Zucchini & Oatmeal Koftas
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
These vegetarian (and with one tweak, vegan) koftas are delicious as a snack, light lunch, or side to a larger meal. Healthwise, they contain the healthiest kind of fiber, as well as omega-3 fatty acids, and beneficial herbs and spices.
You will need
- ¼ cup oatmeal
- 1 large zucchini, grated
- 1 small carrot, grated
- ¼ cup cheese (your preference; vegan is also fine)
- 2 tbsp ground flaxseed
- 2 tbsp nutritional yeast
- ¼ bulb garlic, minced
- 2 tsp black pepper, coarse ground
- ½ tsp MSG or 1 tsp low-sodium salt
- Small handful fresh parsley, chopped
- Extra virgin olive oil, for frying
Method
(we suggest you read everything at least once before doing anything)
1) Soak the flaxseed in 2 oz hot water for at least 5 minutes
2) Combine all of the ingredients except the olive oil (and including the water that the flax has been soaking in) in a big bowl, mixing thoroughly
3) Shape into small balls, patties, or sausage shapes, and fry until the color is golden and the structural integrity is good. If doing patties, you’ll need to gently flip them to cook both sides; otherwise, rolling them to get all sides is fine.
4) Serve! Traditional is with some kind of yogurt dip, but we’re not the boss of you, so enjoy them how you like:

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- The Best Kind Of Fiber For Overall Health? ← it’s β-glucan, as found in oats
- What Omega-3 Fatty Acids Really Do For Us ← as in the flax
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk? ← it’s healthier than table salt
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Beat Food Addictions!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When It’s More Than “Just” Cravings
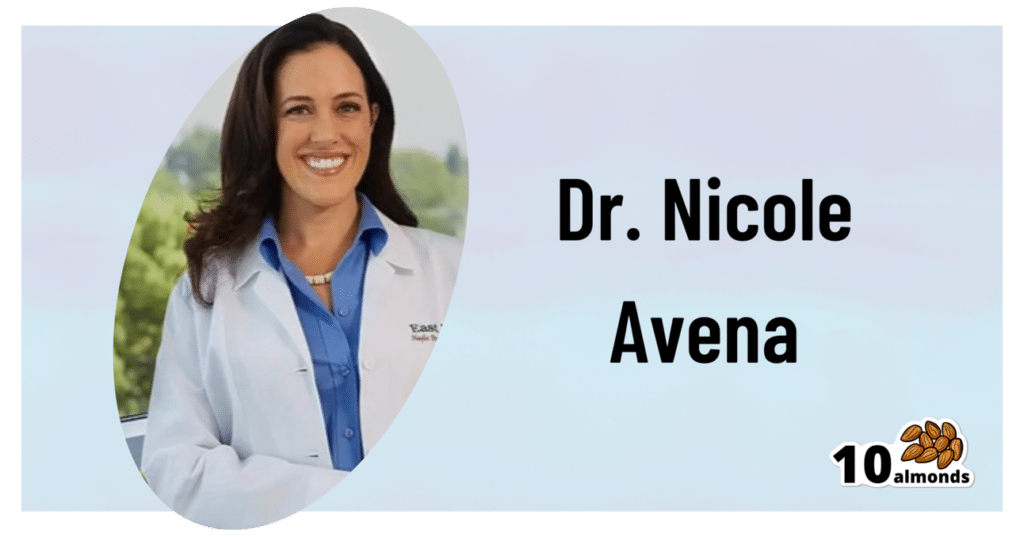
This is Dr. Nicole Avena. She’s a research neuroscientist who also teaches at Mount Sinai School of Medicine, as well as at Princeton. She’s done a lot of groundbreaking research in the field of nutrition, diet, and addition, with a special focus on women’s health and sugar intake specifically.
What does she want us to know?
Firstly, that food addictions are real addictions.
We know it can sound silly, like the famous line from Mad Max:
❝Do not, my friends, become addicted to water. It will take hold of you and you will resent its absence!❞
As an aside, it is actually possible to become addicted to water; if one drinks it excessively (we are talking gallons every day) it does change the structure of the brain (no surprise; the brain is not supposed to have that much water!) causing structural damage that then results in dependency, and headaches upon withdrawal. It’s called psychogenic polydipsia:
But back onto today’s more specific topic, and by a different mechanism of addiction…
Food addictions are dopaminergic addictions (as is cocaine)
If you are addicted to a certain food (often sugar, but other refined carbs such as potato products, and also especially refined flour products, are also potential addictive substances), then when you think about the food in question, your brain lights up with more dopamine than it should, and you are strongly motivated to seek and consume the substance in question.
Remember, dopamine functions by expectation, not by result. So until your brain’s dopamine-gremlin is sated, it will keep flooding you with motivational dopamine; that’s why the first bite tastes best, then you wolf down the rest before your brain can change its mind, and afterwards you may be left thinking/feeling “was that worth it?”.
Much like with other addictions (especially alcohol), shame and regret often feature strongly afterwards, even accompanied by notions of “never again”.
But, binge-eating is as difficult to escape as binge-drinking.
You can break free, but you will probably have to take it seriously
Dr. Avena recommends treating a food addiction like any other addiction, which means:
- Know why you want to quit (make a list of the reasons, and this will help you stay on track later!)
- Make a conscious decision to genuinely quit
- Learn about the nature of the specific addiction (know thy enemy!)
- Choose a strategy (e.g. wean off vs cold turkey, and decide what replacements, if any, you will use)
- Get support (especially from those around you, and/but the support of others facing, or who have successfully faced, the same challenge is very helpful too)
- Keep track of your success (build and maintain a streak!)
- Lean into how you will better enjoy life without addiction to the substance (it never really made you happy anyway, so enjoy your newfound freedom and good health!)
Want more from Dr. Avena?
You can check out her column at Psychology Today here:
Psychology Today | Food Junkie ← it has a lot of posts about sugar addiction in particular, and gives a lot of information and practical advice
You can also read her book, which could be a great help if you are thinking of quitting a sugar addiction:
Sugarless: A 7-Step Plan to Uncover Hidden Sugars, Curb Your Cravings, and Conquer Your Addiction
Enjoy!
Share This Post
-
Unleashing Your Best Skin – by Jennifer Sun
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, an aesthetician with a biotech background, explains about the overlap of skin health and skin beauty, making it better from the inside first (diet and other lifestyle factors), and then tweaking things as desired from the outside.
In the broad category of “tweakments” as she puts it, she covers most of the wide array of modern treatments available at many skin care clinics and the options for which at-home do-it-yourself kits are available—and the pros and cons of various approaches.
And yes, those methods do range from microneedling and red light therapy to dermal fillers and thread lifts. Most of them are relatively non-invasive though.
She also covers common ailments of the skin, and how to identify and treat those quickly and easily, without making things worse along the way.
One last thing she also includes is dealing with unwanted hairs—being a very common side-along issue when it comes to aesthetic medicine.
The book is broadly aimed at women, but hormones are not a main component discussed (except in the context of acne), so there’s no pressing reason why this book couldn’t benefit men too. It also addresses considerations when it comes to darker skintones, something that a lot of similar books overlook.
Bottom line: if you find yourself mystified by the world of skin treatment options and wondering what’s really best for you without the bias of someone who’s trying to sell you a particular treatment, then this is the book for you.
Click here to check out Unleashing Your Best Skin, and unleash your best skin!
Share This Post
-
Eggplant vs Zucchini – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing eggplant to zucchini, we picked the zucchini.
Why?
In terms of macros, eggplant has more carbs and fiber while zucchini has more protein; we’ll generally prioritize fiber, so call this a subjective win for eggplant in this category, though an argument could be made for a tie.
In the category of vitamins, eggplant has more of vitamins B3, B5, and E, while zucchini has more of vitamins A, B1, B2, B6, B9, C, K, and choline, scoring a win for zucchini here.
Looking at minerals, eggplant has more copper, manganese, and selenium, while zucchini has more calcium, iron, magnesium, phosphorus, potassium and zinc, meaning another win for zucchini in this round.
In terms of polyphenols, eggplant has a greater variety of polyphenols, while zucchini has greater total mass of polyphenols, so we’re calling this one a tie.
Adding up the sections makes for an overall win for zucchini, but by all means enjoy either or both (perhaps together!); diversity is good!
Want to learn more?
You might like:
What’s Your Plant Diversity Score?
Enjoy!
Share This Post
Related Posts
-
Healthy Choco-Banoffee Ice Cream
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chocolate, banana, and coffee—quite a threesome, whether for breakfast or dessert, and this is healthy enough for breakfast while being decadent enough for dessert! With no dairy or added sugar, and lots of antioxidants, this is a healthy way to start or end your day.
You will need
- 3 bananas
- 2 tbsp cocoa powder, no additives
- 2 shots espresso, chilled
- 1 tsp vanilla extract
- On standby: milk of your choice—we recommend almond or hazelnut
Method
(we suggest you read everything at least once before doing anything)
1) Peel, slice, and freeze the bananas (let them freeze for at least 2–3 hours)
2) Blend the ingredients, except the milk. Add milk as necessary if the mixture is too thick to blend. Be careful not to add too much at once though, or it will become less of an ice cream and more of a milkshake!
3) Scoop into a sundae glass to serve:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Which Plant Milk?
- The Bitter Truth About Coffee (or is it?)
- Cacao vs Carob – Which is Healthier?
- Apples vs Bananas – Which is Healthier?
- Which Sugars Are Healthier, And Which Are Just The Same?
- Tasty Polyphenols
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Darwin’s Bed Rest: Worthwhile Idea?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I recall that Charles Darwin (of Evolution fame) used to spend a day a month in bed in order to maintain his physical and psychological equilibrium. Do you see merit in the idea?❞
Well, it certainly sounds wonderful! Granted, it may depend on what you do in bed :p
Descartes did a lot of his work from bed (and also a surprising amount of it while hiding in an oven, but that’s another story), which was probably not so good for the health.
As for Darwin, his health was terrible in quite a lot of ways, so he may not be a great model.
However! Certainly taking a break is well-established as an important and healthful practice:
How To Rest More Efficiently (Yes, Really)
❝I don’t like to admit it but I am getting old. Recently, I had my first “fall” (ominous word!) I was walking across some wet decking and, before I knew what had happened, my feet were shooting forwards, and I crashed to the ground. Luckily I wasn’t seriously damaged. But I was wondering whether you can give us some advice about how best to fall. Maybe there are some good videos on the subject? I would like to be able to practice falling so that it doesn’t come as such a shock when it happens!❞
This writer has totally done the same! You might like our recent main feature on the topic:
…if you’ll pardon the pun
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Sweet Truth About Glycine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Make Your Collagen Work Better
This is Dr. James Nicolantonio. He’s a doctor of pharmacy, and a research scientist. He has a passion for evidence-based nutrition, and has written numerous books on the subject.
Controversy! Dr. DiNicolatonio’s work has included cardiovascular research, in which field he has made the case for increasing (rather than decreasing) the recommended amount of salt in our diet. This, of course, goes very much against the popular status quo.
We haven’t reviewed that research so we won’t comment on it here, but we thought it worth a mention as a point of interest. We’ll investigate his claims in that regard another time, though!
Today, however, we’ll be looking at his incisive, yet not controversial, work pertaining to collagen and glycine.
A quick recap on collagen
We’ve written about collagen before, and its importance for maintaining… Well, pretty much most of our body, really, buta deficiency in collagen can particularly weaken bones and joints.
On a more surface level, collagen’s also important for healthy elastic skin, and many people take it for that reason alone,
Since collagen is found only in animals, even collagen supplements are animal-based (often marine collagen or bovine collagen). However, if we don’t want to consume those, we can (like most animals) synthesize it ourselves from the relevant amino acids, which we can get from plants (and also laboratories, in some cases).
You can read our previous article about this, here:
We Are Such Stuff As Fish Are Made Of
What does he want us to know about collagen?
We’ll save time and space here: first, he’d like us to know the same as what we said in our article above
However, there is also more:
Let’s assume that your body has collagen to process. You either consumed it, or your body has synthesized it. We’ll skip describing the many steps of collagen synthesis, fascinating as that is, and get to the point:
When our body weaves together collagen fibrils out of the (triple-helical) collagen molecules…
- the cross-linking of the collagen requires lysyl oxidase
- the lysyl oxidase (which we make inside us) deanimates some other amino acids yielding aldehydes that allow the stable cross-links important for the high tensile strength of collagen, but to do that, it requires copper
- in order to use the copper it needs to be in its reduced cuprous form and that requires vitamin C
- but moving it around the body requires vitamin A
So in other words: if you are taking (or synthesizing) collagen, you also need copper and vitamins A and C.
However! Just to make things harder, if you take copper and vitamin C together, it’ll reduce the copper too soon in the wrong place.
Dr. DiNicolantonio therefore advises taking vitamin C after copper, with a 75 minutes gap between them.
What does he want us to know about glycine?
Glycine is one of the amino acids that makes up collagen. Specifically, it makes up every third amino acid in collagen, and even more specifically, it’s also the rate-limiting factor in the formation of glutathione, which is a potent endogenous (i.e., we make it inside us) antioxidant that works hard to fight inflammation inside the body.
What this means: if your joints are prone to inflammation, being glycine-deficient means a double-whammy of woe.
As well as being one of the amino acids most key to collagen production, glycine has another collagen-related role:
First, the problem: as we age, glycated collagen accumulates in the skin and cartilage (that’s bad; there is supposed to be collagen there, but not glycated).
More on glycation and what it is and why it is so bad:
Are You Eating Advanced Glycation End-Products? The Trouble Of The AGEs
Now, the solution: glycine suppresses advanced glycation end products, including the glycation of collagen.
See for example:
With these three important functions of glycine in mind…
Dr. DiNicolantonio therefore advises getting glycine at a dose of 100mg/kg/day. So, if you’re the same size as this rather medium-sized writer, that means 7.2g/day.
Where can I get it?
Glycine is found in many foods, including gelatin for those who eat that, eggs for the vegetarians, and spinach for vegans.
However, if you’d like to simply take it as a supplement, here’s an example product on Amazon
(the above product is not clear whether it’s animal-derived or not, so if that’s important to you, shop around. This writer got some locally that is certified vegan, but is in Europe rather than N. America, which won’t help most of our subscribers)
Note: pure glycine is a white crystalline powder that has the same sweetness as glucose. Indeed, that is how it got its name, from the Greek “γλυκύς”, pronounced /ɡly.kýs/, meaning “sweet”. Yes, same etymology as glucose.
So don’t worry that you’ve been conned if you order it and think “this is sugar!”; it just looks and tastes the same.
That does mean you should buy from a reputable source though, as a con would be very easy!
this does also mean that if you like a little sugar/sweetener in your tea or coffee, glycine can be used as a healthy substitute.
If you don’t like sweet tastes, then, condolences. This writer pours two espresso coffees (love this decaffeinated coffee that actually tastes good), puts the glycine in the first, and then uses the second to get rid of the sweet taste of the first. So that’s one way to do it.
Enjoy (if you can!)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: