Psychology Sunday: Family Estrangement & How To Fix It
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Estrangement, And How To Heal It
We’ve written before about how deleterious to the health loneliness and isolation can be, and what things can be done about it. Today, we’re tackling a related but different topic.
We recently had a request to write about…
❝Reconciliation of relationships in particular estrangement mother adult daughter❞
And, this is not only an interesting topic, but a very specific one that affects more people than is commonly realized!
In fact, a recent 800-person study found that more than 43% of people experienced family estrangement of one sort or another, and a more specific study of more than 2,000 mother-child pairs found that more than 11% of mothers were estranged from at least one adult child.
So, if you think of the ten or so houses nearest to you, probably at least one of them contains a parent estranged from at least one adult child. Maybe it’s yours. Either way, we hope this article will give you some pause for thought.
Which way around?
It makes a difference to the usefulness of this article whether any given reader experiencing estrangement is the parent or the adult child. We’re going to assume the reader is the parent. It also makes a difference who did the estranging. That’s usually the adult child.
So, we’re broadly going to write with that expectation.
Why does it happen?
When our kids are small, we as parents hold all the cards. It may not always feel that way, but we do. We control our kids’ environment, we influence their learning, we buy the food they eat and the clothes they wear. If they want to go somewhere, we probably have to take them. We can even set and enforce rules on a whim.
As they grow, so too does their independence, and it can be difficult for us as parents to relinquish control, but we’re going to have to at some point. Assuming we are good parents, we just hope we’ve prepared them well enough for the world.
Once they’ve flown the nest and are living their own adult lives, there’s an element of inversion. They used to be dependent on us; now, not only do they not need us (this is a feature not a bug! If we have been good parents, they will be strong without us, and in all likelihood one day, they’re going to have to be), but also…
We’re more likely to need them, now. Not just in the “oh if we have kids they can look after us when we’re old” sense, but in that their social lives are growing as ours are often shrinking, their family growing, while ours, well, it’s the same family but they’re the gatekeepers to that now.
If we have a good relationship, this goes fine. However, it might only take one big argument, one big transgression, or one “final straw”, when the adult child decides the parent is more trouble than they’re worth.
And, obviously, that’s going to hurt. But it’s pretty much how it pans out, according to studies:
Here be science: Tensions in the Parent and Adult Child Relationship: Links to Solidarity and Ambivalence
How to fix it, step one
First, figure out what went wrong.
Resist any urge to protect your own feelings with a defensive knee-jerk “I don’t know; I was a good, loving parent”. That’s a very natural and reasonable urge and you’re quite possibly correct, but it won’t help you here.
Something pushed them away. And, it will almost certainly have been a push factor from you, not a pull factor from whoever is in their life now. It’s easy to put the blame externally, but that won’t fix anything.
And, be honest with yourself; this isn’t a job interview where we have to present a strength dressed up as a “greatest weakness” for show.
You can start there, though! If you think “I was too loving”, then ok, how did you show that love? Could it have felt stifling to them? Controlling? Were you critical of their decisions?
It doesn’t matter who was right or wrong, or even whether or not their response was reasonable. It matters that you know what pushed them away.
How to fix it, step two
Take responsibility, and apologize. We’re going to assume that your estrangement is such that you can, at least, still get a letter to them, for example. Resist the urge to argue your case.
Here’s a very good format for an apology; please consider using this template:
The 10-step (!) apology that’s so good, you’ll want to make a note of it
You may have to do some soul-searching to find how you will avoid making the same mistake in the future, that you did in the past.
If you feel it’s something you “can’t change”, then you must decide what is more important to you. Only you can make that choice, but you cannot expect them to meet you halfway. They already made their choice. In the category of negotiation, they hold all the cards now.
How to fix it, step three
Now, just wait.
Maybe they will reply, forgiving you. If they do, celebrate!
Just be aware that once you reconnect is not the time to now get around to arguing your case from before. It will never be the time to get around to arguing your case from before. Let it go.
Nor should you try to exact any sort of apology from them for estranging you, or they will at best feel resentful, wonder if they made a mistake in reconnecting, and withdraw.
Instead, just enjoy what you have. Many people don’t get that.
If they reply with anger, maybe it will be a chance to reopen a dialogue. If so, family therapy could be an approach useful for all concerned, if they are willing. Chances are, you all have things that you’d all benefit from talking about in a calm, professional, moderated, neutral environment.
You might also benefit from a book we reviewed previously, “Parent Effectiveness Training”. This may seem like “shutting the stable door after the horse has bolted”, but in fact it’s a very good guide to relationship dynamics in general, and extensively covers relations between parents and adult children.
If they don’t reply, then, you did your part. Take solace in knowing that much.
Some final thoughts:
At the end of the day, as parents, our kids living well is (hopefully) testament to that we prepared them well for life, and sometimes, being a parent is a thankless task.
But, we (hopefully) didn’t become parents for the plaudits, after all.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eat to Beat Disease – by Dr. William Li
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. William Li asks the important question: is your diet feeding disease, or defeating it?
Because everything we put in our bodies makes our health just a little better—or just a little worse. Ok, sometimes a lot worse.
But for most people, when it comes to diet, it’s a death of a thousand cuts of unhealthy food. And that’s what he looks to fix with this book.
The good news: Dr. Li (while not advocating for unhealthy eating, of course), focuses less on what to restrict, and more on what to include. This book covers hundreds of such healthy foods, and ideas (practical, useful ones!) on incorporating them daily, including dozens of recipes.
He mainly looks at five ways our food can help us with…
- Angiogenesis (blood vessel replacement)
- Regeneration (of various bodily organs and systems)
- Microbiome health (and all of its knock-on effects)
- DNA protection (and thus slower cellular aging)
- Immunity (defending the body while also reducing autoimmune problems)
The style is simple and explanatory; Dr. Li is a great educator. Reading this isn’t a difficult read, but you’ll come out of it feeling like you just did a short course in health science.
Bottom line: if you’d like an easy way to improve your health in an ongoing and sustainable way, then this book can help you do just that.
Click here to check out Eat To Beat Disease, and eat to beat disease!
Share This Post
-
What you need to know about menopause
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Menopause describes the time when a person with ovaries has gone one full year without a menstrual period. Reaching this phase is a natural aging process that marks the end of reproductive years.
Read on to learn more about the causes, stages, signs, and management of menopause.
What causes menopause?
As you age, your ovaries begin making less estrogen and progesterone—two of the hormones involved in menstruation—and your fertility declines, causing menopause.
Most people begin perimenopause, the transitional time that ends in menopause, in their late 40s, but it can start earlier. On average, people in the U.S. experience menopause in their early 50s.
Your body may reach early menopause for a variety of reasons, including having an oophorectomy, a surgery that removes the ovaries. In this case, the hormonal changes happen abruptly rather than gradually.
Chemotherapy and radiation therapy for cancer patients may also induce menopause, as these treatments may impact ovary function.
What are the stages of menopause?
There are three stages:
- Perimenopause typically occurs eight to 10 years before menopause happens. During this stage, estrogen production begins to decline and ovaries release eggs less frequently.
- Menopause marks the point when you have gone 12 consecutive months without a menstrual period. This means the ovaries have stopped releasing eggs and producing estrogen.
- Postmenopause describes the time after menopause. Once your body reaches this phase, it remains there for the rest of your life.
How do the stages of menopause affect fertility?
Your ovaries still produce eggs during perimenopause, so it is still possible to get pregnant during that stage. If you do not wish to become pregnant, continue using your preferred form of birth control throughout perimenopause.
Once you’ve reached menopause, you can no longer get pregnant naturally. People who would like to become pregnant after that may pursue in vitro fertilization (IVF) using eggs that were frozen earlier in life or donor eggs.
What are the signs of menopause?
Hormonal shifts result in a number of bodily changes. Signs you are approaching menopause may include:
- Hot flashes (a sudden feeling of warmth).
- Irregular menstrual periods, or unusually heavy or light menstrual periods.
- Night sweats and/or cold flashes.
- Insomnia.
- Slowed metabolism.
- Irritability, mood swings, and depression.
- Vaginal dryness.
- Changes in libido.
- Dry skin, eyes, and/or mouth.
- Worsening of premenstrual syndrome (PMS).
- Urinary urgency (a sudden need to urinate).
- Brain fog.
How can I manage the effects of menopause?
You may not need any treatment to manage the effects of menopause. However, if the effects are disrupting your life, your doctor may prescribe hormone therapy.
If you have had a hysterectomy, your doctor may prescribe estrogen therapy (ET), which may be administered via a pill, patch, cream, spray, or vaginal ring. If you still have a uterus, your doctor may prescribe estrogen progesterone/progestin hormone therapy (EPT), which is sometimes called “combination therapy.”
Both of these therapies work by replacing the hormones your body has stopped making, which can reduce the physical and mental effects of menopause.
Other treatment options may include antidepressants, which can help manage mood swings and hot flashes; prescription creams to alleviate vaginal dryness; or gabapentin, an anti-seizure medication that has been shown to reduce hot flashes.
Lifestyle changes may help alleviate the effects on their own or in combination with prescription medication. Those changes include:
- Incorporating movement into your daily life.
- Limiting caffeine and alcohol.
- Quitting smoking.
- Maintaining a regular sleep schedule.
- Practicing relaxation techniques, such as meditation.
- Consuming foods rich in plant estrogens, such as grains, beans, fruits, vegetables, and seeds.
- Seeking support from a therapist and from loved ones.
What health risks are associated with menopause?
Having lower levels of estrogen may put you at greater risk of certain health complications, including osteoporosis and coronary artery disease.
Osteoporosis occurs when bones lose their density, increasing the risk of fractures. A 2022 study found that the prevalence of osteoporotic fractures in postmenopausal women was 82.2 percent.
Coronary artery disease occurs when the arteries that send blood to your heart become narrow or blocked with fatty plaque.
Estrogen therapy can reduce your risk of osteoporosis and coronary artery disease by preserving bone mass and maintaining cardiovascular function.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
-
Aspirin, CVD Risk, & Potential Counter-Risks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aspirin Pros & Cons
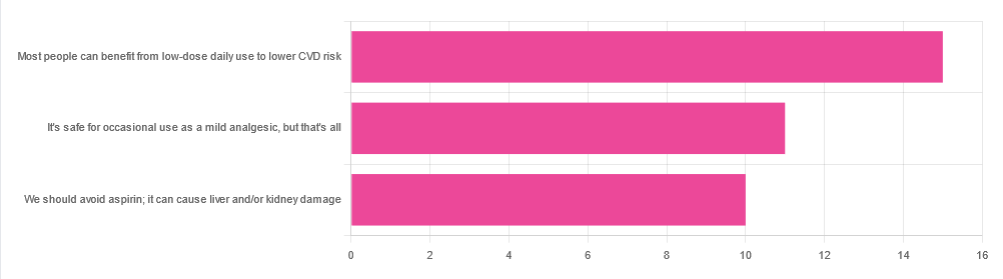
In Tuesday’s newsletter, we asked your health-related opinion of aspirin, and got the above-depicted, below-described set of responses:
- About 42% said “Most people can benefit from low-dose daily use to lower CVD risk”
- About 31% said “It’s safe for occasional use as a mild analgesic, but that’s all”
- About 28% said “We should avoid aspirin; it can cause liver and/or kidney damage”
So, what does the science say?
Most people can benefit from low-dose daily aspirin use to lower the risk of cardiovascular disease: True or False?
True or False depending on what we mean by “benefit from”. You see, it works by inhibiting platelet function, which means it simultaneously:
- decreases the risk of atherothrombosis
- increases the risk of bleeding, especially in the gastrointestinal tract
When it comes to balancing these things and deciding whether the benefit merits the risk, you might be asking yourself: “which am I most likely to die from?” and the answer is: neither
While aspirin is associated with a significant improvement in cardiovascular disease outcomes in total, it is not significantly associated with reductions in cardiovascular disease mortality or all-cause mortality.
In other words: speaking in statistical generalizations of course, it may improve your recovery from minor cardiac events but is unlikely to help against fatal ones
The current prevailing professional (amongst cardiologists) consensus is that it may be recommended for secondary prevention of ASCVD (i.e. if you have a history of CVD), but not for primary prevention (i.e. if you have no history of CVD). Note: this means personal history, not family history.
In the words of the Journal of the American College of Cardiology:
❝Low-dose aspirin (75-100 mg orally daily) might be considered for the primary prevention of ASCVD among select adults 40 to 70 years of age who are at higher ASCVD risk but not at increased bleeding risk (S4.6-1–S4.6-8).
Low-dose aspirin (75-100 mg orally daily) should not be administered on a routine basis for the primary prevention of ASCVD among adults >70 years of age (S4.6-9).
Low-dose aspirin (75-100 mg orally daily) should not be administered for the primary prevention of ASCVD among adults of any age who are at increased risk of bleeding (S4.6-10).❞
~ Dr. Donna Arnett et al. (those section references are where you can find this information in the document)
Read in full: Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology
Or if you’d prefer a more pop-science presentation:
Many older adults still use aspirin for CVD prevention, contrary to clinical guidance
Aspirin can cause liver and/or kidney damage: True or False?
True, but that doesn’t mean we must necessarily abstain, so much as exercise caution.
Aspirin is (at recommended doses) not usually hepatotoxic (toxic to the liver), but there is a strong association between aspirin use in children and the development of Reye’s syndrome, a disease involving encephalopathy and a fatty liver. For this reason, most places have an official recommendation that aspirin not be used by children (cut-off age varies from place to place, for example 12 in the US and 16 in the UK, but the key idea is: it’s potentially dangerous for those who are not fully grown).
Aspirin is well-established as nephrotoxic (toxic to the kidneys), however, the toxicity is sufficiently low that this is not expected to be a problem to otherwise healthy adults taking it at no more than the recommended dose.
For numbers, symptoms, and treatment, see this very clear and helpful resource:
An evidence based flowchart to guide the management of acute salicylate (aspirin) overdose
Take care!
Share This Post
Related Posts
-
Avocado vs Olives – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing avocado to olives, we picked the avocado.
Why?
Both are certainly great! And when it comes to their respective oils, olive oil wins out as it retains many micronutrients that avocado oil loses. But, in their whole form, avocado beats olive:
In terms of macros, avocado has more protein, carbs, fiber, and (healthy) fats. Simply, it’s more nationally-dense than the already nutritionally-dense food that is olives.
When it comes to vitamins, olives are great but avocados really shine; avocado has more of vitamins B1, B2, B3, B5, B6, B7 B9, C, E, K, and choline, while olives boast only more vitamin A.
In the category of minerals, things are closer to even; avocado has more magnesium, manganese, phosphorus, potassium, and zinc, while olives have a lot more calcium, copper, iron, and selenium. Still, a marginal victory for avocado here.
In short, this is another case of one very healthy food looking bad by standing next to an even better one, so by all means enjoy both—if you’re going to pick one though, avocado is the more nutritionally dense.
Want to learn more?
You might like to read:
Avocado Oil vs Olive Oil – Which is Healthier? ← when made into oils, olive oil wins, but avocado oil is still a good option too
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A person in Texas caught bird flu after mixing with dairy cattle. Should we be worried?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The United States’ Centers for Disease Control and Prevention (CDC) has issued a health alert after the first case of H5N1 avian influenza, or bird flu, seemingly spread from a cow to a human.
A farm worker in Texas contracted the virus amid an outbreak in dairy cattle. This is the second human case in the US; a poultry worker tested positive in Colorado in 2022.
The virus strain identified in the Texan farm worker is not readily transmissible between humans and therefore not a pandemic threat. But it’s a significant development nonetheless.
Some background on bird flu
There are two types of avian influenza: highly pathogenic or low pathogenic, based on the level of disease the strain causes in birds. H5N1 is a highly pathogenic avian influenza.
H5N1 first emerged in 1997 in Hong Kong and then China in 2003, spreading through wild bird migration and poultry trading. It has caused periodic epidemics in poultry farms, with occasional human cases.
Influenza A viruses such as H5N1 are further divided into variants, called clades. The unique variant causing the current epidemic is H5N1 clade 2.3.4.4b, which emerged in late 2020 and is now widespread globally, especially in the Americas.
In the past, outbreaks could be controlled by culling of infected birds, and H5N1 would die down for a while. But this has become increasingly difficult due to escalating outbreaks since 2021.
Wild animals are now in the mix
Waterfowl (ducks, swans and geese) are the main global spreaders of avian flu, as they migrate across the world via specific routes that bypass Australia. The main hub for waterfowl to migrate around the world is Quinghai lake in China.
But there’s been an increasing number of infected non-waterfowl birds, such as true thrushes and raptors, which use different flyways. Worryingly, the infection has spread to Antarctica too, which means Australia is now at risk from different bird species which fly here.
H5N1 has escalated in an unprecedented fashion since 2021, and an increasing number of mammals including sea lions, goats, red foxes, coyotes, even domestic dogs and cats have become infected around the world.
Wild animals like red foxes which live in peri-urban areas are a possible new route of spread to farms, domestic pets and humans.
Dairy cows and goats have now become infected with H5N1 in at least 17 farms across seven US states.
What are the symptoms?
Globally, there have been 14 cases of H5N1 clade 2.3.4.4b virus in humans, and 889 H5N1 human cases overall since 2003.
Previous human cases have presented with a severe respiratory illness, but H5N1 2.3.4.4b is causing illness affecting other organs too, like the brain, eyes and liver.
For example, more recent cases have developed neurological complications including seizures, organ failure and stroke. It’s been estimated that around half of people infected with H5N1 will die.
The case in the Texan farm worker appears to be mild. This person presented with conjunctivitis, which is unusual.
Food safety
Contact with sick poultry is a key risk factor for human infection. Likewise, the farm worker in Texas was likely in close contact with the infected cattle.
The CDC advises pasteurised milk and well cooked eggs are safe. However, handling of infected meat or eggs in the process of cooking, or drinking unpasteurised milk, may pose a risk.
Although there’s no H5N1 in Australian poultry or cattle, hygienic food practices are always a good idea, as raw milk or poorly cooked meat, eggs or poultry can be contaminated with microbes such as salmonella and E Coli.
If it’s not a pandemic, why are we worried?
Scientists have feared avian influenza may cause a pandemic since about 2005. Avian flu viruses don’t easily spread in humans. But if an avian virus mutates to spread in humans, it can cause a pandemic.
One concern is if birds were to infect an animal like a pig, this acts as a genetic mixing vessel. In areas where humans and livestock exist in close proximity, for example farms, markets or even in homes with backyard poultry, the probability of bird and human flu strains mixing and mutating to cause a new pandemic strain is higher.
There are a number of potential pathways to a pandemic caused by influenza. Author provided The cows infected in Texas were tested because farmers noticed they were producing less milk. If beef cattle are similarly affected, it may not be as easily identified, and the economic loss to farmers may be a disincentive to test or report infections.
How can we prevent a pandemic?
For now there is no spread of H5N1 between humans, so there’s no immediate risk of a pandemic.
However, we now have unprecedented and persistent infection with H5N1 clade 2.3.4.4b in farms, wild animals and a wider range of wild birds than ever before, creating more chances for H5N1 to mutate and cause a pandemic.
Unlike the previous epidemiology of avian flu, where hot spots were in Asia, the new hot spots (and likely sites of emergence of a pandemic) are in the Americas, Europe or in Africa.
Pandemics grow exponentially, so early warnings for animal and human outbreaks are crucial. We can monitor infections using surveillance tools such as our EPIWATCH platform.
The earlier epidemics can be detected, the better the chance of stamping them out and rapidly developing vaccines.
Although there is a vaccine for birds, it has been largely avoided until recently because it’s only partially effective and can mask outbreaks. But it’s no longer feasible to control an outbreak by culling infected birds, so some countries like France began vaccinating poultry in 2023.
For humans, seasonal flu vaccines may provide a small amount of cross-protection, but for the best protection, vaccines need to be matched exactly to the pandemic strain, and this takes time. The 2009 flu pandemic started in May in Australia, but the vaccines were available in September, after the pandemic peak.
To reduce the risk of a pandemic, we must identify how H5N1 is spreading to so many mammalian species, what new wild bird pathways pose a risk, and monitor for early signs of outbreaks and illness in animals, birds and humans. Economic compensation for farmers is also crucial to ensure we detect all outbreaks and avoid compromising the food supply.
C Raina MacIntyre, Professor of Global Biosecurity, NHMRC L3 Research Fellow, Head, Biosecurity Program, Kirby Institute, UNSW Sydney; Ashley Quigley, Senior Research Associate, Global Biosecurity, UNSW Sydney; Haley Stone, PhD Candidate, Biosecurity Program, Kirby Institute, UNSW Sydney; Matthew Scotch, Associate Dean of Research and Professor of Biomedical Informatics, College of Health Solutions, Arizona State University, and Rebecca Dawson, Research Associate, The Kirby Institute, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Brazil Nuts vs Pecans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Brazil nuts to pecans, we picked the pecans.
Why?
In terms of macros, Brazil nuts have more protein while pecans have more fiber. Both of these nuts are equally fatty, though Brazil nuts have much more saturated fat per 100g, which still isn’t terrible, but it does make pecans’ profile (mostly monounsaturated with some polyunsaturated) the healthier. They’re about equal in carbs. All in all, a win for pecans here.
In the category of vitamins, Brazil nuts have more vitamin E, while pecans have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, K, and choline. An easy win for pecans.
The category of minerals is an interesting one. Brazil nuts have more calcium, copper, magnesium, phosphorus, potassium, and selenium, while pecans have more iron, manganese, and zinc. Before we crown Brazil nuts with the win in this category, though, let’s take a closer look at those selenium levels:
- A cup of cashews contains 21% of the RDA of selenium. Your hair will be luscious and shiny.
- A cup of Brazil nuts contains 10,456% of the RDA of selenium. This is way past the point of selenium toxicity, and your (luscious, shiny) hair will fall out.
For this reason, it’s recommended to eat no more than 3–4 Brazil nuts per day.
We consider that a point against Brazil nuts.
Adding up the sections makes for an overall win for pecans; of course, enjoy either or both, just be sure to practise moderation when it comes to the Brazil nuts!
Want to learn more?
You might like:
Why You Should Diversify Your Nuts
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: