The Brain-Gut Highway: A Two-Way Street
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Brain-Gut Two-Way Highway
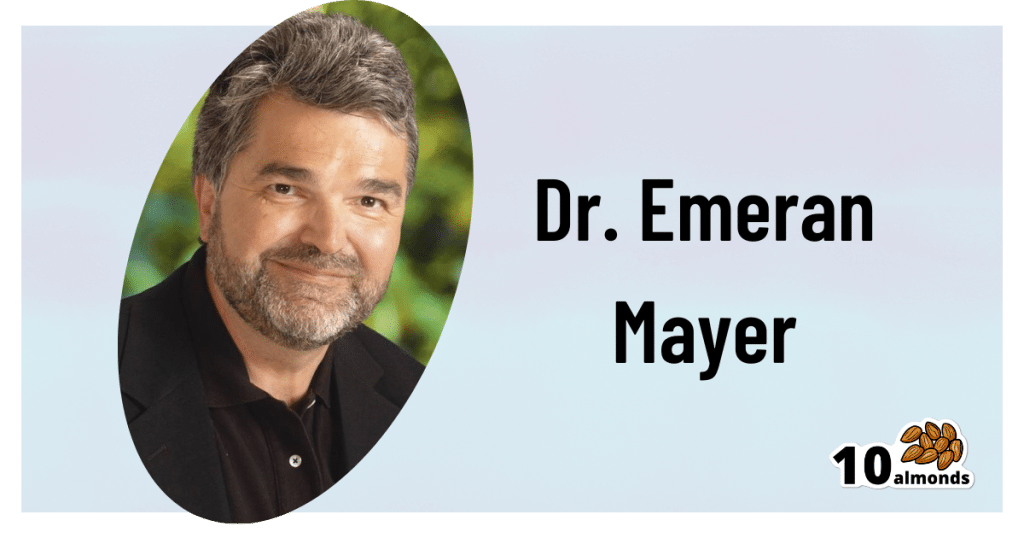
This is Dr. Emeran Mayer. He has the rather niche dual specialty of being a gastroenterologist and a neurologist. He has published over 353 peer reviewed scientific articles, and he’s a professor in the Departments of Medicine, Physiology, and Psychiatry at UCLA. Much of his work has been pioneering medical research into gut-brain interactions.
We know the brain and gut are connected. What else does he want us to know?
First, that it is a two-way interaction. It’s about 90% “gut tells the brain things”, but it’s also 10% “brain tells the gut things”, and that 10% can make more like a 20% difference, if for example we look at the swing between “brain using that 10% communication to tell gut to do things worse” or “brain using that 10% communication to tell gut to do things better”, vs the midpoint null hypothesis of “what the gut would be doing with no direction from the brain”.
For example, if we are experiencing unmanaged chronic stress, that is going to tell our gut to do things that had an evolutionary advantage 20,000–200,000 years ago. Those things will not help us now. We do not need cortisol highs and adrenal dumping because we ate a piece of bread while stressed.
Read more (by Dr. Mayer): The Stress That Evolution Has Not Prepared Us For
With this in mind, if we want to look after our gut, then we can start before we even put anything in our mouths. Dr. Mayer recommends managing stress, anxiety, and depression from the head downwards as well as from the gut upwards.
Here’s what we at 10almonds have written previously on how to manage those things:
- No-Frills, Evidence-Based Mindfulness
- How To Set Anxiety Aside
- The Mental Health First-Aid You’ll Hopefully Never Need
Do eat for gut health! Yes, even if…
Unsurprisingly, Dr. Mayer advocates for a gut-friendly, anti-inflammatory diet. We’ve written about these things before:
…but there’s just one problem:
For some people, such as with IBS, Crohn’s, and colitis, the Mediterranean diet that we (10almonds and Dr. Mayer) generally advocate for, is inaccessible. If you (if you have those conditions) eat as we describe, a combination of the fiber in many vegetables and the FODMAPs* in many fruits, will give you a very bad time indeed.
*Fermentable Oligo-, Di-, Monosaccharides And Polyols
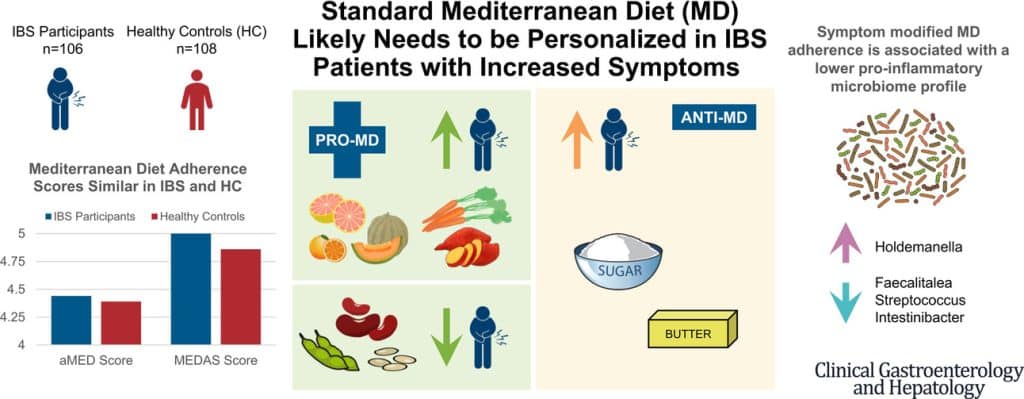
Dr. Mayer has the answer to this riddle, and he’s not just guessing; he and his team did science to it. In a study with hundreds of participants, he measured what happened with adherence (or not) to the Mediterranean diet (or modified Mediterranean diet) (or not), in participants with IBS (or not).
The results and conclusions from that study included:
❝Among IBS participants, a higher consumption of fruits, vegetables, sugar, and butter was associated with a greater severity of IBS symptoms. Multivariate analysis identified several Mediterranean Diet foods to be associated with increased IBS symptoms.
A higher adherence to symptom-modified Mediterranean Diet was associated with a lower abundance of potentially harmful Faecalitalea, Streptococcus, and Intestinibacter, and higher abundance of potentially beneficial Holdemanella from the Firmicutes phylum.
A standard Mediterranean Diet was not associated with IBS symptom severity, although certain Mediterranean Diet foods were associated with increased IBS symptoms. Our study suggests that standard Mediterranean Diet may not be suitable for all patients with IBS and likely needs to be personalized in those with increased symptoms.❞
In graphical form:
And if you’d like to read more about this (along with more details on which specific foods to include or exclude to get these results), you can do so…
- The study itself (full article): The Association Between a Mediterranean Diet and Symptoms of Irritable Bowel Syndrome
- Dr. Mayer’s blog (lay explanation): The Benefits of a Modified Mediterranean Diet for Irritable Bowel Syndrome
Want to know more?
Dr. Mayer offers many resources, including a blog, books, recipes, podcasts, and even a YouTube channel:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Weight Vests Against Osteoporosis: Do They Really Build Bone?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Doug Lucas is a dual board-certified physician specializing in optimizing healthspan and bone health for women experiencing osteoporosis, perimenopause, and menopause. Here, he talks weight vests:
Worth the weight?
Dr. Lucas cites “Wolf’s Law”—bones respond to stress. A weighted vest adds stress, to help build bone density. That said, they may not be suitable for everyone (for example, in cases of severe osteoporosis or a recent vertebral fracture).
He also cites some studies:
- Erlanger Fitness Study (2004): participants with a weighted vest maintained or improved bone density compared to a control group, but there was no group with exercise alone, making it unclear if the vest itself had the biggest impact.
- Newer studies (2016, 2017): showed improved outcomes for groups wearing a weighted vest, but again lacked an exercise-only group for comparison.
- 2012 study: included three groups (control, weighted vest, exercise only). Results showed no significant bone density difference between vest and exercise-only groups, though the vest group showed better balance and motor control.
Dr. Lucas concludes that weighted vests are a useful tool while nevertheless not being a magic bullet for bone health. In other words, they can complement exercise but you will also be fine without. If you do choose to level-up your exercise by using a weight vest, then starting with 5–10% of body weight in a vest is often recommended, but it depends on individual circumstances. If in doubt, start low and build up. Wearing the vest for daily activities can be effective, but improper use (awkward positions or improper impact training) can increase injury risk, so do be careful with that.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Osteoporosis & Exercises: Which To Do (And Which To Avoid)
- One More Resource Against Osteoporosis!
- The Osteoporosis Breakthrough – by Dr. Doug Lucas ← we reviewed his book a while back!
Take care!
Share This Post
-
Grains: Bread Of Life, Or Cereal Killer?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Going Against The Grain?
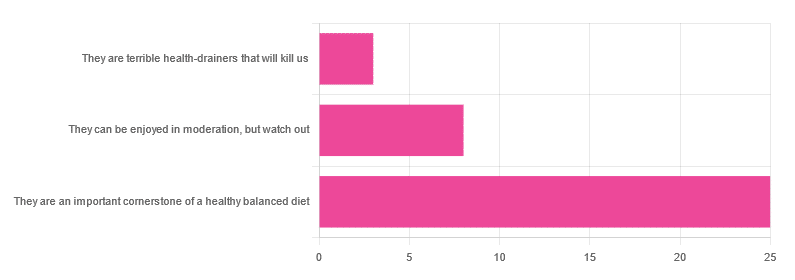
In Wednesday’s newsletter, we asked you for your health-related opinion of grains (aside from any gluten-specific concerns), and got the above-depicted, below-described, set of responses:
- About 69% said “They are an important cornerstone of a healthy balanced diet”
- About 22% said “They can be enjoyed in moderation, but watch out”
- About 8% said “They are terrible health-drainers that will kill us”
So, what does the science say?
They are terrible health-drainers that will kill us: True or False?
True or False depending on the manner of their consumption!
There is a big difference between the average pizza base and a bowl of oats, for instance. Or rather, there are a lot of differences, but what’s most critical here?
The key is: refined and ultraprocessed grains are so inferior to whole grains as to be actively negative for health in most cases for most people most of the time.
But! It’s not because processing is ontologically evil (in reality: some processed foods are healthy, and some unprocessed foods are poisonous). although it is a very good general rule of thumb.
So, we need to understand the “why” behind the “key” that we just gave above, and that’s mostly about the resultant glycemic index and associated metrics (glycemic load, insulin index, etc).
In the case of refined and ultraprocessed grains, our body gains sugar faster than it can process it, and stores it wherever and however it can, like someone who has just realised that they will be entertaining a houseguest in 10 minutes and must tidy up super-rapidly by hiding things wherever they’ll fit.
And when the body tries to do this with sugar from refined grains, the result is very bad for multiple organs (most notably the liver, but the pancreas takes quite a hit too) which in turn causes damage elsewhere in the body, not to mention that we now have urgently-produced fat stored in unfortunate places like our liver and abdominal cavity when it should have gone to subcutaneous fat stores instead.
In contrast, whole grains come with fiber that slows down the absorption of the sugars, such that the body can deal with them in an ideal fashion, which usually means:
- using them immediately, or
- storing them as muscle glycogen, or
- storing them as subcutaneous fat
👆 that’s an oversimplification, but we only have so much room here.
For more on this, see:
Glycemic Index vs Glycemic Load vs Insulin Index
And for why this matters, see:
Which Sugars Are Healthier, And Which Are Just The Same?
And for fixing it, see:
They can be enjoyed in moderation, but watch out: True or False?
Technically True but functionally False:
- Technically true: “in moderation” is doing a lot of heavy lifting here. One person’s “moderation” may be another person’s “abstemiousness” or “gluttony”.
- Functionally false: while of course extreme consumption of pretty much anything is going to be bad, unless you are Cereals Georg eating 10,000 cereals each day and being a statistical outlier, the issue is not the quantity so much as the quality.
Quality, we discussed above—and that is, as we say, paramount. As for quantity however, you might want to know a baseline for “getting enough”, so…
They are an important cornerstone of a healthy balanced diet: True or False?
True! This one’s quite straightforward.
3 servings (each being 90g, or about ½ cup) of whole grains per day is associated with a 22% reduction in risk of heart disease, 5% reduction in all-cause mortality, and a lot of benefits across a lot of disease risks:
❝This meta-analysis provides further evidence that whole grain intake is associated with a reduced risk of coronary heart disease, cardiovascular disease, and total cancer, and mortality from all causes, respiratory diseases, infectious diseases, diabetes, and all non-cardiovascular, non-cancer causes.
These findings support dietary guidelines that recommend increased intake of whole grain to reduce the risk of chronic diseases and premature mortality.❞
~ Dr. Dagfinn Aune et al.
We’d like to give a lot more sources for the same findings, as well as papers for all the individual claims, but frankly, there are so many that there isn’t room. Suffice it to say, this is neither controversial nor uncertain; these benefits are well-established.
Here’s a very informative pop-science article, that also covers some of the things we discussed earlier (it shows what happens during refinement of grains) before getting on to recommendations and more citations for claims than we can fit here:
Harvard School Of Public Health | Whole Grains
“That’s all great, but what if I am concerned about gluten?”
There certainly are reasons you might be, be it because of a sensitivity, allergy, or just because perhaps you’d like to know more.
Let’s first mention: not all grains contain gluten, so it’s perfectly possible to enjoy naturally gluten-free grains (such as oats and rice) as well as gluten-free pseudocereals, which are not actually grains but do the same job in culinary and nutritional terms (such as quinoa and buckwheat, despite the latter’s name).
Finally, if you’d like to know more about gluten’s health considerations, then check out our previous mythbusting special:
Enjoy!
Share This Post
-
Imposter Syndrome (and why almost everyone has it)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Imposter Syndrome (and why almost everyone has it)
Imposter syndrome is the pervasive idea that we’re not actually good enough, people think we are better than we are, and at any moment we’re going to get found out and disappoint everyone.
Beyond the workplace
Imposter syndrome is most associated with professionals. It can range from a medical professional who feels like they’ve been projecting an image of confidence too much, to a writer or musician who is sure that their next piece will never live up to the acclaim of previous pieces and everyone will suddenly realize they don’t know what they’re doing, to a middle-manager who feels like nobody above or below them realizes how little they know how to do.
But! Less talked-about (but no less prevalent) is imposter syndrome in other areas of life. New parents tend to feel this strongly, as can the “elders” of a family that everyone looks to for advice and strength and support. Perhaps worst is when the person most responsible for the finances of a household feels like everyone just trusts them to keep everything running smoothly, and maybe they shouldn’t because it could all come crashing down at any moment and everyone will see them for the hopeless shambles of a human being that they really are.
Feelings are not facts
And yet (while everyone makes mistakes sometimes) the reality is that we’re all doing our best. Given that imposter syndrome affects up to 82% of people, let’s remember to have some perspective. Everyone feels like they’re winging it sometimes. Everyone feels the pressure.
Well, perhaps not everyone. There’s that other 18%. Some people are sure they’re the best thing ever. Then again, there’s probably some in that 18% that actually feel worse than the 82%—they just couldn’t admit it, even in an anonymized study.
But one thing’s for sure: it’s very, very common. Especially in high-performing women, by the way, and people of color. In other words, people who typically “have to do twice as much to get recognized as half as good”.
That said, the flipside of this is that people who are not in any of those categories may feel “everything is in my favor, so I really have no excuse to not achieve the most”, and can sometimes take very extreme actions to try to avoid perceived failure, and it can be their family that pays the price.
Things to remember
If you find imposter syndrome nagging at you, remember these things:
- There are people far less competent than you, doing the same thing
- Nobody knows how to do everything themselves, especially at first
- If you don’t know how to do something, you can usually find out
- There is always someone to ask for help, or at least advice, or at least support
At the end of the day, we evolved to eat fruit and enjoy the sun. None of us are fully equipped for all the challenges of the modern world, but if we do our reasonable best, and look after each other (and that means that you too, dear reader, deserve looking after as well), we can all do ok.
Share This Post
Related Posts
-
Ozempic Helps People Walk Further
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s often a catch-22 when it comes to exercise: it’s important for good health, and/but people with ill health usually cannot exercise much.
A recent (published today, at time of writing, the 29th of March 2025, never let it be said we don’t bring you the very most up-to-date health science!) study by Dr. Neda Rasouli et al. has shown there is a possible way through that catch-22, depending on the nature of the illness.
This study followed 792 people across 112 outpatient clinical trial sites in 20 countries in North America, Asia, and Europe, with type 2 diabetes and peripheral artery disease.
What they found
Patients taking semaglutide (specifically, 1mg Ozempic) enjoyed a 21% median increase in walking distance, as well as some bonus benefits, namely:
- Weight reduction: the semaglutide group saw a greater reduction in body weight (–4.1 kg; P < 0 .0001)
- HbA1c levels: semaglutide lowered HbA1c by 1 percentage point (P < 0.0001)
- Blood pressure: systolic blood pressure decreased by 3.2 mmHg (P = 0.0042)
You may be wondering what that “P =” means: it’s the probability of this occurring by random chance, on a scale from zero (impossible outcome) to 1 (unavoidable outcome).
For example:
“We hypothesized that singing the happy birthday song before tossing a coin would result in it landing on heads. We sang the happy birthday song and tossed the coin; it landed on heads (P = 0.5)”
In science, generally speaking anything with a probability of under 0.05 (expressed as: “P < 0.05”) is considered a statistically significant result.
All this to say, the cited figures of, for example, P < 0.0001, are very significant indeed.
On which note, that 21% median increase in walking distance? P < 0.0004.
As for side effects? Serious adverse events related to the drug occurred in 1% of the semaglutide group vs 2% in the placebo group. So, that seems quite safe indeed.
You can find the paper itself here:
Want to learn more?
Check out:
- The Doctor Who Wants Us To Exercise Less, & Move More
- Walking… Better.
- 5 Ways To Naturally Boost The “Ozempic Effect”
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How we can prepare for future public health emergencies
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The U.S. is experiencing an increasing number of disease outbreaks and extreme weather events. While state and national preparedness for public health emergencies has improved in some areas, dangerous gaps remain, says a recent report from Trust for America’s Health.
Titled, “Ready or Not 2024: Protecting the Public’s Health from Diseases, Disasters, and Bioterrorism,” the report identifies gaps in national and state preparedness for public health emergencies and provides recommendations for improvement.
Using nine key indicators, the report categorizes all U.S. states and the District of Columbia into three readiness levels: high, medium, and low. The writers hope the report will help policymakers in under-performing states improve public health infrastructure.
Read on to learn more about what the research found and how we can individually prepare for future public health emergencies.
There’s work to be done
The report highlights areas with strong performance as well as those that need improvement.
Some areas with strong performance:
- State public health funding: Most states and the District of Columbia either maintained or increased their public health funding during the 2023 fiscal year.
- Health care labor force preparedness: Most states have started expanding the health care labor force for improved emergency response. As of 2023, 39 states participated in the Nurse Licensure Compact, which allows nurses to work in multiple member states without the need for additional state licenses.
Some areas that need improvement:
- Hospital safety scores: Only 25 percent of acute care hospitals earned the highest patient safety grade in fall 2023. These scores measure health care-associated infection rates, intensive care unit capacity, and other metrics. More high-scoring hospitals would improve preparedness for future public health emergencies.
- Access to paid time off: From March 2018 to March 2023, only 55 percent of U.S. workers used paid time off. Access to paid time off is important for reducing the spread of infectious diseases.
We can all do our part by staying up to date on vaccines
While the report focuses on policy changes that would improve emergency preparedness, Trust for America’s Health’s research identifies one way that we can individually prepare for future public health emergencies: staying up to date on vaccines.
The report found that during the 2022-2023 flu season, only 49 percent of those eligible for the flu vaccine received it. Public health experts are concerned that false claims about COVID-19 vaccines have resulted in overall vaccine hesitancy.
A decline in vaccination rates has led to an uptick in life-threatening, vaccine-preventable diseases, such as measles. Increasing vaccine uptake would prevent the spread of vaccine-preventable diseases and reduce strain on hospital systems during public health crises.
Make sure that you and your children have received all recommended vaccines to prevent severe illness, hospitalization, and death. Learn more about recommended vaccines for adults and children from the CDC.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
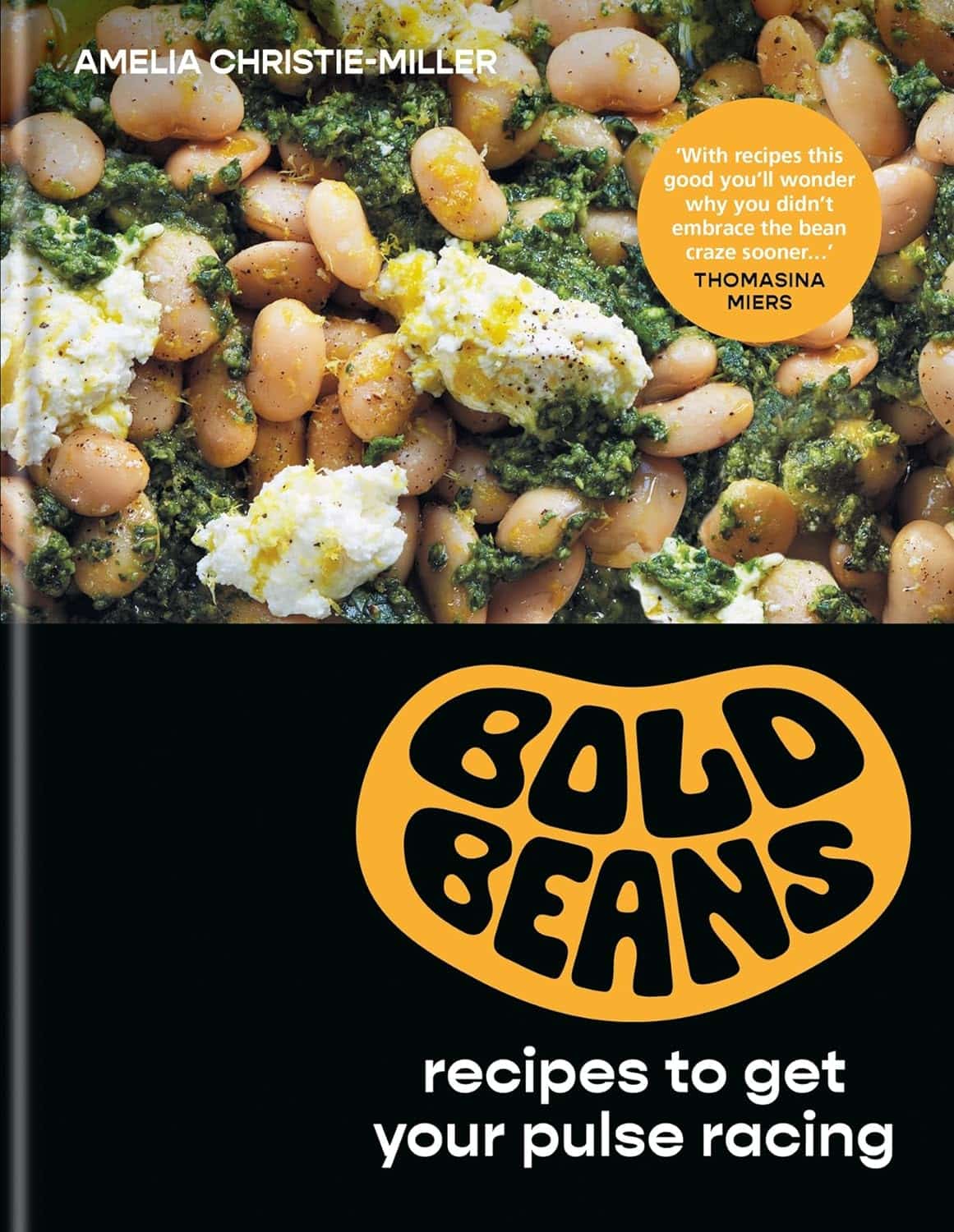
Bold Beans – by Amelia Christie-Miller
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We all know beans are one of the most healthful foods around, but how to include more of them, without getting boring?
This book has the answer, giving 80 exciting recipes, divided into the following sections:
- Speedy beans
- Bean snacks & sharing plates
- Brothy beans
- Bean bowls
- Hearty salads
- Bean feasts
The recipes are obviously all bean-centric, though if you have a particular dietary restriction, watch out for the warning labels on some (e.g. meat, fish, dairy, gluten, etc), and make a substitution if appropriate.
The recipes themselves have a happily short introductory paragraph, followed by all you’d expect from a recipe book (ingredients, measurements, method, picture)
There’s also a reference section, to learn about different kinds of beans and bean-related culinary methods that can be applied per your preferences.
Bottom line: if you’d like to include more beans in your daily diet but are stuck for making them varied and interesting, this is the book for you!
Click here to check out Bold Beans, and get your pulse racing (in a good way!)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: