Morning Routines That Just FLOW
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Morning Routines That Just FLOW
“If the hardest thing you have to do in your day is eat a frog, eat that frog first!”, they say.
And, broadly speaking, it is indeed good to get anything stressful out of the way early, so that we can relax afterwards. But…
- Are we truly best at frog-eating when blurry-eyed and sleepy?
- Is there a spoonful of sugar that could make the medicine go down better?
- What do we need to turn eating the frog into an enjoyable activity?
Flow
“Flow” is a concept brought to public consciousness by psychologist Mihaly Csikszentmihalyi, and it refers to a state in which we feel good about what we’re doing, and just keep doing, at a peak performance level.
Writer’s note: as a writer, for example…
Sometimes I do not want to write, I pace to and fro near my computer, going on side-quests like getting a coffee or gazing out of the window into my garden. But once I get going, suddenly, something magical happens and before I know it, I have to trim my writing down because I’ve written too much. That magical window of effortless productivity was a state of flow.
Good morning!
What is a good morning, to you? Build that into your morning! Set parameters around it so you don’t get carried away timewise and find yourself in the afternoon (unless that would work for you!), but first thing in the morning is the time to light up each part of your brain with appropriate neurotransmitters.
Getting the brain juices flowing
Cortisol
When we wake up, we (unless we have some neurochemical imbalance, such as untreated depression) get a spike of cortisol. Cortisol is much-maligned and feared, and indeed it can be very much deleterious to the health in cases of chronic stress. But a little spike now and again is actually beneficial for us.
Quick Tip: if you want to artificially stimulate (or enhance) a morning cortisol spike, a cold shower is the way to go. Or even just a face-plunge into a bowl of ice-water (put ice in it, give it a couple of minutes to chill the water, then put your face in for a count of 30 seconds, or less if you can’t hold your breath that long).
Serotonin
Serotonin is generally thought of as “the happy chemical”, and it’s stimulated by blue/white light, and also by seeing greenery.
Quick tip: to artificially stimulate (or enhance) a morning serotonin boost, your best friend is sunlight. Even sun through a partly-clouded sky will tend to outperform artificial lighting, including artificial sunlight lighting. Try to get sun between 08:30 and 09:00, if you can. Best of all, do it in your garden or nearby park, as the greenery will be an extra boost!
Dopamine
Generally thought of as “the reward chemical”, but it’s also critical for a lot of kinds of brainwork, including language processing and problem-solving.
Quick Tip: to artificially stimulate* a dopamine surge to get you going, do something that you and/or your body finds rewarding. Examples include:
- Exercise, especially in a vigorous burst
- A good breakfast, a nice coffee, whatever feels right to you
- An app that has motivational bells and whistles, a streak for you to complete, etc
Note: another very enjoyable activity might come to mind that doesn’t even require you getting out of bed. Be aware, however, gentleman-readers specifically, that if you complete that activity, you’ll get a prolactin spike that will wipe out the dopamine you just worked up (because prolactin is antagonistic to dopamine). So that one’s probably better for a lazy morning when you can go back to sleep, than a day when you want to get up and go! Ladies, this is less of a worry for us as the physiology an orgasm driven by estrogen+progesterone rather than testosterone is different; there will not usually be a prolactin spike following the spike of dopamine; our orgasm-related dopamine spike is followed by a wave of oxytocin instead (“the cuddle chemical”), which is much more pleasant than prolactin.
*there’s no “(or enhance)” for this one; you won’t get dopamine from doing nothing, that’s just not how “the reward chemical” works
Flow-building in a stack
When you’ve just woken up and are in a blurry morning haze, that’s not the time to be figuring out “what should I be doing next?”, so instead:
- Work out the things you want to incorporate into your morning routine
- Put them in the order that will be easiest to perform—some things will go a lot better after others!
- Remember to also include things that are simply necessary—morning bathroom ablutions, for example
The goal here is to have a this-and-this-and-this-and-this list of items that you can go through without any deviations, and get in the habit of “after item 1 I automatically do item 2, after which I automatically do item 3, after which…”
Implement this, and your mornings will become practically automated, but in a joyous, life-enhancing way that sets you up in good order for whatever you want/need to do!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Brain-Gut Highway: A Two-Way Street
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
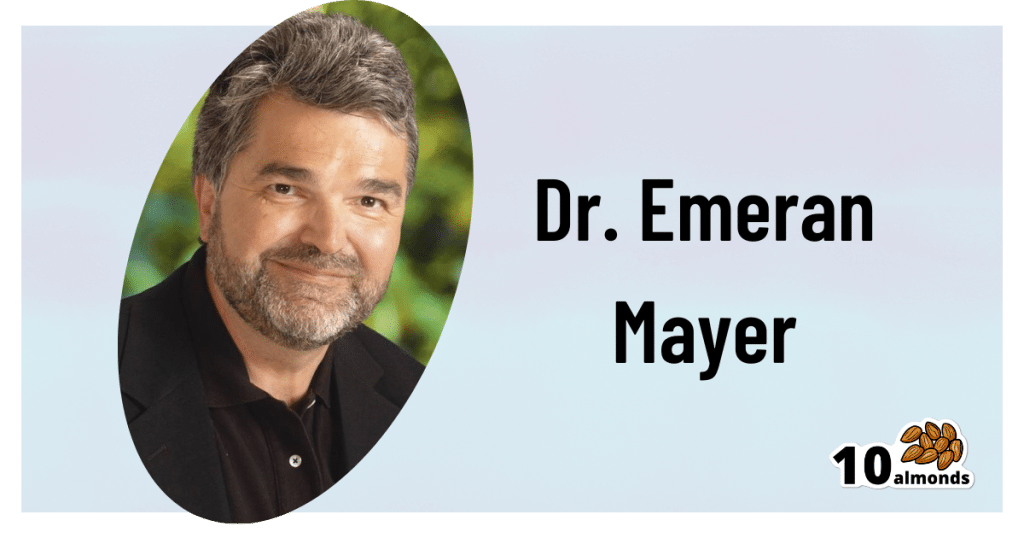
The Brain-Gut Two-Way Highway
This is Dr. Emeran Mayer. He has the rather niche dual specialty of being a gastroenterologist and a neurologist. He has published over 353 peer reviewed scientific articles, and he’s a professor in the Departments of Medicine, Physiology, and Psychiatry at UCLA. Much of his work has been pioneering medical research into gut-brain interactions.
We know the brain and gut are connected. What else does he want us to know?
First, that it is a two-way interaction. It’s about 90% “gut tells the brain things”, but it’s also 10% “brain tells the gut things”, and that 10% can make more like a 20% difference, if for example we look at the swing between “brain using that 10% communication to tell gut to do things worse” or “brain using that 10% communication to tell gut to do things better”, vs the midpoint null hypothesis of “what the gut would be doing with no direction from the brain”.
For example, if we are experiencing unmanaged chronic stress, that is going to tell our gut to do things that had an evolutionary advantage 20,000–200,000 years ago. Those things will not help us now. We do not need cortisol highs and adrenal dumping because we ate a piece of bread while stressed.
Read more (by Dr. Mayer): The Stress That Evolution Has Not Prepared Us For
With this in mind, if we want to look after our gut, then we can start before we even put anything in our mouths. Dr. Mayer recommends managing stress, anxiety, and depression from the head downwards as well as from the gut upwards.
Here’s what we at 10almonds have written previously on how to manage those things:
- No-Frills, Evidence-Based Mindfulness
- How To Set Anxiety Aside
- The Mental Health First-Aid You’ll Hopefully Never Need
Do eat for gut health! Yes, even if…
Unsurprisingly, Dr. Mayer advocates for a gut-friendly, anti-inflammatory diet. We’ve written about these things before:
…but there’s just one problem:
For some people, such as with IBS, Crohn’s, and colitis, the Mediterranean diet that we (10almonds and Dr. Mayer) generally advocate for, is inaccessible. If you (if you have those conditions) eat as we describe, a combination of the fiber in many vegetables and the FODMAPs* in many fruits, will give you a very bad time indeed.
*Fermentable Oligo-, Di-, Monosaccharides And Polyols
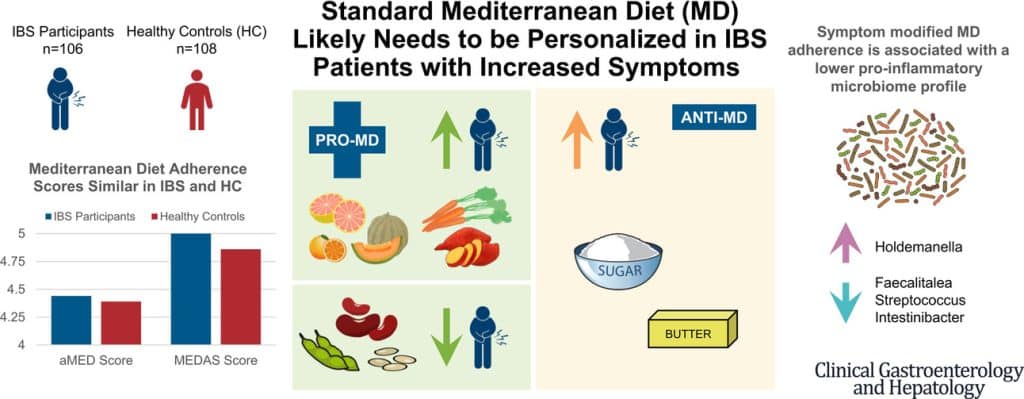
Dr. Mayer has the answer to this riddle, and he’s not just guessing; he and his team did science to it. In a study with hundreds of participants, he measured what happened with adherence (or not) to the Mediterranean diet (or modified Mediterranean diet) (or not), in participants with IBS (or not).
The results and conclusions from that study included:
❝Among IBS participants, a higher consumption of fruits, vegetables, sugar, and butter was associated with a greater severity of IBS symptoms. Multivariate analysis identified several Mediterranean Diet foods to be associated with increased IBS symptoms.
A higher adherence to symptom-modified Mediterranean Diet was associated with a lower abundance of potentially harmful Faecalitalea, Streptococcus, and Intestinibacter, and higher abundance of potentially beneficial Holdemanella from the Firmicutes phylum.
A standard Mediterranean Diet was not associated with IBS symptom severity, although certain Mediterranean Diet foods were associated with increased IBS symptoms. Our study suggests that standard Mediterranean Diet may not be suitable for all patients with IBS and likely needs to be personalized in those with increased symptoms.❞
In graphical form:
And if you’d like to read more about this (along with more details on which specific foods to include or exclude to get these results), you can do so…
- The study itself (full article): The Association Between a Mediterranean Diet and Symptoms of Irritable Bowel Syndrome
- Dr. Mayer’s blog (lay explanation): The Benefits of a Modified Mediterranean Diet for Irritable Bowel Syndrome
Want to know more?
Dr. Mayer offers many resources, including a blog, books, recipes, podcasts, and even a YouTube channel:
Share This Post
-
Coach’s Plan – by Mike Kavanagh
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A sports coach’s job is to prepare a plan, give it to the player(s), and hold them accountable to it. Change the strategy if needs be, call the shots. The job of the player(s) is then to follow those instructions.
If you have trouble keeping yourself accountable, Kavanagh argues that it can be good to separate how you approach things.
Not just “coach yourself”, but put yourself entirely in the coach’s shoes, as though you were a separate person, then switch back, and follow those instructions, trusting in your coach’s guidance.
The book also provides illustrative examples and guides the reader through some potential pitfalls—for example, what happens when morning you doesn’t want to do the things that evening you decided would be best?
The absolute backbone of this method is that it takes away the paralysing self-doubt that can occur when we second-guess ourselves mid-task.
In short, this book will fire up your enthusiasm and give you a reliable fall-back for when your motivation’s flagging.
Share This Post
-
Pain Clinics Made Millions From ‘Unnecessary’ Injections Into ‘Human Pin Cushions’
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
McMINNVILLE, Tenn. — Each month, Michelle Shaw went to a pain clinic to get the shots that made her back feel worse — so she could get the pills that made her back feel better.
Shaw, 56, who has been dependent on opioid painkillers since she injured her back in a fall a decade ago, said in both an interview with KFF Health News and in sworn courtroom testimony that the Tennessee clinic would write the prescriptions only if she first agreed to receive three or four “very painful” injections of another medicine along her spine.
The clinic claimed the injections were steroids that would relieve her pain, Shaw said, but with each shot her agony would grow. Shaw said she eventually tried to decline the shots, then the clinic issued an ultimatum: Take the injections or get her painkillers somewhere else.
“I had nowhere else to go at the time,” Shaw testified, according to a federal court transcript. “I was stuck.”
Shaw was among thousands of patients of Pain MD, a multistate pain management company that was once among the nation’s most prolific users of what it referred to as “tendon origin injections,” which normally inject a single dose of steroids to relieve stiff or painful joints. As many doctors were scaling back their use of prescription painkillers due to the opioid crisis, Pain MD paired opioids with monthly injections into patients’ backs, claiming the shots could ease pain and potentially lessen reliance on painkillers, according to federal court documents.
Now, years later, Pain MD’s injections have been proved in court to be part of a decade-long fraud scheme that made millions by capitalizing on patients’ dependence on opioids. The Department of Justice has successfully argued at trial that Pain MD’s “unnecessary and expensive injections” were largely ineffective because they targeted the wrong body part, contained short-lived numbing medications but no steroids, and appeared to be based on test shots given to cadavers — people who felt neither pain nor relief because they were dead.
Four Pain MD employees have pleaded guilty or been convicted of health care fraud, including company president Michael Kestner, who was found guilty of 13 felonies at an October trial in Nashville, Tennessee. According to a transcript from Kestner’s trial that became public in December, witnesses testified that the company documented giving patients about 700,000 total injections over about eight years and said some patients got as many as 24 shots at once.
“The defendant, Michael Kestner, found out about an injection that could be billed a lot and paid well,” said federal prosecutor James V. Hayes as the trial began, according to the transcript. “And they turned some patients into human pin cushions.”
The Department of Justice declined to comment for this article. Kestner’s attorneys either declined to comment or did not respond to requests for an interview. At trial, Kestner’s attorneys argued that he was a well-intentioned businessman who wanted to run pain clinics that offered more than just pills. He is scheduled to be sentenced on April 21 in a federal court in Nashville.
According to the transcript of Kestner’s trial, Shaw and three other former patients testified that Pain MD’s injections did not ease their pain and sometimes made it worse. The patients said they tolerated the shots only so Pain MD wouldn’t cut off their prescriptions, without which they might have spiraled into withdrawal.
“They told me that if I didn’t take the shots — because I said they didn’t help — I would not get my medication,” testified Patricia McNeil, a former patient in Tennessee, according to the trial transcript. “I took the shots to get my medication.”
In her interview with KFF Health News, Shaw said that often she would arrive at the Pain MD clinic walking with a cane but would leave in a wheelchair because the injections left her in too much pain to walk.
“That was the pain clinic that was supposed to be helping me,” Shaw said in her interview. “I would come home crying. It just felt like they were using me.”
‘Not Actually Injections Into Tendons at All’
Pain MD, which sometimes operated under the name Mid-South Pain Management, ran as many as 20 clinics in Tennessee, Virginia, and North Carolina throughout much of the 2010s. Some clinics averaged more than 12 injections per patient each month, and at least two patients each received more than 500 shots in total, according to federal court documents.
All those injections added up. According to Medicare data filed in federal court, Pain MD and Mid-South Pain Management billed Medicare for more than 290,000 “tendon origin injections” from January 2010 to May 2018, which is about seven times that of any other Medicare biller in the U.S. over the same period.
Tens of thousands of additional injections were billed to Medicaid and Tricare during those same years, according to federal court documents. Pain MD billed these government programs for about $111 per injection and collected more than $5 million from the government for the shots, according to the court documents.
More injections were billed to private insurance too. Christy Wallace, an audit manager for BlueCross BlueShield of Tennessee, testified that Pain MD billed the insurance company about $40 million for more than 380,000 injections from January 2010 to March 2013. BlueCross paid out about $7 million before it cut off Pain MD, Wallace said.
These kinds of enormous billing allegations are not uncommon in health care fraud cases, in which fraudsters sometimes find a legitimate treatment that insurance will pay for and then overuse it to the point of absurdity, said Don Cochran, a former U.S. attorney for the Middle District of Tennessee.
Tennessee alone has seen fraud allegations for unnecessary billing of urine testing, skin creams, and other injections in just the past decade. Federal authorities have also investigated an alleged fraud scheme involving a Tennessee company and hundreds of thousands of catheters billed to Medicare, according to The Washington Post, citing anonymous sources.
Cochran said the Pain MD case felt especially “nefarious” because it used opioids to make patients play along.
“A scheme where you get Medicare or Medicaid money to provide a medically unnecessary treatment is always going to be out there,” Cochran said. “The opioid piece just gives you a universe of compliant people who are not going to question what you are doing.”
“It was only opioids that made those folks come back,” he said.
The allegations against Pain MD became public in 2018 when Cochran and the Department of Justice filed a civil lawsuit against the company, Kestner, and several associated clinics, alleging that Pain MD defrauded taxpayers and government insurance programs by billing for “tendon origin injections” that were “not actually injections into tendons at all.”
Kestner, Pain MD, and several associated clinics have each denied all allegations in that lawsuit, which is ongoing.Scott Kreiner, an expert on spine care and pain medicine who testified at Kestner’s criminal trial, said that true tendon origin injections (or TOIs) typically are used to treat inflamed joints, like the condition known as “tennis elbow,” by injecting steroids or platelet-rich plasma into a tendon. Kreiner said most patients need only one shot at a time, according to the transcript.
But Pain MD made repeated injections into patients’ backs that contained only lidocaine or Marcaine, which are anesthetic medications that cause numbness for mere hours, Kreiner testified. Pain MD also used needles that were often too short to reach back tendons, Kreiner said, and there was no imaging technology used to aim the needle anyway. Kreiner said he didn’t find any injections in Pain MD’s records that appeared medically necessary, and even if they had been, no one could need so many.
“I simply cannot fathom a scenario where the sheer quantity of TOIs that I observed in the patient records would ever be medically necessary,” Kreiner said, according to the trial transcript. “This is not even a close call.”
Jonathan White, a physician assistant who administered injections at Pain MD and trained other employees to do so, then later testified against Kestner as part of a plea deal, said at trial that he believed Pain MD’s injection technique was based on a “cadaveric investigation.”
According to the trial transcript, White said that while working at Pain MD he realized he could find no medical research that supported performing tendon origin injections on patients’ backs instead of their joints. When he asked if Pain MD had any such research, White said, an employee responded with a two-paragraph letter from a Tennessee anatomy professor — not a medical doctor — that said it was possible to reach the region of back tendons in a cadaver by injecting “within two fingerbreadths” of the spine. This process was “exactly the procedure” that was taught at Pain MD, White said.
During his own testimony, Kreiner said it was “potentially dangerous” to inject a patient as described in the letter, which should not have been used to justify medical care.
“This was done on a dead person,” Kreiner said, according to the trial transcript. “So the letter says nothing about how effective the treatment is.”
Over-Injecting ‘Killed My Hand’
Pain MD collapsed into bankruptcy in 2019, leaving some patients unable to get new prescriptions because their medical records were stuck in locked storage units, according to federal court records.
At the time, Pain MD defended the injections and its practice of discharging patients who declined the shots. When a former patient publicly accused the company of treating his back “like a dartboard,” Pain MD filed a defamation lawsuit, then dropped the suit about a month later.
“These are interventional clinics, so that’s what they offer,” Jay Bowen, a then-attorney for Pain MD, told The Tennessean newspaper in 2019. “If you don’t want to consider acupuncture, don’t go to an acupuncture clinic. If you don’t want to buy shoes, don’t go to a shoe store.”
Kestner’s trial told another story. According to the trial transcript, eight former Pain MD medical providers testified that the driving force behind Pain MD’s injections was Kestner himself, who is not a medical professional and yet regularly pressured employees to give more shots.
One nurse practitioner testified that she received emails “every single workday” pushing for more injections. Others said Kestner openly ranked employees by their injection rates, and implied that those who ranked low might be fired.
“He told me that if I had to feed my family based on my productivity, that they would starve,” testified Amanda Fryer, a nurse practitioner who was not charged with any crime.
Brian Richey, a former Pain MD nurse practitioner who at times led the company’s injection rankings, and has since taken a plea deal that required him to testify in court, said at the trial that he “performed so many injections” that his hand became chronically inflamed and required surgery.
“‘Over injecting killed my hand,’” Richey said on the witness stand, reading a text message he sent to another Pain MD employee in 2017, according to the trial transcript. “‘I was in so much pain Injecting people that didnt want it but took it to stay a patient.’”
“Why would they want to stay there?” a prosecutor asked.
“To keep getting their narcotics,” Richey responded, according to the trial transcript.
Throughout the trial, defense attorney Peter Strianse argued that Pain MD’s focus on injections was a result of Kestner’s “obsession” with ensuring that the company “would never be called a pill mill.”
Strianse said that Kestner “stayed up at night worrying” about patients coming to clinics only to get opioid prescriptions, so he pushed his employees to administer injections, too.
“Employers motivating employees is not a crime,” Strianse said at closing arguments, according to the court transcript. “We get pushed every day to perform. It’s not fraud; it’s a fact of life.”
Prosecutors insisted that this defense rang hollow. During the trial, former employees had testified that most patients’ opioid dosages remained steady or increased while at Pain MD, and that the clinics did not taper off the painkillers no matter how many injections were given.
“Giving them injections does not fix the pill mill problem,” federal prosecutor Katherine Payerle said during closing arguments, according to the trial transcript. “The way to fix being a pill mill is to stop giving the drugs or taper the drugs.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
How to Prevent Dementia – by Dr. Richard Restak
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written about this topic here, we know. But there’s a lot more we can do to be on guard against, and pre-emptively strengthen ourselves against, dementia.
The author, a neurologist, takes us on a detailed exploration of dementia in general, with a strong focus on Alzheimer’s in particular, as that accounts for more than half of all dementia cases.
But what if you can’t avoid it? It could be that with the wrong genes and some other factor(s) outside of your control, it will get you if something else doesn’t get you first.
Rather than scaremongering, Dr. Restak tackles this head-on too, and discusses how symptoms can be managed, to make the illness less anxiety-inducing, and look to maintain quality of life as much as possible.
The style of the book is… it reads a lot like an essay compilation. Good essays, then organized and arranged in a sensible order for reading, but distinct self-contained pieces. There are ten or eleven chapters (depending on how we count them), each divided into few or many sections. All this makes for:
- A very “read a bit now and a bit later and a bit the next day” book, if you like
- A feeling of a very quick pace, if you prefer to sit down and read it in one go
Either way, it’s a very informative read.
Bottom line: if you’d like to better understand the many-headed beast that is dementia, this book gives a far more comprehensive overview than we could here, and also explains the prophylactic interventions available.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Managing Your Mortality
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Planning Is a Matter of Life and Death
Barring medical marvels as yet unrevealed, we are all going to die. We try to keep ourselves and our loved ones in good health, but it’s important to be prepared for the eventuality of death.
While this is not a cheerful topic, considering these things in advance can help us manage a very difficult thing, when the time comes.
We’ve put this under “Psychology Sunday” as it pertains to processing our own mortality, and managing our own experiences and the subsequent grief that our death may invoke in our loved ones.
We’ll also be looking at some of the medical considerations around end-of-life care, though.
Organizational considerations
It’s generally considered good to make preparations in advance. Write (or update) a Will, tie up any loose ends, decide on funerary preferences, perhaps even make arrangements with pre-funding. Life insurance, something difficult to get at a good rate towards the likely end of one’s life, is better sorted out sooner rather than later, too.
Beyond bureaucracy
What’s important to you, to have done before you die? It could be a bucket list, or it could just be to finish writing that book. It could be to heal a family rift, or to tell someone how you feel.
It could be more general, less concrete: perhaps to spend more time with your family, or to engage more with a spiritual practice that’s important to you.
Perhaps you want to do what you can to offset the grief of those you’ll leave behind; to make sure there are happy memories, or to make any requests of how they might remember you.
Lest this latter seem selfish: after a loved one dies, those who are left behind are often given to wonder: what would they have wanted? If you tell them now, they’ll know, and can be comforted and reassured by that.
This could range from “bright colors at my funeral, please” to “you have my blessing to remarry if you want to” to “I will now tell you the secret recipe for my famous bouillabaisse, for you to pass down in turn”.
End-of-life care
Increasingly few people die at home.
- Sometimes it will be a matter of fighting tooth-and-nail to beat a said-to-be-terminal illness, and thus expiring in hospital after a long battle.
- Sometimes it will be a matter of gradually winding down in a nursing home, receiving medical support to the end.
- Sometimes, on the other hand, people will prefer to return home, and do so.
Whatever your preferences, planning for them in advance is sensible—especially as money may be a factor later.
Not to go too much back to bureaucracy, but you might also want to consider a Living Will, to be enacted in the case that cognitive decline means you cannot advocate for yourself later.
Laws vary from place to place, so you’ll want to discuss this with a lawyer, but to give an idea of the kinds of things to consider:
National Institute on Aging: Preparing A Living Will
Palliative care
Palliative care is a subcategory of end-of-life care, and is what occurs when no further attempts are made to extend life, and instead, the only remaining goal is to reduce suffering.
In the case of some diseases including cancer, this may mean coming off treatments that have unpleasant side-effects, and retaining—or commencing—pain-relief treatments that may, as a side-effect, shorten life.
Euthanasia
Legality of euthanasia varies from place to place, and in some times and places, palliative care itself has been considered a form of “passive euthanasia”, that is to say, not taking an active step to end life, but abstaining from a treatment that prolongs it.
Clearer forms of passive euthanasia include stopping taking a medication without which one categorically will die, or turning off a life support machine.
Active euthanasia, taking a positive action to end life, is legal in some places and the means varies, but an overdose of barbiturates is an example; one goes to sleep and does not wake up.
It’s not the only method, though; options include benzodiazepines, and opioids, amongst others:
Efficacy and safety of drugs used for assisted dying
Unspoken euthanasia
An important thing to be aware of (whatever your views on euthanasia) is the principle of double-effect… And how it comes to play in palliative care more often than most people think.
Say a person is dying of cancer. They opt for palliative care; they desist in any further cancer treatments, and take medication for the pain. Morphine is common. Morphine also shortens life.
It’s common for such a patient to have a degree of control over their own medication, however, after a certain point, they will no longer be in sufficient condition to do so.
After this point, it is very common for caregivers (be they medical professionals or family members) to give more morphine—for the purpose of reducing suffering, of course, not to kill them.
In practical terms, this often means that the patient will die quite promptly afterwards. This is one of the reasons why, after sometimes a long-drawn-out period of “this person is dying”, healthcare workers can be very accurate about “it’s going to be in the next couple of days”.
The take-away from this section is: if you would like for this to not happen to you or your loved one, you need to be aware of this practice in advance, because while it’s not the kind of thing that tends to make its way into written hospital/hospice policies, it is very widespread and normalized in the industry on a human level.
Further reading: Goods, causes and intentions: problems with applying the doctrine of double effect to palliative sedation
One last thing…
Planning around our own mortality is never a task that seems pressing, until it’s too late. We recommend doing it anyway, without putting it off, because we can never know what’s around the corner.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hazelnuts vs Chestnuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing hazelnuts to chestnuts, we picked the hazelnuts.
Why?
This one’s not close.
In terms of macros, we have some big difference to start with, since chestnuts contain a lot more water and carbs whereas hazelnuts contain a lot more protein, fats, and fiber. The fats, as with most nuts, are healthy; in this case mostly being monounsaturated fat.
Because of the carbs and fiber being so polarized (i.e., chestnuts have most of the carbs and hazelnuts have most of the fiber), there’s a big difference in glycemic index; hazelnuts have a GI of 15 while chestnuts have a GI of 52.
In the category of vitamins, hazelnuts contain more of vitamins A, B1, B2, B3, B5, B6, and B9, while chestnuts contain more vitamin C.
When it comes to minerals, the story is similar: hazelnuts contain a lot more calcium, copper, iron, magnesium, manganese, phosphorus, and zinc, while chestnuts contain a tiny bit more potassium.
All in all, enjoy either or both, but nutritionally speaking, hazelnuts are a lot better in almost every way.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: