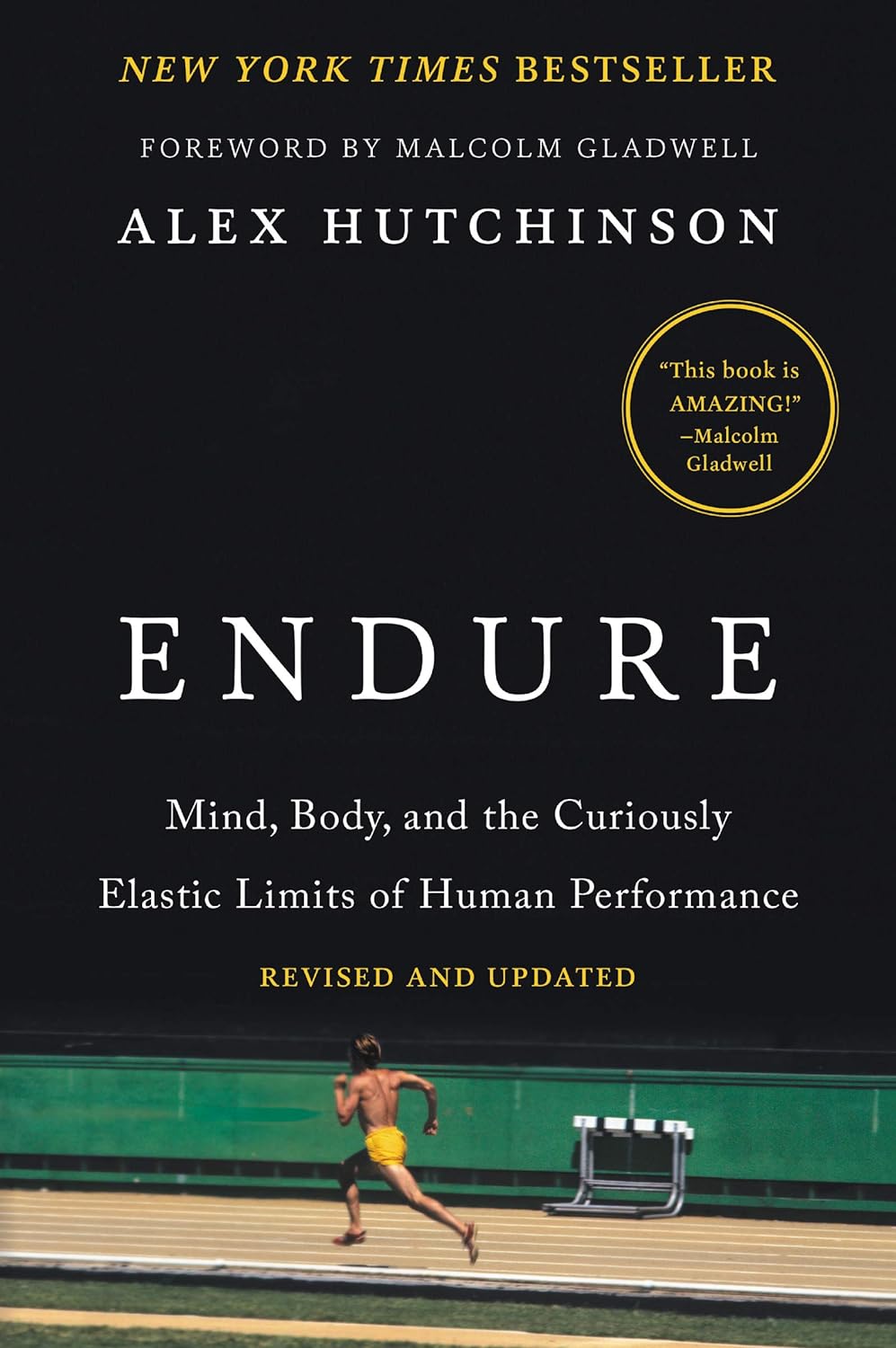
Endure – by Alex Hutchinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Life is a marathon, not a sprint. For most of us, at least. But how do we pace ourselves to go the distance, without falling into complacency along the way?
According to our author Alex Hutchinson, there’s a lot more to it than goal-setting and strategy.
Hutchinson set out to write a running manual, and ended up writing a manual for life. To be clear, this is still mostly centered around the science of athletic endurance, but covers the psychological factors as much as the physical… and notes how the capacity to endure is the key trait that underlies great performance in every field.
The writing style is both personal and personable, and parts read like a memoir (Hutchinson himself being a runner and sports journalist), while others are scientific in nature.
As for the science, the kind of science examined runs the gamut from case studies to clinical studies. We examine not just the science of physical endurance, but the science of psychological endurance too. We learn about such things as:
- How perception of ease/difficulty plays its part
- What factors make a difference to pain tolerance
- How mental exhaustion affects physical performance
- What environmental factors increase or lessen our endurance
- …and many other elements that most people don’t consider
Bottom line: whether you want to run a marathon in under two hours, or just not quit after one minute forty seconds on the exercise bike, or to get through a full day’s activities while managing chronic pain, this book can help.
Click here to check out Endure, and find out what you are capable of when you move your limits!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Bromelain vs Inflammation & Much More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s Get Fruity
Bromelain is an enzyme* found in pineapple (and only in pineapple), that has many very healthful properties, some of them unique to bromelain.
*actually a combination of enzymes, but most often referred to collectively in the singular. But when you do see it referred to as “they”, that’s what that means.
What does it do?
It does a lot of things, for starters:
❝Various in vivo and in vitro studies have shown that they are anti-edematous, anti-inflammatory, anti-cancerous, anti-thrombotic, fibrinolytic, and facilitate the death of apoptotic cells. The pharmacological properties of bromelain are, in part, related to its arachidonate cascade modulation, inhibition of platelet aggregation, such as interference with malignant cell growth; anti-inflammatory action; fibrinolytic activity; skin debridement properties, and reduction of the severe effects of SARS-Cov-2❞
Some quick notes:
- “facilitate the death of apoptotic cells” may sound alarming, but it’s actually good; those cells need to be killed quickly; see for example: Fisetin: The Anti-Aging Assassin
- If you’re wondering what arachidonate cascade modulation means, that’s the modulation of the cascade reaction of arachidonic acid, which plays a part in providing energy for body functions, and has a role in cell structure formation, and is the precursor of assorted inflammatory mediators and cell-signalling chemicals.
- Its skin debridement properties (getting rid of dead skin) are most clearly seen when using bromelain topically (one can literally just make a pineapple poultice), but do occur from ingestion also (because of what it can do from the inside).
- As for being anti-thrombotic and fibrinolytic, let’s touch on that before we get to the main item, its anti-inflammatory properties.
If you want to read more of the above before moving on, though, here’s the full text:
Anti-thrombotic and fibrinolytic
While it does have anti-thrombotic effects, largely by its fibrinolytic action (i.e., it dissolves the fibrin mesh holding clots together), it can have a paradoxically beneficial effect on wound healing, too:
For more specifically on its wound-healing benefits:
In Vitro Effect of Bromelain on the Regenerative Properties of Mesenchymal Stem Cells
Anti-inflammatory
Bromelain is perhaps most well-known for its anti-inflammatory powers, which are so diverse that it can be a challenge to pin them all down, as it has many mechanisms of action, and there’s a large heterogeneity of studies because it’s often studied in the context of specific diseases. But, for example:
❝Bromelain reduced IL-1β, IL-6 and TNF-α secretion when immune cells were already stimulated in an overproduction condition by proinflammatory cytokines, generating a modulation in the inflammatory response through prostaglandins reduction and activation of cascade reactions that trigger neutrophils and macrophages, in addition to accelerating the healing process❞
~ Dr. Taline Alves Nobre et al.
Read in full:
Bromelain as a natural anti-inflammatory drug: a systematic review
Or if you want a more specific example, here’s how it stacks up against arthritis:
❝The results demonstrated the chondroprotective effects of bromelain on cartilage degradation and the downregulation of inflammatory cytokine (tumor necrosis factor (TNF)-α, IL-1β, IL-6, IL-8) expression in TNF-α–induced synovial fibroblasts by suppressing NF-κB and MAPK signaling❞
~ Dr. Perephan Pothacharoen et al.
Read in full:
More?
Yes more! You’ll remember from the first paper we quoted today, that it has a long laundry list of benefits. However, there’s only so much we can cover in one edition, so that’s it for today
Is it safe?
It is generally recognized as safe. However, its blood-thinning effect means it should be avoided if you’re already on blood-thinners, have some sort of bleeding disorder, or are about to have a surgery.
Additionally, if you have a pineapple allergy, this one may not be for you.
Aside from that, anything can have drug interactions, so do check with your doctor/pharmacist to be sure (with the pharmacist usually being the more knowledgeable of the two, when it comes to drug interactions).
Want to try some?
You can just eat pineapples, but if you don’t enjoy that and/or wouldn’t want it every day, bromelain is available in supplement form too.
We don’t sell it, but here for your convenience is an example product on Amazon
Enjoy!
Share This Post
-
The Easiest Way To Take Up Journaling
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dear Diary…
It’s well-established that journaling is generally good for mental health. It’s not a magical panacea, as evidenced by The Diaries of Franz Kafka for example (that man was not in good mental health). But for most of us, putting our thoughts and feelings down on paper (or the digital equivalent) is a good step for tidying our mind.
And as it can be said: mental health is also just health.
But…
What to write about?
It’s about self-expression (even if only you will read it), and…
❝Writing about traumatic, stressful or emotional events has been found to result in improvements in both physical and psychological health, in non-clinical and clinical populations.
In the expressive writing paradigm, participants are asked to write about such events for 15–20 minutes on 3–5 occasions.
Those who do so generally have significantly better physical and psychological outcomes compared with those who write about neutral topics.❞
Source: Emotional and physical health benefits of expressive writing
In other words, write about whatever moves you.
Working from prompts
If you read the advice above and thought “but I don’t know what moves me”, then fear not. It’s perfectly respectable to work from prompts, such as:
- What last made you cry?
- What last made you laugh?
- What was a recent meaningful moment with family?
- What is a serious mistake that you made and learned from?
- If you could be remembered for just one thing, what would you want it to be?
In fact, sometimes working from prompts has extra benefits, precisely because it challenges us to examine things we might not otherwise think about.
If a prompt asks “What tends to bring you most joy recently?” and the question stumps you, then a) you now are prompted to look at what you can change to find more joy b) you probably wouldn’t have thought of this question—most depressed people don’t, and if you cannot remember recent joy, then well, we’re not here to diagnose, but let’s just say that’s a symptom.
A quick aside: if you or a loved oneare prone to depressive episodes, here’s a good resource, by the way:
The Mental Health First-Aid That You’ll Hopefully Never Need
And in the event of the mental health worst case scenario:
The six prompts we gave earlier are just ideas that came to this writer’s mind, but they’re (ok, some bias here) very good ones. If you’d like more though, here’s a good resource:
550+ Journal Prompts: The Ultimate List
The Good, The Bad, and The Ugly
While it’s not good to get stuck in ruminative negative thought spirals, it is good to have a safe outlet to express one’s negative thoughts/feelings:
Remember, your journal is (or ideally, should be) a place without censure. If you fear social consequences should your journal be read, then using an app with a good security policy and encryption options can be a good idea for journaling
Finch App is a good free option if it’s not too cutesy for your taste, because in terms of security:
- It can’t leak your data because your data never leaves your phone (unless you manually back up your data and then you choose to put it somewhere unsafe)
- It has an option to require passcode/biometrics etc to open the app
As a bonus, it also has very many optional journaling prompts, and also (optional) behavioral activation prompts, amongst more other offerings that we don’t have room to list here.
Take care!
Share This Post
-
Protein: How Much Do We Need, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mythbusting Protein!
Yesterday, we asked you for your policy on protein consumption. The distribution of responses was as follows:
- A marginal majority (about 55%) voted for “Protein is very important, but we can eat too much of it”
- A large minority (about 35%) voted for “We need lots of protein; the more, the better!”
- A handful (about 4%) voted for “We should go as light on protein as possible”
- A handful (6%) voted for “If we don’t eat protein, our body will create it from other foods”
So, what does the science say?
If we don’t eat protein, our body will create it from other foods: True or False?
Contingently True on an absurd technicality, but for all practical purposes False.
Our body requires 20 amino acids (the building blocks of protein), 9 of which it can’t synthesize and absolutely must get from food. Normally, we get those amino acids from protein in our diet, and we can also supplement them by buying amino acid supplements.
Specifically, we require (per kg of bodyweight) a daily average of:
- Histidine: 10 mg
- Isoleucine: 20 mg
- Leucine: 39 mg
- Lysine: 30 mg
- Methionine: 10.4 mg
- Phenylalanine*: 25 mg
- Threonine: 15 mg
- Tryptophan: 4 mg
- Valine: 26 mg
*combined with the non-essential amino acid tyrosine
Source: Protein and Amino Acid Requirements In Human Nutrition: WHO Technical Report
However, to get the requisite amino acid amounts, without consuming actual protein, would require gargantuan amounts of supplementation (bearing in mind bioavailability will never be 100%, so you’ll always need to take more than it seems), using supplements that will have been made by breaking down proteins anyway.
So unless you live in a laboratory and have access to endless amounts of all of the required amino acids (you can’t miss even one; you will die), and are willing to do that for the sake of proving a point, then you do really need to eat protein.
Your body cannot, for example, simply break down sugar and use it to make the protein you need.
On another technical note… Do bear in mind that many foods that we don’t necessarily think of as being sources of protein, are sources of protein.
Grains and grain products, for example, all contain protein; we just don’t think of them as that because their macronutritional profile is heavily weighted towards carbohydrates.
For that matter, even celery contains protein. How much, you may ask? Almost none! But if something has DNA, it has protein. Which means all plants and animals (at least in their unrefined forms).
So again, to even try to live without protein would very much require living in a laboratory.
We can eat too much protein: True or False?
True. First on an easy technicality; anything in excess is toxic. Even water, or oxygen. But also, in practical terms, there is such a thing as too much protein. The bar is quite high, though:
❝Based on short-term nitrogen balance studies, the Recommended Dietary Allowance of protein for a healthy adult with minimal physical activity is currently 0.8 g protein per kg bodyweight per day❞
❝To meet the functional needs such as promoting skeletal-muscle protein accretion and physical strength, dietary intake of 1.0, 1.3, and 1.6 g protein per kg bodyweight per day is recommended for individuals with minimal, moderate, and intense physical activity, respectively❞
❝Long-term consumption of protein at 2 g per kg bodyweight per day is safe for healthy adults, and the tolerable upper limit is 3.5 g per kg bodyweight per day for well-adapted subjects❞
❝Chronic high protein intake (>2 g per kg bodyweight per day for adults) may result in digestive, renal, and vascular abnormalities and should be avoided❞
Source: Dietary protein intake and human health
To put this into perspective, if you weigh about 160lbs (about 72kg), this would mean eating more than 144g protein per day, which grabbing a calculator means about 560g of lean beef, or 20oz, or 1¼lb.
If you’re eating quarter-pounder burgers though, that’s not usually so lean, so you’d need to eat more than nine quarter-pounder burgers per day to get too much protein.
High protein intake damages the kidneys: True or False?
True if you have kidney damage already; False if you are healthy. See for example:
- Effects of dietary protein restriction on the progression of advanced renal disease in the modification of diet in renal disease study
- A high protein diet has no harmful effects: a one-year crossover study in healthy male athletes
High protein intake increases cancer risk: True or False?
True or False depending on the source of the protein, so functionally false:
- Eating protein from red meat sources has been associated with higher risk for many cancers
- Eating protein from other sources has been associated with lower risk for many cancers
Source: Red Meat Consumption and Mortality Results From 2 Prospective Cohort Studies
High protein intake increase risk of heart disease: True or False?
True or False depending on the source of the protein, so, functionally false:
- Eating protein from red meat sources has been associated with higher risk of heart disease
- Eating protein from other sources has been associated with lower risk of heart disease
Source: Major Dietary Protein Sources and Risk of Coronary Heart Disease in Women
In summary…
Getting a good amount of good quality protein is important to health.
One can get too much, but one would have to go to extremes to do so.
The source of protein matters:
- Red meat is associated with many health risks, but that’s not necessarily the protein’s fault.
- Getting plenty of protein from (ideally: unprocessed) sources such as poultry, fish, and/or plants, is critical to good health.
- Consuming “whole proteins” (that contain all 9 amino acids that we can’t synthesize) are best.
Learn more: Complete proteins vs. incomplete proteins (explanation and examples)
Share This Post
Related Posts
-
What Curiosity Really Kills
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Curiosity Kills The Neurodegeneration
Of the seven things that Leonardo da Vinci considered most important for developing and maintaining the mind, number one on his list was curiosity, and we’re going to be focussing on that today.
In case you are curious about what seven things made Leonardo’s* list, they were:
- Curiosità: an insatiably curious approach to life and an unrelenting quest for continuous learning
- Dimostrazione: a commitment to test knowledge through experience, persistence, and a willingness to learn from mistakes
- Sensazione: the continual refinement of the senses, especially sight, as a means to enliven experience
- Sfumato: (lit: “gone up in smoke”) a willingness to embrace ambiguity, paradox, and uncertainty
- Arte/Scienza: the curated balance of art and science, imagination and logic
- Corporalità: the cultivation of physical grace, ambidexterity, and fitness
- Connessione: a recognition of and appreciation for the interconnectedness of phenomena (systems-based thinking)
*In case you are curious why we wrote “Leonardo” and not “da Vinci” as per our usual convention of shortening names to last names, da Vinci is not technically a name, in much the same way as “of Nazareth” was not a name.
You can read more about all 7 of these in a book that we’ve reviewed previously:
How to Think Like Leonardo da Vinci: Seven Steps to Genius Every Day – by Michael J. Gelb
But for now, let’s take on “curiosity”!
If you need an extra reason to focus on growing and nurturing your curiosity, it was also #1 of Dr. Daniel Levitin’s list of…
The Five Keys Of Aging Healthily
…and that’s from a modern-day neuroscientist whose research focuses on aging, the brain, health, productivity, and creativity.
But how do we foster curiosity in the age of Google?
Curiosity is like a muscle: use it or lose it
While it’s true that many things can be Googled to satisfy one’s curiosity in an instant…
- do you? It’s only useful if you do use it
- is the top result on Google reliable?
- there are many things that aren’t available there
In short: douse “fast
foodinformation” sources, but don’t rely on them! Not just for the sake of having correct information, but also: for the actual brain benefits which is what we are aiming for here with today’s article.If you want the best brain benefits, dive in, and go deep
Here at 10almonds we often present superficial information, with links to deeper information (often: scholarly articles). We do this because a) there’s only so much we can fit in our articles and b) we know you only have so much time available, and/but may choose to dive deeper.
Think of it in layers, e.g:
- Collagen is good for joints and bones
- Collagen is a protein made of these amino acids that also requires these vitamins and minerals to be present in order to formulate it
- Those amino acids are needed in these quantities, of which this particular one is usually the weakest link that might need supplementing, and those vitamins and minerals need to be within this period of time, but not these ones at the exact same time, or else it will disrupt the process of collagen synthesis
(in case you’re curious, we covered this here and here and offered a very good, very in-depth book about it here)
Now, this doesn’t mean that to have a healthy brain you need to have the equivalent knowledge of an anatomy & physiology degree, but it is good to have that level of curiosity in at least some areas of your life—and the more, the better.
Top tips for developing a habit of curiosity
As you probably know, most of our endeavors as humans go best when they are habits:
How To Really Pick Up (And Keep!) Those Habits
And as for specifically building a habit of curiosity:
- Make a deal with yourself that when someone is excited to tell you what they know about something (no matter whether it is your grandkid, or the socially awkward nerd at a party, or whoever), listen and learn, no matter the topic.
- Learn at least one language other than your native language (presumably English for most of our readers). Not only does learning a language convey a lot of brain benefits of its own, but also, it is almost impossible to separate language learning from cultural learning, and so you will learn a lot about another culture too, and have whole new worlds opened up to you. Again, more is better, but one second language is already a lot better than none.
- Make a regular habit of going to your local library, and picking out a non-fiction book to take home and read. This has an advantage over a bookshop, by the way (and not just that the library is free): since library books must be returned, you will keep going back, and build a habit of taking out books.
- Pick a skill that you’d like to make into a fully-fledged hobby, and commit to continually learning as much about it as you can. We already covered language-learning above, but others might include: gardening (perhaps a specific kind), cooking (perhaps a specific kind), needlecraft (perhaps a specific kind), dance (perhaps a specific kind). You could learn a musical instrument. Or it could be something very directly useful, like learning to be a first responder in case of emergencies, and committing to continually learning more about it (because there is always more to learn).
And when it comes to the above choices… Pick things that excite you, regardless of how practical or not they are. Because that stimulation that keeps on driving you? That’s what keeps your brain active, healthy, and sharp.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Early Dementia Screening From Your Blood & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dementia is, statistically speaking, the most feared disease in the US. Notwithstanding…
- heart disease killing more
- COVID being more of a lottery
- cancer being the “yes you can modify risk factors but it can come for anyone” life-changing (and often life-ending) disease,
…it’s still dementia that Americans report fearing the most.
And yet… Early dementia screening is seriously underused
It may be a case of a head-in-sand approach to avoid unwanted news, or it could be a case of not knowing what’s available.
So, with that in mind…
How to watch out: first line warning signs
You walk into a room of your house, and suddenly stop: “what did I come in here for?”, you wonder.
A moment later, you’re worrying whether this is a sign of age-related cognitive decline.
The good news: it usually isn’t. In fact, you did that when you were younger, too, you just didn’t pay enough attention at the time to remember it now.
Dementia-related memory loss is less “where did I put my car keys?”, and more “what is this thing for?” (it’s your car keys). Or at a less advanced stage: “whose are these car keys?” (they are yours).
You can read about some of the nuances here:
Is It Dementia? Spot The Signs (Because None Of Us Are Immune) ← If you’d like an objective test of memory and other cognitive impairments, this article also has a link to the industry’s gold standard test (it’s free)
(The Self-Administered Gerocognitive Exam (SAGE) is designed to detect early signs of cognitive, memory or thinking impairments)
Tests you can’t do at home
We wrote a little while back about how one kind of blood testing for Alzheimer’s disease works:
The Brain Alarm Signs That Warn Of Dementia
Why “Brain Alarm Signs” if it’s a blood test? Because the blood gets (in very lay terms) bits of broken brain in it. Or more specifically, they tested the blood for density of cerebrovascular endothelial extracellular vesicles (CEEVs), which are bits of the cells from the lining of blood vessels in the brain. These cerebrovascular endothelial extracellular vesicles should not, ideally, be falling off and riding around your bloodstream, and the greater the density of them, the greater likelihood of mild cognitive impairment now, and by extension, dementia later.
It’s not the only blood test available though, see:
Highly accurate blood test for Alzheimer’s disease is similar or superior to clinical cerebrospinal fluid (CSF) tests ← this one checks the ratio of phosporylated-tau217 to non-phosphorylated tau (which is a protein antibody), which equalled or outperformed FDA-approved CSF tests in classifying amyloid-β positron emission topography (PET, as in a PET scan) status, with a confidence interval as high as, or better than, industry standards.
If you don’t like having your blood taken, trust us that you’d find having your cerebrospinal fluid taken even less enjoyable, so this is a very welcome improvement!
In case you’re curious about how the CSF test works, here you go: NPTX2 in Cerebrospinal Fluid Predicts the Progression From Normal Cognition to Mild Cognitive Impairment ← NPTX2 is a protein biomarker of Alzheimer’s risk
…but again, we really think the blood test is preferable.
Tests beyond the physiological
There are, of course, psychological tests that can be done, including a linguistic analysis of your conversation, compared with a vast database of other people’s conversations, with and without various degrees of cognitive impairment
As Dr. Ioannis Paschalidis explains:
❝We wanted to predict what would happen in the next six years—and we found we can reasonably make that prediction with relatively good confidence and accuracy.
Rather than using acoustic features of speech, like enunciation or speed, the model is just pulling from the content of the interview—the words spoken, how they’re structured.
You can think of the score as the likelihood, the probability, that someone will remain stable or transition to dementia. It had significant predictive ability.
Digital is the new blood. You can collect it, analyze it for what is known today, store it, and reanalyze it for whatever new emerges tomorrow.❞
You can read the full paper here: Prediction of Alzheimer’s disease progression within 6 years using speech: A novel approach leveraging language models
See also: AI: The Doctor That Never Tires?
What if the news isn’t good?
While bad news is never welcome per se, it is preferable to not knowing, insofar as we can then take steps to manage the situation.
You may be wondering: what can be done that I wouldn’t already be doing to minimize my dementia risk in the first place?
And the answer is: yes, do continue those things of course, but there is more to do:
See: Beyond Guarding Against Dementia: When Age’s Brain-Changes Come Knocking
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
4 ways to cut down on meat when dining out – and still make healthy choices
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many of us are looking for ways to eat a healthier and more sustainable diet. And one way to do this is by reducing the amount of meat we eat.
That doesn’t mean you need to become a vegan or vegetarian. Our recent research shows even small changes to cut down on meat consumption could help improve health and wellbeing.
But not all plant-based options are created equal and some are ultra-processed. Navigating what’s available when eating out – including options like tofu and fake meats – can be a challenge.
So what are your best options at a cafe or restaurant? Here are some guiding principles to keep in mind when cutting down on meat.
Mikhaylovskiy/Shutterstock Health benefits to cutting down
Small amounts of lean meat can be part of a healthy, balanced diet. But the majority of Australians still eat more meat than recommended.
Only a small percentage of Australians (10%) are vegetarian or vegan. But an increasing number opt for a flexitarian diet. Flexitarians eat a diet rich in fruits and vegetables, while still enjoying small amounts of meat, dairy, eggs and fish.
Our recent research looked at whether the average Australian diet would improve if we swapped meat and dairy for plant-based alternatives, and the results were promising.
The study found health benefits when people halved the amount of meat and dairy they ate and replaced them with healthy plant-based foods, like tofu or legumes. On average, their dietary fibre intake – which helps with feeling fuller for longer and digestive health – went up. Saturated fats – which increase our blood cholesterol levels, a risk factor for heart disease – went down.
Including more fibre and less saturated fat helps reduce the risk of heart disease.
Achieving these health benefits may be as simple as swapping ham for baked beans in a toastie for lunch, or substituting half of the mince in your bolognese for lentils at dinner.
Filling your plate with fibre-rich foods can help lower cholesterol. Wally Pruss/Shutterstock How it’s made matters
For a long time we’ve known processed meats – such as ham, bacon and sausages – are bad for your health. Eating high amounts of these foods is associated with poor heart health and some forms of cancer.
But the same can be true of many processed meat alternatives.
Plant-based alternatives designed to mimic meat, such as sausages and burgers, have become readily available in supermarkets, cafes and restaurants. These products are ultra-processed and can be high in salt and saturated fat.
Our study found when people replaced meat and dairy with ultra-processed meat alternatives – such as plant-based burgers or sausages – they ate more salt and less calcium, compared to eating meat or healthy plant-based options.
So if you’re cutting down on meat for health reasons, it’s important to think about what you’re replacing it with. The Australian Dietary Guidelines recommend eggs, legumes/beans, tofu, nuts and seeds.
Tofu can be a great option. But we recommend flavouring plain tofu with herbs and spices yourself, as pre-marinated products are often ultra-processed and can be high in salt.
What about when dining out?
When you’re making your own food, it’s easier to adapt recipes or reduce the amount of meat. But when faced with a menu, it can be difficult to work out what is the best option.
Eating a range of colours is one way to ensure variety. Mikhail Nilov/Pexels Here are our four ways to make healthy choices when you eat out:
1. Fill half your plate with vegetables
When cutting down on meat, aim for half your plate to be vegetables. Try to also eat a variety of colours, such as leafy green spinach, red capsicum and pumpkin.
When you’re out, this might look like choosing a vegetable-based entree, a stir-fry or ordering a side salad to have with your meal.
2. Avoid the deep fryer
The Australian Dietary Guidelines recommend limiting deep fried foods to once a week or less. When dining out, choose plant-based options that are sautéed, grilled, baked, steamed, boiled or poached – instead of those that are crumbed or battered before deep frying.
This could mean choosing vegetarian dumplings that are steamed not fried, or poached eggs at brunch instead of fried. Ordering a side of roast vegetables instead of hot chips is also a great option.
3. Pick wholegrains
Scan the menu for wholegrain options such as brown rice, wholemeal pizza or pasta, barley, quinoa or wholemeal burger buns. Not only are they good sources of protein, but they also provide more dietary fibre than refined grains, which help keep you fuller for longer.
4. If you do pick meat – choose less processed kinds
You may not always want, or be able, to make a vegetarian choice when eating out and with other people. If you do opt for meat, it’s better to steer clear of processed options like bacon or sausages.
If sharing dishes with other people, you could try adding unprocessed plant-based options into the mix. For example, a curry with lentils or chickpeas, or a vegetable-based pizza instead of one with ham or salami. If that’s not an option, try choose meat that’s a lean cut, such as chicken breast, or options which are grilled rather than fried.
Laura Marchese, PhD candidate at the Institute for Physical Activity and Nutrition, Deakin University and Katherine Livingstone, NHMRC Emerging Leadership Fellow and Senior Research Fellow at the Institute for Physical Activity and Nutrition, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: