Raspberries vs Blackberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing raspberries to blackberries, we picked the blackberries.
Why?
It was very close! Raspberries most certainly also have their merits. But blackberries do just a little bit better in a few categories:
In terms of macros, raspberries have a tiny bit more carbs and fiber, while blackberries have a even tinier bit more protein, and the two berries have an equal glycemic index. We’ll call this category a tie, or else the meanest of nominal wins for raspberry.
In the category of vitamins, raspberries have more of vitamins B1, B2, B5, B6, and choline, while blackberries have more of vitamins A, B3, B9, C, E, and K. This would be a very marginal win for blackberries, except that blackberries have more than 6x the vitamin A, a much larger margin than any of the other differences in vitamins (which were usually small differences), which gives blackberry a more convincing win here.
When it comes to minerals, things are closer: raspberries have more iron, magnesium, manganese, and phosphorus, while blackberries have more calcium, copper, potassium, selenium, and zinc. None of the differences are outstanding, so this is a simple marginal victory for blackberries.
It would be rude to look at berries without noting their polyphenols; we’re not list them all (or this article will get very long, because each has very many polyphenols with names like “pelargonidin 3-O-glucosyl-rutinoside” and so forth), but suffice it to say: raspberries are great for polyphenols and blackberries are even better for polyphenols.
That said… In the category of specific polyphenols we’ve written about before at 10almonds, it’s worth noting a high point of each berry, for the sake of fairness: raspberries have more quercetin (but blackberries have lots too) and blackberries have more ellagic acid (of which, raspberries have some, but not nearly as much). Anyway, just going off total polyphenol content, blackberries are the clear winner here.
Adding up the sections makes for an overall win for blackberries, but by all means, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
21 Most Beneficial Polyphenols & What Foods Have Them
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Mental Health Dangers Of Oversharing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Oversharers can be fun and amiable; the life of the party. In and of itself, this something that can be considered “pro-social” and thus healthy.
But the problem for one’s mental health in the long-run lies in the “over” part of oversharing. Sometimes, if not checking in with the other person’s comfort, oversharing can be “trauma-dumping”, and push people away. Alternatively, if the oversharing exposes an unmet need, it can make the other person feel obliged to try to help in some fashion, which in the long run may also cause awkwardness and withdrawal.
Some potential problems are purely internal, such the feelings of shame or anxiety that can come afterwards; “I should not have been so vulnerable”, “What if my friends think badly of me now?”, etc.
And of course, sometimes those fears are then validated by reality, if “friends” indeed take advantage of that, or withdraw their friendship. That’s a minority occurrence, but it doesn’t make it any less of a crushing thing if it happens.
Sometimes people overshare because of being a bad judge of what’s a socially-approved appropriate amount of sharing; sometimes people overshare out of a need for closeness, and perhaps the hope of hearing what one needed to hear previously.
The dangers of oversharing don’t mean that we should never speak about our experiences and feelings; in fact sometimes, it is the most healthy thing to do—be it because it’s something that needs communicating to a specific person, or because it’s something we just need to “get off our chest”.
In short, it can be good to share! It can also be good to do so judiciously, by conscious decision and not in response to a spur-of-the-moment impulse, and remember to prioritize our own safety.
Below, Alain de Botton explains more of the psychodynamics of this:
Click Here If The Embedded Video Doesn’t Load Automatically!
10almonds tip, not included in the video: unsure whether your urge to share is too impulsive or not? Write a letter/email, and wait until the next day to decide whether or not to send it.
Want to read more?
Check out:
Breathe; Don’t Vent (At Least In The Moment)
Take care!
Share This Post
-
A Peek Behind The 10almonds Curtain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At 10almonds we give a lot of health information, so you may wonder: how much do we (the 10almonds team) put into practice? Is it even possible to do all these things? Do we have an 80:20 rule going on?
So, here’s what someone who thinks, reads, and writes about health all day, does for her health—and how it ties in with what you read here at 10almonds.
Hi, it’s me, a member of the 10almonds team and regular writer here, and I’m going to do the rest of this article in the first-person, since it’s using me as an example!
(PS: yes, the thumbnail is a digital impression of my appearance, though I would correct it that my hair is much longer, and my eyes are more gray; I must admit though it captured my smile, not to mention my collarbones-that-you-could-sit-on)
Dietary habits
Before we get to foods, let’s talk intermittent fasting. I practise 16:8 intermittent fasting… Approximately. That is to say, I’m mostly not religious about it, but I will generally breakfast around 12 noon, and have finished eating dinner before 8pm, with no food outside of those hours.
See also: Intermittent Fasting: What’s the truth?
Importantly, while I feel free to be a little flexible around start and finish times, I do very consciously decide “I am now fasting” and “I will now break the fast”.
Note my imperfection: it would be ideal to have the eating period earlier in the day, and have a bigger breakfast and small dinner. However, that doesn’t really work for me (leisurely evening meal is an important daily event in this household), so this is how I do it instead.
Foods!
It gets an exclamation mark because a thing about me is that I do love foods.
Breakfast: a typical breakfast for me these past months is a couple of ounces of mixed nuts with about 1oz of goji berries.
The mixed nuts are in equal proportions: almonds, walnuts, hazelnuts, cashews. Why those four? Simple, it’s because that’s what Aldi sells as “mixed nuts” and they are the cheapest nuts around, as well as containing absolute nutritional heavyweights almonds and walnuts in generous portions.
Often, but not always, I’ll have some dates with it, or dried apricots, or prunes.
I go through phases; sometimes I’ll enjoy overnight oats as my breakfast for a month or two at a time. I really just follow my gut in this regard.
See for example: Spiced Pear & Pecan Polyphenol Porridge
Lunch: I don’t really lunch per se, but between breakfast and dinner I’ll usually snack on a 3–5 organic carrots (I literally just cut the tops off and otherwise eat them like Bugs Bunny—peeling them would be extra work just to lose fiber). Note my imperfection: I don’t buy all of my vegetables organic, but I do for the ones where it makes the biggest difference.
If I’m feeling like it, I may lunch on a selection of herbs sabzi khordan style (see: Invigorating Sabzi Khordan), though I’m vegan so for simplicity I just skip the cheeses that are also traditional with that dish. On the other hand, for protein and fat I’ll usually add a cup of beans (usually black beans or kidney beans), seasoned with garlic and black pepper in an olive oil and balsamic vinegar dressing (that I make myself, so it’s just those ingredients). See also: Kidney Beans vs Black Beans – Which Is Healthier?
Dinner: this is my main sit-down meal of the day, and it’s enjoyed in a leisurely fashion (say, 40 minutes average with a normal distribution bell curve running between 20 and 60 minutes) with my son who lives with me. I mention all of this, because of the importance of relaxed mindful eating. In the instances of it being nearer the 20 minutes end, it’s not because of rushing, but rather because of a lighter meal some days.
See also: How To Get More Nutrition From The Same Food
Regular recurrences in the menu include:
I’ll often snack on something probiotic (e.g. kimchi) while I’m cooking.
See also: Make Friends With Your Gut! (You Can Thank Us Later)
In terms of what’s not in my diet: as mentioned, I’m vegan, so animal products are out. I don’t drink alcohol or use other recreational drugs, and I mostly drink decaffeinated coffee, but I’ll have a caffeinated one if I’m out somewhere. I’m not a puritan when it comes to sugar, but also, I simply don’t like it and I know well its health effects, so it doesn’t really form part of my diet except insofar as it’s in some ready-made condiments I may sometimes use (e.g. sriracha, teriyaki sauce). I’m also not a puritan when it comes to wheat, but it’s not something I consume daily. Usually on a weekly basis I’ll have a wholegrain pasta dish, and a dish with some kind of wholegrain flatbread.
See also:
Exercise!
First, some things that are lifestyle factors:
- I do not own a car, and I dislike riding in cars, buses, etc. So, I walk everywhere, unless it’s far enough that I must take the train, and even then I usually stand between carriages rather than sitting down.
- I have a standing desk setup, that hasn’t been lowered even once since I got it. I highly recommend it, as someone who spends a lot of time at my desk.
- You may imagine that I spend a lot of time reading; if it’s books (as opposed to scientific papers etc, which I read at my desk), then I’ll most of the time read them while perched like a gargoyle in a sitting squat (Slav squat, Asian squat, resting squat, deep squat, etc) on a balance ball. Yes, it is comfortable once you’re used to it!
About that latter, see also: The Most Anti Aging Exercise
In terms of “actual” exercise, I get 150–300 minutes “moderate exercise” per week, which is mostly composed of:
- Most days I walk into town to get groceries; it’s a 40-minute round trip on foot
- On days I don’t do that, even if I do walk to a more local shop, I spend at least 20 minutes on my treadmill.
See also: The Doctor Who Wants Us To Exercise Less, & Move More
Strength and mobility training, for me, comes mostly in what has been called “exercise snacking”, that is to say, I intersperse my working day with brief breaks to do Pilates exercises. I have theme days (lower body, core, upper body) and on average one rest day (from Pilates exercises) per week, though honestly, that’s usually more likely because of time constraints than anything else, because a deadline is looming.
See also: Four Habits That Drastically Improve Mobility
You may be wondering about HIIT: when I’m feeling extra-serious about it, I use my exercise bike for this, but I’ll be honest, I don’t love the bike, so on a daily basis, I’m much more likely to do HIIT by blasting out a hundred or so Hindu squats, resting, and repeating.
See also: How To Do HIIT (Without Wrecking Your Body)
Supplements
First I’ll mention, I do have HRT, of which the hormones I have are bioidentical estradiol gel in the morning, and a progesterone pessary in the evening. They may not be for everybody, but they’ve made a world of difference to me.
See also: HRT: A Tale Of Two Approaches
In terms of what one usually means when one says supplements, many I use intermittently (which is good in some cases, as otherwise the body may stop using them so well, or other problems can arise), but regular features include:
- Magnesium glycinate, malate, & citrate (See: Which Magnesium? (And: When?))
- Active vitamers of vitamins B9 and B12 (See: Which B Vitamins? It Makes A Difference!)
- Liposomal vitamin C (I actually get enough for general purposes in my diet, but as a vegan I don’t get dietary collagen, so this helps collagen synthesis)
- L-theanine (bedtime only) (See: L-Theanine: What’s The Tea?)
- Lion’s mane mushroom (See: What does lion’s mane mushroom actually do, anyway?)
- Quercetin (See: Fight Inflammation & Protect Your Brain, With Quercetin)
- Fisetin (weekends only) (See: Fisetin: The Anti-Aging Assassin)
Why weekends only for Fisetin? See: The Drug & Supplement Combo That Reverses Aging ← the supplement is fisetin, which outperforms quercetin in this role, and/but it only needs be taken for two days every two weeks, as a sort of “clearing out” of senescent cells. There is no need to take it every day, because if you just cleared out your senescent cells, then guess what, they’re not there now. Also, while sensescent cells are a major cause of aging, on a lower level they do have some anti-tumor effects, so it can be good to let some live a least for a while now and again. In short, cellular sensescence can help prevent tumors on a daily level, but it doesn’t hurt that capacity to have a clearing-out every couple of weeks; so says the science (linked above). Note my imperfection: I take it at weekends instead of for two days every two weeks (as is standard in studies, like those linked above), because it is simpler than remembering to count the weeks.
Cognitive exercise
Lest we forget, exercising our mind is also important! In my case:
- I’m blessed to have work that’s quite cognitively stimulating; our topics here at 10almonds are interesting. If it weren’t for that, I’d still be reading and writing a lot.
- I play chess, though these days I don’t play competitively anymore, and play rather for the social aspect, but this too is important in avoiding cognitive decline.
- I am one of those people who compulsively learns languages, and uses them a lot. This is very beneficial, as language ability is maintained in a few small areas of the brain, and it’s very much “use it or lose it”. Now, while I may not need my French or Russian or Arabic to keep the lights on in this part of the brain or that, the fact that I am pushing my limits every day is the important part. It’s not about how much I know—it’s about how much I engage those parts of my brain on a daily basis. Thus, even if you speak only one language right now, learning even just one more, and learning even only a little bit, you will gain the brain benefits—because you’re engaging it regularly in a new way, and that forces the brain to wire new synapses and also to maintain volume in those parts.
See also: How To Reduce Your Alzheimer’s Risk
And about language-learning specifically: An Underrated Tool Against Alzheimer’s ←this also shows how you don’t have to be extreme about language learning like I admittedly am.
How’s all this working out for me?
I can say: it works! My general health is better now than it was decades ago. I’ve personally focused a lot on reducing inflammation, and that really pays dividends when it comes to the rest of health. I didn’t talk about it above, but focusing on my sleep regularity and quality has helped a lot too.
In terms of measurable results, I recently had a general wellness checkup done by means of a comprehensive panel of 14 blood tests, and various physical metrics (BMI, body fat %, blood pressure, etc), and per those, I could not be in better health; it was as though I had cheated and written in all the best answers. I say this not to brag (you don’t know me, after all), but rather to say: it can be done!
Even without extreme resources, and without an abundance of free time, etc, it can be done!
Caveat: if you have some currently incurable chronic disease, there may be some limits. For example, if you have Type 1 Diabetes, probably your HbA1c* is going to be a little off even if you do everything right.
*HbA1c = glycated hemoglobin, a very accurate measure of what your blood glucose has been on average for the past 2–3 months—why 2–3 months? Because that’s the approximate lifespan of a red blood cell, and we’re measuring how much hemoglobin (in the red blood cells) has been glycated (because of blood glucose).
In summary
The stuff we write about at 10almonds can be implemented, on a modest budget and while juggling responsibilities (work, family, classes, etc).
I’m not saying that my lifestyle should be everyone’s template, but it’s at least an example of one that can work.
- Maybe you hate walking and love swimming.
- Maybe you have no wish to give up fish and eggs, say (both of which are fine/good in moderation healthwise).
- Maybe you have different priorities with supplements.
- Maybe you find language-learning uninteresting but take singing lessons.
- And so on.
In the absolute fewest words, the real template is:
- Decide your health priorities (what matters most for you)
- Look them up on 10almonds
- Put the things into action in a way that works for you!
Take care!
Share This Post
-
Gut-Healthy Spaghetti Chermoula
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chermoula is a Maghreb relish/marinade (it’s used for both purposes); it’s a little like chimichurri but with distinctly N. African flavors. The gut-healthiness starts there (it’s easy to forget that olives—unless fresh—are a fermented food full of probiotic Lactobacillus sp. and thus great for the gut even beyond their fiber content), and continues in the feta, the vegetables, and the wholewheat nature of the pasta. The dish can be enjoyed at any time, but it’s perfect for warm summer evenings—perhaps dining outside, if you’ve place for that.
You will need
- 9oz wholewheat spaghetti (plus low-sodium salt for its water)
- 10oz broccoli, cut into small florets
- 3oz cilantro (unless you have the soap gene)
- 3oz parsley (whether or not you included the cilantro)
- 3oz green olives, pitted, rinsed
- 1 lemon, pickled, rinsed
- 1 bulb garlic
- 3 tbsp pistachios, shelled
- 2 tbsp mixed seeds
- 1 tsp cumin
- 1 tsp chili flakes
- ½ cup extra virgin olive oil
- For the garnish: 3oz feta (or plant-based equivalent), crumbled, 3oz sun-dried tomatoes, diced, 1 tsp cracked black pepper
Note: why are we rinsing the things? It’s because while picked foods are great for the gut, the sodium can add up, so there’s no need to bring extra brine with them too. By doing it this way, there’ll be just the right amount for flavor, without overdoing it.
Method
(we suggest you read everything at least once before doing anything)
1) Cook the spaghetti as you normally would, but when it’s a minute or two from being done, add the broccoli in with it. When it’s done, drain and rinse thoroughly to get rid of excess starch and salt, and also because cooling it even temporarily (as in this case) lowers its glycemic index.
2) Put the rest of the ingredients into a food processor (except the olive oil and the garnish), and blitz thoroughly until no large coarse bits remain. When that’s done, add the olive oil, and pulse it a few times to combine. We didn’t add the olive oil previously, because blending it so thoroughly in that state would have aerated it in a way we don’t want.
3) Put ⅔ of the chermoula you just made into the pan you used for cooking the spaghetti, and set it over a medium heat. When it starts bubbling, return the spaghetti and broccoli to the pan, mixing gently but thoroughly. If the pasta threatens to stick, you can add a little more chermoula, but go easy on it. Any leftover chermoula that you didn’t use today, can be kept in the fridge and used later as a pesto.
4) Serve! Add the garnish as you do.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Less Obvious Probiotics Benefits
- Making Friends With Your Gut (You Can Thank Us Later)
- What Matters Most For Your Heart? ← spoiler: this is why, while we do watch the sodium, we care more about the fiber
- All about Olive Oil: Is “Extra Virgin” Worth It?
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Share This Post
Related Posts
-
Feta or Parmesan – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing feta to parmesan, we picked the parmesan.
Why?
It’s close! Looking at the macros, parmesan has more protein and slightly less fat. Of the fat content, parmesan also has slightly less saturated fat, but neither of them are doing great in this category. Still, a relative win for parmesan.
In the category of vitamins, feta is a veritable vitamin-B-fest with more of vitamins B1, B2, B3, B5, B6, and B9. On the other hand, parmesan has more of vitamins A, B12, and choline. By strength of numbers, this is a win for feta.
Minerals tell a different story; parmesan has a lot more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. Meanwhile, feta is not higher in any minerals. A clear win for parmesan.
Both cheeses offer gut-healthy benefits (if consumed regularly in small portions), while neither are great for the heart.
On balance, we say parmesan wins the day.
Want to learn more?
You might like to read:
Feta Cheese vs Mozzarella – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Should We Skip Shampoo?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝What’s the science on “no poo”? Is it really better for hair? There are so many mixed reports out there.❞
First, for any unfamiliar: this is not about constipation; rather, it is about skipping shampoo, and either:
- Using an alternative cleaning agent, such as vinegar and/or sodium bicarbonate
- Using nothing at all, just conditioner when wet and brushing when dry
Let’s examine why the trend became a thing: the thinking went “shampoo does not exist in nature, and most of our body is more or less self-cleaning; shampoos remove oils from hair, and the body has to produce more sebum to compensate, resulting in a rapid cycle of dry and greasy hair”.
Now let’s fact-check each of those:
- shampoo does not exist in nature: true (except in the sense that everything that exists can be argued to exist in nature, since nature encompasses everything—but the point is that shampoo is a purely artificial human invention)
- most of our body is more or less self-cleaning: true, but our hair is not, for the same reason our nails are not: they’re not really a living part of the overall organism that is our body, so much as a keratinous protrusion of neatly stacked and hardened dead cells from our body. Dead things are not self-cleaning.
- shampoos remove oils from hair: true; that is what they were invented for and they do it well
- the body has to produce more sebum to compensate, resulting in a rapid cycle of dry and greasy hair: false; or at least, there is no evidence for this.
Our hair’s natural oils are great at protecting it, and also great at getting dirt stuck in it. For the former reason we want the oil there; for the latter reason, we don’t.
So the trick becomes: how to remove the oil (and thus the dirt stuck in it) and then put clean oil back (but not too much, because we don’t want it greasy, just, shiny and not dry)?
The popular answer is: shampoo to clean the hair, conditioner to put an appropriate amount of oil* back.
*these days, mostly not actually oil, but rather silicon-based substitutes, that do the same job of protecting hair and keeping it shiny and not brittle, without attracting so much dirt. Remember also that silicon is inert and very body safe; its molecules are simply too large to be absorbed, which is why it gets used in hair products, some skin products, and lube.
See also: Water-based Lubricant vs Silicon-based Lubricant – Which is Healthier?
If you go “no poo”, then what will happen is either you dry your hair out much worse by using vinegar or (even worse) bicarbonate of soda, or you just have oil (and any dirt stuck in it) in your hair for the life of the hair. As in, each individual strand of hair has a lifespan, and when it falls out, the dirt will go with it. But until that day, it’s staying with you, oil and dirt and all.
If you use a conditioner after using those “more natural” harsh cleaners* that aren’t shampoo, then you’ll undo a lot of the damage done, and you’ll probably be fine.
*in fact, if you’re going to skip shampoo, then instead of vinegar or bicarbonate of soda, dish soap from your kitchen may actually do less damage, because at least it’s pH-balanced. However, please don’t use that either.
If you’re going to err one way or the other with regard to pH though, erring on the side of slightly acidic is much better than slightly alkaline.
More on pH: Journal of Trichology | The Shampoo pH can Affect the Hair: Myth or Reality?
If you use nothing, then brushing a lot will mitigate some of the accumulation of dirt, but honestly, it’s never going to be clean until you clean it.
Our recommendation
When your hair seems dirty, and not before, wash it with a simple shampoo (most have far too many unnecessary ingredients; it just needs a simple detergent, and the rest is basically for marketing; to make it foam completely unnecessarily but people like foam, to make it thicker so it feels more substantial, to make it smell nice, to make it a color that gives us confidence it has ingredients in it, etc).
Then, after rinsing, enjoy a nice conditioner. Again there are usually a lot of unnecessary ingredients, but an argument can be made this time for some being more relevant as unlike with the shampoo, many ingredients are going to remain on your hair after rinsing.
Between washes, if you have long hair, consider putting some hair-friendly oil (such as argan oil or coconut oil) on the tips daily, to avoid split ends.
And if you have tight curly hair, then this advice goes double for you, because it takes a lot longer for natural oils to get from your scalp to the ends of your hair. For those of us with straight hair, it pretty much zips straight on down there within a day or two; not so if you have beautiful 4C curls to take care of!
For more on taking care of hair gently, check out:
Gentler Hair Care Options, According To Science
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
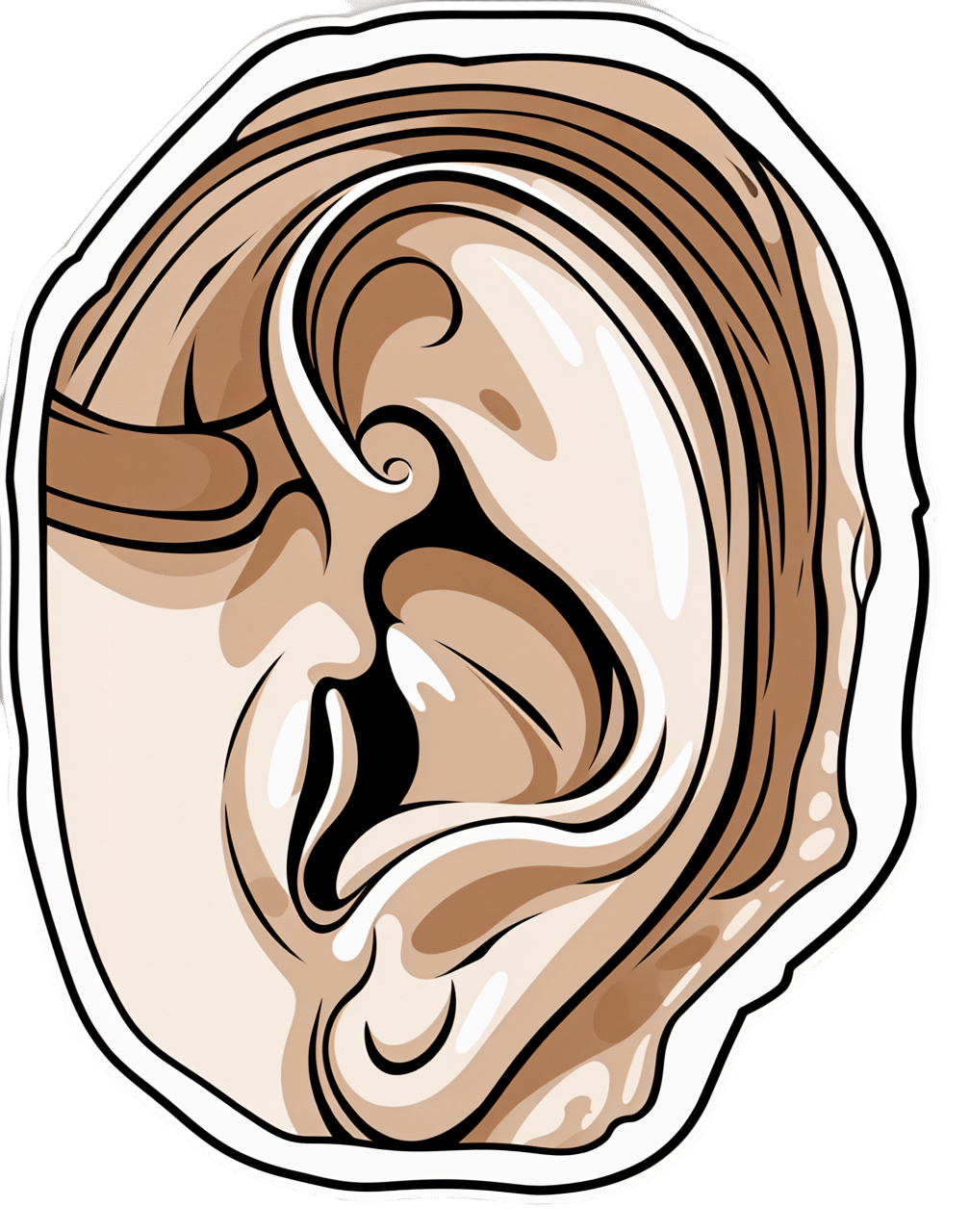
5 Ways To Avoid Hearing Loss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hear Ye, Hear Ye
Hearing loss is often associated with getting older—but it can strike at any age. In the US, for example…
- Around 13% of adults have hearing difficulties
- Nearly 27% of those over 65 have hearing difficulties
Complete or near-complete hearing loss is less common. From the same source…
- A little under 2% of adults in general had a total or near-total inability to hear
- A little over 4% of those over 65 had a total or near-total inability to hear
Source: CDC | Hearing Difficulties Among Adults: United States, 2019
So, what to do if we want to keep our hearing as it is?
Avoid loud environments
An obvious one, but it bears stating for the sake of being methodical. Loud environments damage our ears, but how loud is too loud?
You can check how loud an environment is by using a free smartphone app, such as:
Decibel Pro: dB Sound Level Meter (iOS / Android)
An 82 dB environment is considered safe for 16 hours. That’s the equivalent of, for example moderate traffic.
Every 3 dB added to that halves the safe exposure time, for example:
- An 85 dB environment is considered safe for 8 hours. That’s the equivalent of heavier traffic, or a vacuum cleaner.
- A 94 dB environment is considered safe for 1 hour. That might be a chainsaw, a motorcycle, or a large sporting event.
Many nightclubs or concert venues often have environments of 110 dB and more. So the safe exposure time would be under two minutes.
Source: NIOSH | Noise and Hearing Loss
With differences like that per 3 dB increase, then you may want to wear hearing protection if you’re going to be in a noisy environment.
Discreet options include things like these -20 dB silicone ear plugs that live in a little case on one’s keyring.
Stop sticking things in your ears
It’s said “nothing smaller than your elbow should go in your ear canal”. We’ve written about this before:
What’s Good (And What’s Not) Against Earwax
Look after the rest of your health
Our ears are not islands unaffected by the rest of our health, and indeed, they’re larger and more complex organs than we think about most of the time, since we only tend to think about the (least important!) external part.
Common causes of hearing loss that aren’t the percussive injuries we discussed above include:
- Diabetes
- High blood pressure
- Smoking
- Infections
- Medications
Lest that last one sound a little vague, it’s because there are hundreds of medications that have hearing loss as a potential side-effect. Here’s a list so you can check if you’re taking any of them:
List of Ototoxic Medications That May Cause Tinnitus or Hearing Loss
Get your hearing tested regularly.
There are online tests, but we recommend an in-person test at a local clinic, as it won’t be subject to the limitations and quirks of the device(s) you’re using. Pretty much anywhere that sells hearing aids will probably offer you a free test, so take advantage of it!
And, more generally, if you suddenly notice you lost some or all of your hearing in one or more ears, then get thee to a doctor, and quickly.
Treat it as an emergency, because there are many things that can be treated if and only if they are caught early, before the damage becomes permanent.
Use it or lose it
This one’s important. As we get older, it’s easy to become more reclusive, but the whole “neurons that fire together, wire together” neuroplasticity thing goes for our hearing too.
Our brain is, effectively, our innermost hearing organ, insofar as it processes the information it receives about sounds that were heard.
There are neurological hearing problems that can show up without external physical hearing damage (auditory processing disorders being high on the list), but usually these things are comorbid with each other.
So if we want to maintain our ability to process the sounds our ears detect, then we need to practice that ability.
Important implication:
That means that if you might benefit from a hearing aid, you should get it now, not later.
It’s counterintuitive, we know, but because of the neurological consequences, hearing aids help people retain their hearing, whereas soldiering on without can hasten hearing loss.
On the topic of hearing difficulty comorbidities…
Tinnitus (ringing in the ears) is, paradoxically, associated with both hearing loss, and with hyperacusis (hearing supersensitivity, which sounds like a superpower, but can be quite a problem too).
Learn more about managing that, here:
Tinnitus: Quieting The Unwanted Orchestra In Your Ears
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: