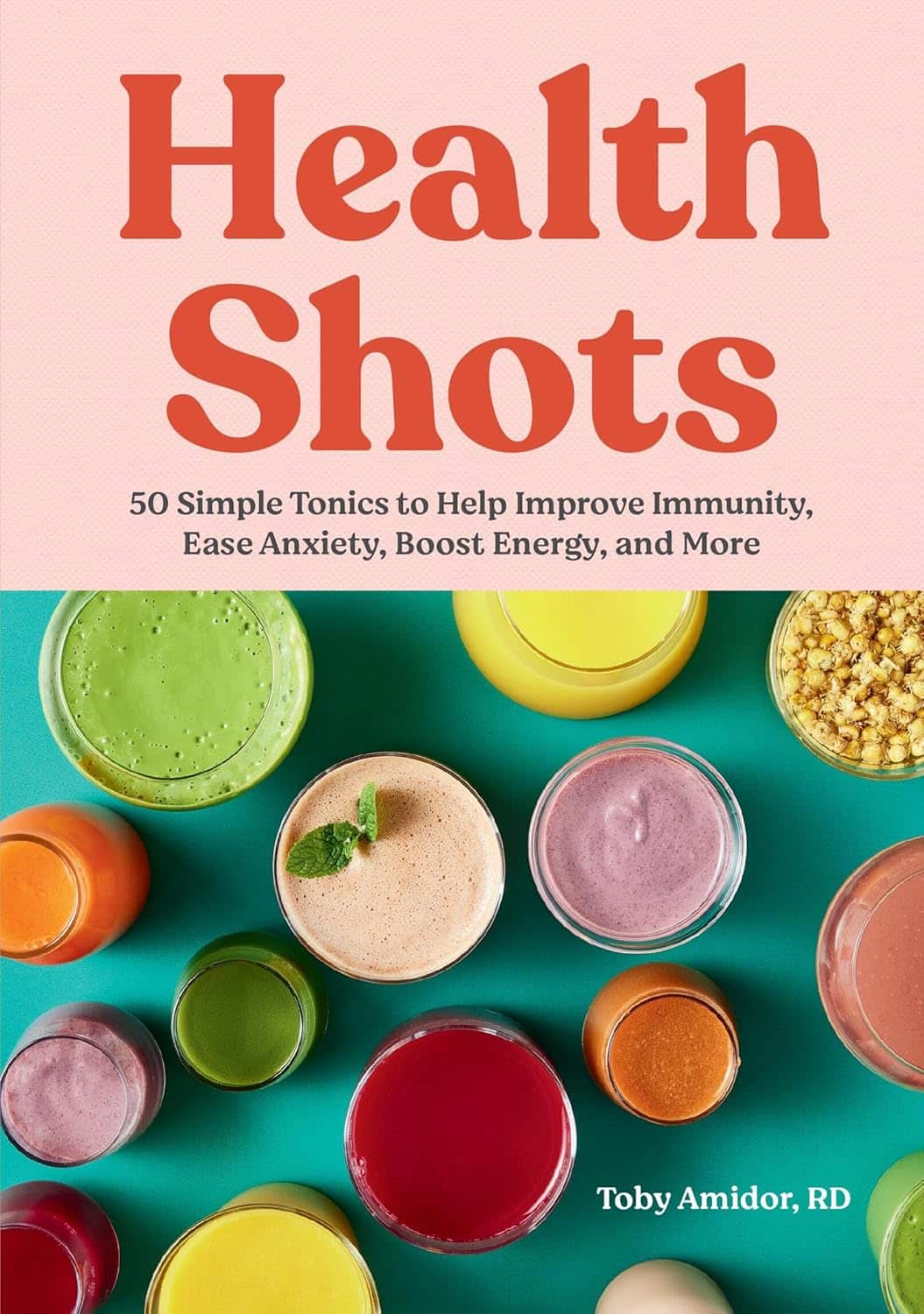
Health Shots − by Toby Amidor
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First a quick note on qualifications: while not a doctor, she’s a RD, CDN, FAND, and as such, this is a very nutrition-focused book.
As a general rule of thumb, juices are unhealthy because of being largely liquid sugar and no fiber, but in this case:
- even the juice-based tonics are very small portions, so even if some have a high glycemic index, they’ll still have a low glycemic load, which means that having one is unlikely to spike blood glucose and thus insulin
- many of the tonics have fiber in any case, due to how they are made.
The tonics are divided into sections per what one wants to focus on, e.g. anti-inflammatory, brain health, sleep, gut health, skin/nails/hair, etc.
That said, some of the recipes are a little optimistic about how much effect the dosage present will have. For example, we calculate an an average of 0.03mg of resveratrol in her grape-based shot boasting resveratrol benefits. For contrast, resveratrol supplements range from 500mg to 200mg. So, to get the equivalent of the least generous supplement, you’d need to drink 16,667 shots.
Bottom line: some of the the health claims in this book are overstated, but by and large, it’s hard to go wrong consuming more plants, and these “health shots” are not a bad way to get a good dose of phytonutrients without hitting glycemic problems.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
‘Tis To Season To Be SAD-Savvy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Seasonal Affective Disorder & SAD Lamps
For those of us in the Northern Hemisphere, it’s that time of the year; especially after the clocks recently went back and the nights themselves are getting longer. So, what to do in the season of 3pm darkness?
First: the problem
The problem is twofold:
- Our circadian rhythm gets confused
- We don’t make enough serotonin
The latter is because serotonin production is largely regulated by sunlight.
People tend to focus on item 2, but item 1 is important too—both as problem, and as means of remedy.
Circadian rhythm is about more than just light
We did a main feature on this a little while back, talking about:
- What light/dark does for us, and how it’s important, but not completely necessary
- How our body knows what time it is even in perpetual darkness
- The many peaks and troughs of many physiological functions over the course of a day/night
- What that means for us in terms of such things as diet and exercise
- Practical take-aways from the above
Read: The Circadian Rhythm: Far More Than Most People Know
With that in mind, the same methodology can be applied as part of treating Seasonal Affective Disorder.
Serotonin is also about more than just light
Our brain is a) an unbelievably powerful organ, and the greatest of any animal on the planet b) a wobbly wet mass that gets easily confused.
In the case of serotonin, we can have problems:
- knowing when to synthesize it or not
- synthesizing it
- using it
- knowing when to scrub it or not
- scrubbing it
- etc
Selective Serotonin Re-uptake Inhibitors (SSRIs) are a class of antidepressants that, as the name suggests, inhibit the re-uptake (scrubbing) of serotonin. So, they won’t add more serotonin to your brain, but they’ll cause your brain to get more mileage out of the serotonin that’s there, using it for longer.
So, whether or not they help will depend on you and your brain:
Read: Antidepressants: Personalization Is Key!
How useful are artificial sunlight lamps?
Artificial sunlight lamps (also called SAD lamps), or blue light lamps, are used in an effort to “replace” daylight.
Does it work? According to the science, generally yes, though everyone would like more and better studies:
- The Efficacy of Light Therapy in the Treatment of Seasonal Affective Disorder: A Meta-Analysis of Randomized Controlled Trials
- Blue-Light Therapy for Seasonal and Non-Seasonal Depression: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Interestingly, it does still work in cases of visual impairment and blindness:
How much artificial sunlight is needed?
According to Wirz-Justice and Terman (2022), the best parameters are:
- 10,000 lux
- full spectrum (white light)
- 30–60 minutes exposure
- in the morning
Source: Light Therapy: Why, What, for Whom, How, and When (And a Postscript about Darkness)
That one’s a fascinating read, by the way, if you have time.
Can you recommend one?
For your convenience, here’s an example product on Amazon that meets the above specifications, and is also very similar to the one this writer has
Enjoy!
Share This Post
-
Cabbage vs Carrots – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cabbage to carrots, we picked the carrots.
Why?
Both are top-tier vegetables! But as the Highlander said, “there can be only one”, and we say carrots get a marginal victory;
In terms of macros, nominally cabbage has slightly more protein (but it’s a tiny amount, and thus an even tinier difference) while carrots have slightly more fiber and carbs (but again, not big differences), as well as the lower glycemic index (but nobody is getting metabolic disease from eating cabbage). We could call this category a tie because it’s all so close, but by the numbers, it’s a slender victory for carrots.
In the category of vitamins, carrots have more of vitamins A, B1, B2, B3, B5, B6, and E, while cabbage has more of vitamins B9, C, K, and choline. Thus, a win for carrots, especially as carrots’ vitamin A is 167x what cabbage has.
When it comes to minerals, cabbage has more calcium, iron, manganese, and selenium, while carrots have more copper, phosphorus, potassium, and zinc. They’re both equal on magnesium, and their respective margins of difference for the other minerals were not big, so this round’s a clear tie.
Adding up the sections makes for an overall win for carrots, but by all means enjoy either or both (together, even, if you like!); diversity is good!
Want to learn more?
You might like:
12 Most Powerful Supplements and Foods to Increase Energy & Slow Down Aging
Enjoy!
Share This Post
-
Capsaicin For Weight Loss And Against Inflammation
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Capsaicin’s Hot Benefits
Capsaicin, the compound in hot peppers that makes them spicy, is a chemical irritant and a neurotoxin. However, humans being humans, we decided to eat them for fun.
In contrast to many other ways in which humans recreationally enjoy things that are objectively poisonous, consuming capsaicin (in moderation) is considered to have health benefits, such as aiding weight loss (by boosting metabolism) and reducing inflammation.
Let’s see what the science says…
First: is it safe?
Capsaicin is classified as “Generally Recognized As Safe”. That said, the same mechanism that causes them to boost metabolism, does increase blood pressure:
Mechanisms underlying the hypertensive response induced by capsaicin
If you are in good cardiovascular health, this increase should be slight and not pose any threat, unless for example you enter a chili-eating contest when not acclimated to such:
Capsaicin and arterial hypertensive crisis
As ever, if unsure, do check with your doctor first, especially if you are taking any blood pressure medications, or otherwise have known blood pressure issues.
Does it really boost metabolism?
It certainly does; it works by increasing oxygen consumption and raising body temperature, both of which mean more calories will be burned for the same amount of work:
Dietary capsaicin and its anti-obesity potency: from mechanism to clinical implications
This means, of course, that chili peppers enjoy the status of being functionally a “negative calorie” food, and a top-tier one at that:
Chili pepper as a body weight-loss food
Here’s a good quality study that showed a statistically significant* fat loss improvement over placebo:
*To put it in numbers, the benefit was:
- 5.91 percentage points lower body fat percentage than placebo
- 6.68 percentage points greater change in body fat mass than placebo
See also: Difference between percentages and percentage points
For those who prefer big reviews than single studies, we’ve got you covered:
Does it really reduce inflammation?
Counterintuitive as it may seem, yes. By means of reducing oxidative stress. Given that things that reduce oxidative stress tend to reduce inflammation, and in turn tend to reduce assorted disease risks (from diabetes to cancer to Alzheimer’s), this probably has more knock-on benefits too, but we don’t have room to explore all of those today.
Fresh peppers are best for this, but dried peppers (such as when purchased as a ground spice in the supermarket, or when purchased as a capsule-based supplement) still have a very respectable anti-inflammatory effect:
- Capsaicinoids, Polyphenols and Antioxidant Activities of Capsicum annuum: Comparative Study of the Effect of Ripening Stage and Cooking Methods
- A Review on the Effect of Drying on Antioxidant Potential of Fruits and Vegetables
How much should we take?
It’s recommended to start at a low dose and gradually increase it, but 2–6mg of capsaicin per day is the standard range used in studies.
If you’re getting this from peppers, then for example cayenne pepper (a good source of capsaicin) contains around 2.5mg of capsaicin per 1 gram of cayenne.
In the case of capsules, if for example you don’t like eating hot pepper, this will usually mean taking 2–6 capsules per day, depending on dosage.
Make sure to take it with plenty of water!
Where can we get it?
Fresh peppers or ground spice from your local grocery store is fine. Your local health food store probably sells the supplements, too.
If you’d like to buy it online, here is an example product on Amazon.
Note: options on Amazon were more limited than usual, so this product is not vegan, and probably not halal or kosher, as the capsule contains an unspecified gelatin.
Share This Post
Related Posts
-
Lower Your Cortisol! (Here’s Why & How)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cortisol, or “the stress hormone” to its friends, is produced by your adrenal glands, and is generally considered “not fun”.
It does serve a purpose, of course, just like almost everything else our body does. It serves as part of the “fight or flight” response, for example, and helps you to wake up in the morning.
While you do need some cortisol (and a small percentage of people have too little), most of us have too much.
Why? Simply put, modern life is not what 200,000* years of human evolution prepared us for:
- Agriculture (which allowed us to settle down and cease being nomadic) happened during the last 6% of those 200,000 years.
- The Industrial Revolution and the onset of modern capitalism happened during only during the last 0.1% of those 200,000 years.
*the 200,000 years figure is conservative and doesn’t take into account the 200,000,000 years of pre-hominid mammalian evolution. Doing so, on the basis of the mammalian brain & physiology being what’s important here, means our modern stressors have been around for <0.0001% of the time we have.
So guess what, our bodies haven’t caught up. As far as our bodies are concerned, we are supposed to be enjoying the sunshine of grassy plains and the shade of woodland while eating fruit.
- When the alarm clock goes off, our body panics and prepares us to either flee or help fight the predator, because why else would we have been woken so?
- When we have a pressing deadline for work, our brain processes this as “if we don’t do this, we will literally starve and die”.
- When people are upset or angry with us, there’s a part of our brain that fears exile from the tribe and resultant death.
…and so on.
Health Risks of High Cortisol
The long-term stressors are the biggest issue for health. Unless you have a heart condition or other relevant health problem, almost anyone can weather a brief unpleasant surprise. But if something persists? That prompts the body to try to protect you, bless it. The body’s attempts backfire, because…
- One way it does this by making sure to save as much food as possible in the form of body fat
- It’ll also increase your appetite, to make sure you eat anything you can while you still can
- It additionally tries to protect you by keeping you on the brink of fight-or-flight readiness, e.g:
- High blood pressure
- High blood sugar levels
- Rapid mood changes—gotta be able to do those heel-turns as necessary and react quickly to any possible threat!
Suffice it to say, these things are not good for your long-term health.
That’s the “Why”—now here’s the “How”:
Lowering your cortisol levels mostly means lowering your stress and/or lowering your stress response. We previously gave some powerful tools for lowering anxiety, which for these purposes amounts to the same thing.
However, we can also make nutritional and lifestyle changes that will reduce our cortisol levels, for example:
- Reduce (ideally: eliminate from your lifestyle) caffeine
- Reduce (ideally: eliminate from your lifestyle) alcohol
- Yes, really. While many understandably turn to alcohol specifically to help manage stress, it only makes it worse long-term.
- Additionally, alcohol directly stimulates cortisol production, counterintuitive as that may be.
Read: Alcohol, Aging, and the Stress Response ← full article (with 37 sources of its own) from the NYMC covering how alcohol stimulates cortisol production and what that means for us
As well as reductions/eliminations, are some things you can add into your lifestyle that will help!
We’ve written previously about some:
Read: Ashwagandha / Read: L-Theanine / Read: CBD Oil
Other things include, no surprises here:
- The Mediterranean diet (nutritious and delicious): https://10almonds.com/mediterranean-diet
- Get 7–9 hours (good quality!) sleep per night: https://10almonds.com/time-pillow-talk
- Get regular exercise (the regularity matters most!): https://10almonds.com/keep-on-keeping-on
Progressive Relaxation
We’ll give this one its own section because we’ve not talked about it before. Maybe you’re familiar. If not, then in a nutshell: progressive relaxation means progressively tensing and then relaxing each part of your body in turn.
Why does this work? Part of it is just a physical trick involving biofeedback and the natural function of muscles to contract and relax in turn, but the other part is even cleverer:
It basically tricks the most primitive part of your brain, the limbic system, into thinking you had a fight and won, telling it “thank you very much for the cortisol but we don’t need it anymore”.
Take a Hike! Or a Stroll… You Do You!
Last but not least: go connect with your roots. Spend time in the park, or at least the garden. Have a picnic, if the weather suits. Go somewhere you can spend time around leafy green things under a blue sky (we realize the blue sky may be subject to availability in some locations, but do what you can!).
Remember also: just as your body’s responses will be tricked by the alarm clock or the housework, they will also be easily tricked by blue and green stuff around you. If a sunny garden isn’t available in your location, a picture of one as your desktop background is the next best thing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The push for Medicare to cover weight-loss drugs: An explainer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The largest U.S. insurer, Medicare, does not cover weight-loss drugs, making it tougher for older people to get access to promising new medications.
If you cover stories about drug costs in the U.S., it’s important to understand why Medicare’s Part D pharmacy program, which covers people aged 65 and older and people with certain disabilities, doesn’t cover weight-loss drugs today. It’s also important to consider what would happen if Medicare did start covering weight loss drugs. This explainer will give you a brief overview of the issues and then summarize some recent publications the benefits and costs of drugs like semaglutide and tirzepatide.
First, what are these new and newsy weight loss drugs?
Semaglutide is a medication used for both the treatment of type 2 diabetes and for long-term weight management in adults with obesity. It debuted in the United States in 2017 as an injectable diabetes drug called Ozempic, manufactured by Novo Nordisk. It’s part of a class of drugs that mimics the action of glucagon, a substance that the human body makes to aid digestion.
Glucagon-like peptide-1 (GLP-1) drugs like semaglutide help prompt the body to release insulin. But they also cause a minor delay in the pace of digestion, helping people feel sated after eating.
That second effect turned Ozempic into a widely used weight-loss drug, even before the Food and Drug Administration (FDA) gave its okay for this use. Doctors in the United States can prescribe medicines for uses beyond those approved by the FDA. This is known as off-label use.
In writing about her own experience in using the medicine to help her shed 40 pounds, Washington Post columnist Ruth Marcus in June noted that Novo Nordisk mentioned the potential for weight loss in its “ubiquitous cable ads (‘Oh-oh-oh, Ozempic!’)”
The American Society of Health-System Pharmacists has reported shortages of semaglutide due to demand, leaving some people with diabetes struggling to find supply of the medicine.
Novo Nordisk won Food and Drug Administration (FDA) approval in 2021 to market semaglutide as an injectable weight loss drug under the name Wegovy, but with a different dosing regimen than Ozempic. Rival Eli Lilly first won FDA approval of its similar GLP-1 diabetes drug, tirzepatide, in the United States in 2022 and sells it under the brand name Mounjaro.
In November of 2023, Eli Lilly won FDA approval to sell tirzepatide as a weight-loss drug, soon-to-be marketed under the brand name Zepbound. The company said it will set a monthly list price for a month’s supply of the drug at $1,059.87, which the company described as 20% discount to the cost of rival Novo Nordisk’s Wegovy. Wegovy has a list price of $1,349.02, according to the Novo Nordisk website.
Even when their insurance plans officially cover costs for weight loss drugs, consumers may face barriers in seeking that coverage for these drugs. Commercial health plans have in place prior authorization requirements to try to limit coverage of new weight-loss shots to those who qualify for these treatments. The Wegovy shot, for example, is intended for people whose weight reaches a certain benchmark for obesity or who are overweight and have a condition related to excess weight, such as diabetes, high blood pressure or high cholesterol.
State Medicaid programs, meanwhile, have taken approaches that vary by state. For example, the most populous U.S. state, California, provides some coverage to new weight-loss injections through its Medicaid program, but many others, including Texas, the No. 2 state in terms of population, do not, according to an online tool that Novo Nordisk created to help people check on coverage.
Medicare does cover semaglutide for treatment of diabetes, and the insurer reported $3 billion in 2021 spending on the drug under Medicare Part D. Congress last year gave Medicare new tools that might help it try to lower the cost of semaglutide.
Medicare is in the midst of implementing new authority it gained through the Inflation Reduction Act (IRA) of 2022 to negotiate with companies about the cost of certain medicines.
This legislation gave Medicare, for the first time, tools to directly negotiate with pharmaceutical companies on the cost of some medicines. Congress tailored this program to spare drug makers from negotiations for the first few years they put new medicines on the market, allowing them to recoup investment in these products.
Why doesn’t Medicare cover weight-loss drugs?
Congress created the Medicare Part D pharmacy program in 2003 to address a gap in coverage that had existed since the creation of Medicare in 1965. The program long covered the costs of drugs administered by doctors and those given in hospitals, but not the kinds of medicines people took on their own, like Wegovy shots.
In 2003, there seemed to be good reasons to leave weight-loss drugs out of the benefit, write Inmaculada Hernandez of the University of California, San Diego, and coauthors in their September 2023 editorial in the Journal of General Internal Medicine, “Medicare Part D Coverage of Anti-obesity Medications: a Call for Forward-Looking Policy Reform.”
When members of Congress worked on the Part D benefit, the drugs available on the market were known to have limited effectiveness and unpleasant side effects. And those members of Congress were aware of how a drug combination called fen-phen, once touted as a weight-loss miracle medicine, turned out in rare cases to cause fatal heart valve damage. In 1997, American Home Products, which later became Wyeth, took its fen-phen product off the market.
But today GLP-1 drugs like semaglutide appear to offer significant benefits, with far less risk and milder side effects, write Hernandez and coauthors.
“Other than budget impact, it is hard to find a reason to justify the historical statutory exclusion of weight loss drugs from coverage other than the stigma of the condition itself,” they write.
What’s happening today that could lead Medicare to start covering weight loss drugs?
Novo Nordisk and Eli Lilly both have hired lobbyists to try to persuade lawmakers to reverse this stance, according to Senate records. Pro tip: You can use the Senate’s lobbying disclosure database to track this and other issues. Type in the name of the company of interest and then read through the forms.
Some members of Congress already have been trying for years to strike the Medicare Part D restriction on weight-loss drugs. Over the past decade, senators Tom Carper (D-DE) and Bill Cassidy, MD, (R-LA) have repeatedly introduced bills that would do that. They introduced the current version, the Treat and Reduce Obesity Act of 2023, in July. It has the support of 10 other Republican senators and seven Democratic ones, as of Dec. 19. The companion House measure has the support of 41 Democrats and 23 Republicans in that chamber, which has 435 seats.
The influential nonprofit Institute for Clinical and Economic Review conducts in-depth analyses of drugs and medical treatments in the United States. ICER last year recommended passage of a law allowing Medicare Part D to cover weight-loss medications. ICER also called for broader coverage of weight-loss medications in state Medicaid programs. Insurers, including Medicare, consider ICER’s analyses in deciding whether to cover treatments.
While offering these calls for broader coverage as part of a broad assessment of obesity management, ICER also urged companies to reduce the costs of weight-loss medicines.
Most people with obesity can’t achieve sustained weight loss through diet and exercise alone, said David Rind, ICER’s chief medical officer in an August 2022 statement. The development of newer obesity treatments represents the achievement of a long-standing goal of medical research, but prices of these new products must be reasonable to allow broad access to them, he noted.
After an extensive process of reviewing studies, engaging in public debate and processing feedback, ICER concluded that semaglutide for weight loss should have an annual cost of $7,500 to $9,800, based on its potential benefits.
What does academic research say about the benefits and the potential costs of new obesity drugs?
Here are a couple of studies to consider when covering the ongoing story of weight-loss drug costs:
Medicare Part D Coverage of Antiobesity Medications — Challenges and Uncertainty Ahead
Khrysta Baig, Stacie B. Dusetzina, David D. Kim and Ashley A. Leech. New England Journal of Medicine, March 2023In this Perspective piece, researchers at Vanderbilt University create a series of estimates about how much Medicare may have to spend annually on weight-loss drugs if the program eventually covers these drugs.
These include a high estimate — $268 billion — based on an extreme calculation, one reflecting the potential cost if virtually all people on Medicare who have obesity used semaglutide. In an announcement of the study on the Vanderbilt website, lead author Khrysta Baig described this as a “purely hypothetical scenario,” but one that “ underscores that at current prices, these medications cannot be the only way – or even the main way – we address obesity as a society.”
In a more conservative estimate, Bhaig and coauthors consider a case where only about 10% of those eligible for obesity treatment opted for semaglutide, which would result in $27 billion in new costs.
(To put these numbers in context, consider that the federal government now spends about $145 billion a year on the entire Part D program.)
It’s likely that all people enrolled in Part D would have to pay higher monthly premiums if Medicare were to cover weight-loss injections, Baig and coauthors write.
Baig and coauthors note that the recent ICER review of weight-loss drugs focused on patients younger than the Medicare population. The balance of benefits and risks associated with weight-loss drugs may be less favorable for older people than the younger ones, making it necessary to study further how these drugs work for people aged 65 and older, they write. For example, research has shown older adults with a high blood sugar level called prediabetes are less likely to develop diabetes than younger adults with this condition.
SELECTing Treatments for Cardiovascular Disease — Obesity in the Spotlight
Amit Khera and Tiffany M. Powell-Wiley. New England Journal of Medicine, Dec. 14, 2023
Semaglutide and Cardiovascular Outcomes in Patients Without Diabetes
A Michael Lincoff, et. al. New England Journal of Medicine, Dec. 14, 2023.An editorial accompanies the publication of a semaglutide study that drew a lot of coverage in the media. The Semaglutide and Cardiovascular Outcomes in Obesity without Diabetes (SELECT) study was a randomized controlled trial, conducted by Novo Nordisk, which looked at rates of cardiovascular events in people who already had known heart risk and were overweight, but not diabetic. Patients were randomly assigned to receive a once-weekly dose of semaglutide (Wegovy) or a placebo.
In the study, the authors report that of the 8,803 patients who took Wegovy in the trial, 569 (6.5%)
The study also reports a mean 9.4% reduction in body weight among patients taking Wegovy, while those on placebo had a mean loss of 0.88%.
The findings suggest Wegovy may be a welcome new treatment option for many people who have coronary disease and are overweight, but are not diabetic, write Khera and Powell-Wiley in their editorial.
But the duo, both of whom focus on disease prevention in their research, also call for more focus on the prevention and root causes of obesity and on the use of proven treatment approaches other than medication.
“Socioeconomic, environmental, and psychosocial factors contribute to incident obesity, and therefore equity-focused obesity prevention and treatment efforts must target multiple levels,” they write. “For instance, public policy targeting built environment features that limit healthy behaviors can be coupled with clinical care interventions that provide for social needs and access to treatments like semaglutide.”
Additional information:
The nonprofit KFF, formerly known as the Kaiser Family Foundation, has done recent reports looking at the potential for expanded coverage of semaglutide:
Medicaid Utilization and Spending on New Drugs Used for Weight Loss, Sept. 8, 2023
What Could New Anti-Obesity Drugs Mean for Medicare? May 18, 2023
And KFF held an Aug. 4 webinar, New Weight Loss Drugs Raise Issues of Coverage, Cost, Access and Equity, for which the recording is posted here.
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Secret to Mental Health – by George Pransky
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book (and its author) have a sizeable popular following, so it definitely can be said that it has been well-received by many people. The premise in this book is that there is fundamentally nothing wrong with anybody’s brain, and rather everything can be broken down into:
- Mind (the energy and intelligence that animates all life)
- Consciousness (the capacity to be aware of one’s life and experiences)
- Thought (the ability to think, allowing individuals to create their personal experience of reality)
The author explains, over the course of 145 pages, that where anyone with any perceived mental health issue is going wrong is by either lacking self-awareness (Consciousness) or erring by creating an undesirable personal experience of reality (Thought).
In terms of the science of this, frequent references are made to “there is evidence that shows”, “new discoveries about mental health suggest…”, etc, but this claimed evidence is never actually presented, just alluded to. Where many books would have a bibliography, this one has simply a collection of what the author has titled “interesting case studies, conversations, papers, and discussions” (there are no actual case studies or papers; it is just a collection of anecdotes).
The style is… Honestly, in this reviewer’s opinion, barely readable. But, apparently lots of people love it, so your mileage may vary.
We don’t usually delve too far into claimed credentials, but because of the interesting writing style and the bold claims without evidence, we were curious as to where this PhD came from, and apparently it came from a now-shut-down diploma mill that was described by the court as “a complete scam”.
Bottom line: we can’t recommend this one, but we read it so that you don’t have to, and we hope that publishing this review will help reassure you that when we do recommend a book, we mean it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: