Why You Should Diversify Your Nuts!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Time to go nuts for nuts!
Nuts, in popular perception, range from “basically the healthiest food anyone can eat” to “basically high calorie salty snacks”. And, they can be either!
Some notes, then:
- Raw is generally better that not
- Dry roasted is generally better than the kind with added oils
- Added salt is neither necessary nor good
Quick tip: if “roasted salted” are the cheapest or most convenient to buy, you can at least mitigate that by soaking them in warm water for 5 minutes, before rinsing and (if you don’t want wet nuts) drying.
You may be wondering: who does want wet nuts? And the answer is, if for example you’re making a delicious cashew and chickpea balti, the fact you didn’t dry them before throwing them in won’t make a difference.
Now, let’s do a quick run-down; we don’t usually do “listicles” but it seemed a good format here, so we’ve picked a top 5 for nutritional potency:
Almonds
We may have a bias. We accept it. But almonds are also one of the healthiest nuts around, and generally considered by most popular metrics the healthiest.
Not only are they high in protein, healthy fat, fiber, vitamins, and minerals, but they’re even a natural prebiotic that increases the populations of healthy gut bacteria, while simultaneously keeping down the populations of gut pathogens—what more can we ask of a nut?
Read more: Prebiotic effects of almonds and almond skins on intestinal microbiota in healthy adult humans
Pistachios
Not only are these super tasty and fun to eat (and mindful eating is all but guaranteed, as shelling them by hand slows us down and makes us more likely to eat them one at a time rather than by the handful), but also they contain lots of nutrients and are lower in calories than most nuts, so they’re a great option for anyone who’d like to eat more nuts but is doing a calorie-controlled diet and doesn’t want to have half a day’s calories in a tiny dish of nuts.
Walnuts
Popularly associated with brain health (perhaps easy to remember because of their appearance), they really are good for the brain:
Check it out: Beneficial Effects of Walnuts on Cognition and Brain Health
Cashews
A personal favorite of this writer for their versatility in cooking, food prep, or just as a snack, they also do wonders for metabolic health:
Brazil nuts
The most exciting thing about these nuts is that they’re an incredibly potent source of selenium, which is important not just for hair/skin/nails as popularly marketed, but also for thyroid hormone production and DNA synthesis.
But don’t eat too many, because selenium is definitely one of those “you can have too much of a good thing” nutrients, and selenium poisoning can make your hair (however beautiful and shiny it got because of the selenium) fall out if you take too much.
Know the numbers: Brazil nuts and selenium—health benefits and risks
Bottom line on nuts:
- Nuts are a great and healthful part of almost anyone’s diet
- Obviously, if you have a nut allergy, then we’re sorry; this one won’t have helped you so much
- Almonds are one of the most healthful nuts out there
- Brazil nuts are incredibly potent, to the point where moderation is recommended
- A handful of mixed nuts per day is a very respectable option—when it comes to food and health, diversity is almost always good!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Brain-Skin Doctor
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Of Brains And Breakouts
Today’s spotlight is on Dr. Claudia Aguirre. She’s a molecular neuroscientist, and today she’s going to be educating us about skin.
What? Why?
When we say “neuroscience”, we generally think of the brain. And indeed, that’s a very important part of it.
We might think about eyes, which are basically an extension of the brain.
We don’t usually think about skin, which (just like our eyes) is constantly feeding us a lot of information about our surroundings, via a little under three million nerve endings. Guess where the other ends of those nerves lead!
There’s a constant two-way communication going on between our brain and our skin.
What does she want us to know?
Psychodermatology
The brain and the skin talk to each other, and maladies of one can impact the other:
- Directly, e.g. stress prompting skin breakouts (actually this is a several-step process physiologically, but for the sake of brevity we’ll call this direct)
- Indirectly, e.g. nervous disorders that result in people scratching or picking at their skin, which prompts a whole vicious cycle of one thing making the other worse
Read more: Psychodermatology: The Brain-Skin Connection
To address both kinds of problems, clearly something beyond moisturizer is needed!
Mindfulness (meditation and beyond)
Mindfulness is a well-evidenced healthful practice for many reasons, and Dr. Aguirra argues the case for it being good for our skin too.
As she points out,
❝Cultural stress and anxiety can trigger or aggravate many skin conditions—from acne to eczema to herpes, psoriasis, and rosacea.
Conversely, a disfiguring skin condition can trigger stress, anxiety, depression, and even suicide.
Chronic, generalized anxiety can create chronic inflammation and exacerbate inflammatory skin conditions, such as those I mentioned previously.
Chronic stress can result in chronic anxiety, hypervigilance, poor sleep, and a whole cascade of effects resulting in a constant breakdown of tissues and organs, including the skin.❞
So, she recommends mindfulness-based stress reduction (MBSR), for the above reasons, along with others!
Read more: Mind Matters
How to do it: No-Frills, Evidence-Based Mindfulness
And as for “and beyond?”
Do you remember in the beginning of the pandemic, when people were briefly much more consciously trying to avoid touching their faces so much? That, too, is mindfulness. It may have been a stressed and anxious mindfulness for many*, but mindfulness nonetheless.
*which is why “mindfulness-based stress reduction” is not a redundant tautology repeated more than once unnecessarily, one time after another 😉
So: do try to keep aware of what you are doing to your skin, and so far as is reasonably practicable, only do the things that are good for it!
The skin as an endocrine organ
Nerves are not the only messengers in the body; hormones do a lot of our body’s internal communication too. And not just the ones everyone remembers are hormones (e.g. estrogen, testosterone, although yes, they do both have a big impact on skin too), but also many more, including some made in the skin itself!
Dr. Aguirra gives us a rundown of common conditions, the hormones behind them, and what we can do if we don’t want them:
Read more: Rethinking The Skin As An Endocrine Organ
Take-away advice:
For healthy skin, we need to do more than just hydrate, get good sleep, have good nutrition, and get a little sun (but not too much).
- We should also practice mindfulness-based stress reduction, and seek help for more serious mental health issues.
- We should also remember the part our hormones play in our skin, and not just the obvious ones.
Did you know that vitamin D is also a hormone, by the way? It’s not the only hormone at play in your skin by a long way, but it is an important one:
Society for Endocrinology | Vitamin D
Want to know more?
You might like this interview with Dr. Aguirre:
The Brain in Our Skin: An Interview with Dr. Claudia Aguirre
Take care!
Share This Post
-
Peach vs Papaya – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing peach to papaya, we picked the peach.
Why?
It was close!
In terms of macros, there’s not much between them; they are close to identical on protein, carbs, and fiber. Technically peach has slightly more protein (+0.4g/100g) and papaya has slightly more carbs and fiber (+1.28g/100g carbs, +0.2g/100g fiber), but since the differences are so tiny, we’re calling this section a tie—bearing in mind, these numbers are based on averages, which means that when they’re very close, they’re meaningless—one could easily, for example, pick up a peach that has more fiber than a papaya, because that 0.2g/100g is well within the margin of variation. So, as we say: a tie.
When it comes to vitamins, things are also close; peaches have more of vitamins B1, B2, B3, and E, while papaya has more of vitamins A, B6, B9, and C. This is a 4:4 tie, but since the most notable margin of difference is vitamin C (of which papayas have 9x more) while the others are much closer, we’ll call this a tie-breaker win for papaya.
The category of minerals sets things apart more: peaches have more copper, iron, manganese, phosphorus, potassium, and zinc, while papaya has more calcium, magnesium, and selenium. That’s already a 6:3 win for peaches, before we take into account that the numbers for papaya’s calcium and selenium are tiny, so adding this to the already 6:3 win for peaches makes for a clear and easy win for peaches in this category.
Adding up the sections is 1W/1D/1L for both fruits, but looking at the win/loss for each, it’s clear which won/lost on a tiebreaker, and which won/lost by a large margin, so peaches get the victory here.
Of course, enjoy either or both, though! And see below for a bonus feature of peaches:
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← peaches are high on this list! They kill cancer cells while sparing healthy ones 🙂
Take care!
Share This Post
-
Food and exercise can treat depression as well as a psychologist, our study found. And it’s cheaper
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Around 3.2 million Australians live with depression.
At the same time, few Australians meet recommended dietary or physical activity guidelines. What has one got to do with the other?
Our world-first trial, published this week, shows improving diet and doing more physical activity can be as effective as therapy with a psychologist for treating low-grade depression.
Previous studies (including our own) have found “lifestyle” therapies are effective for depression. But they have never been directly compared with psychological therapies – until now.
Amid a nation-wide shortage of mental health professionals, our research points to a potential solution. As we found lifestyle counselling was as effective as psychological therapy, our findings suggest dietitians and exercise physiologists may one day play a role in managing depression.
Alexander Raths/shutterstock What did our study measure?
During the prolonged COVID lockdowns, Victorians’ distress levels were high and widespread. Face-to-face mental health services were limited.
Our trial targeted people living in Victoria with elevated distress, meaning at least mild depression but not necessarily a diagnosed mental disorder. Typical symptoms included feeling down, hopeless, irritable or tearful.
We partnered with our local mental health service to recruit 182 adults and provided group-based sessions on Zoom. All participants took part in up to six sessions over eight weeks, facilitated by health professionals.
Half were randomly assigned to participate in a program co-facilitated by an accredited practising dietitian and an exercise physiologist. That group – called the lifestyle program – developed nutrition and movement goals:
Lifestyle therapy aims to improve diet. Jonathan Borba/Pexels - eating a wide variety of foods
- choosing high-fibre plant foods
- including high quality fats
- limiting discretionary foods, such as those high in saturated fats and added sugars
- doing enjoyable physical activity.
The second group took part in psychotherapy sessions convened by two psychologists. The psychotherapy program used cognitive behavioural therapy (CBT), the gold standard for treating depression in groups and when delivered remotely.
In both groups, participants could continue existing treatments (such as taking antidepressant medication). We gave both groups workbooks and hampers. The lifestyle group received a food hamper, while the psychotherapy group received items such as a colouring book, stress ball and head massager.
Lifestyle therapies just as effective
We found similar results in each program.
At the trial’s beginning we gave each participant a score based on their self-reported mental health. We measured them again at the end of the program.
Over eight weeks, those scores showed symptoms of depression reduced for participants in the lifestyle program (42%) and the psychotherapy program (37%). That difference was not statistically or clinically meaningful so we could conclude both treatments were as good as each other.
There were some differences between groups. People in the lifestyle program improved their diet, while those in the psychotherapy program felt they had increased their social support – meaning how connected they felt to other people – compared to at the start of the treatment.
Participants in both programs increased their physical activity. While this was expected for those in the lifestyle program, it was less expected for those in the psychotherapy program. It may be because they knew they were enrolled in a research study about lifestyle and subconsciously changed their activity patterns, or it could be a positive by-product of doing psychotherapy.
People in both groups reported doing more physical activity. fongbeerredhot/Shutterstock There was also not much difference in cost. The lifestyle program was slightly cheaper to deliver: A$482 per participant, versus $503 for psychotherapy. That’s because hourly rates differ between dietitians and exercise physiologists, and psychologists.
What does this mean for mental health workforce shortages?
Demand for mental health services is increasing in Australia, while at the same time the workforce faces worsening nation-wide shortages.
Psychologists, who provide about half of all mental health services, can have long wait times. Our results suggest that, with the appropriate training and guidelines, allied health professionals who specialise in diet and exercise could help address this gap.
Lifestyle therapies can be combined with psychology sessions for multi-disciplinary care. But diet and exercise therapies could prove particularly effective for those on waitlists to see a psychologists, who may be receiving no other professional support while they wait.
Many dietitians and exercise physiologists already have advanced skills and expertise in motivating behaviour change. Most accredited practising dietitians are trained in managing eating disorders or gastrointestinal conditions, which commonly overlap with depression.
There is also a cost argument. It is overall cheaper to train a dietitian ($153,039) than a psychologist ($189,063) – and it takes less time.
Potential barriers
Australians with chronic conditions (such as diabetes) can access subsidised dietitian and exercise physiologist appointments under various Medicare treatment plans. Those with eating disorders can also access subsidised dietitian appointments. But mental health care plans for people with depression do not support subsidised sessions with dietitians or exercise physiologists, despite peak bodies urging them to do so.
Increased training, upskilling and Medicare subsidies would be needed to support dietitians and exercise physiologists to be involved in treating mental health issues.
Our training and clinical guidelines are intended to help clinicians practising lifestyle-based mental health care within their scope of practice (activities a health care provider can undertake).
Future directions
Our trial took place during COVID lockdowns and examined people with at least mild symptoms of depression who did not necessarily have a mental disorder. We are seeking to replicate these findings and are now running a study open to Australians with mental health conditions such as major depression or bipolar disorder.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Adrienne O’Neil, Professor, Food & Mood Centre, Deakin University and Sophie Mahoney, Associate Research Fellow, Food and Mood Centre, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
An RSV vaccine has been approved for people over 60. But what about young children?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Therapeutic Goods Administration (TGA) has approved a vaccine against respiratory syncytial virus (RSV) in Australia for the first time. The shot, called Arexvy and manufactured by GSK, will be available by prescription to adults over 60.
RSV is a contagious respiratory virus which causes an illness similar to influenza, most notably in babies and older adults.
So while it will be good to have an RSV vaccine available for older people, where is protection up to for the youngest children?
A bit about RSV
RSV was discovered in chimpanzees with respiratory illness in 1956, and was soon found to be a common cause of illness in humans.
There are two key groups of people we would like to protect from RSV: babies (up to about one year old) and people older than 60.
Babies tend to fill up hospitals during the RSV season in late spring and winter in large numbers, but severe infection requiring admission to intensive care is less common.
In babies and younger children, RSV generally causes a wheezing asthma-like illness (bronchiolitis), but can also cause pneumonia and croup.
Although there are far fewer hospital admissions among older people, they can develop severe disease and die from an infection.
Babies account for the majority of hospitalisations with RSV.
Prostock-studio/ShutterstockRSV vaccines for older people
For older adults, there are actually several RSV vaccines in the pipeline. The recent Australian TGA approval of Arexvy is likely to be the first of several, with other vaccines from Pfizer and Moderna currently in development.
The GSK and Pfizer RSV vaccines are similar. They both contain a small component of the virus, called the pre-fusion protein, that the immune system can recognise.
Both vaccines have been shown to reduce illness from RSV by more than 80% in the first season after vaccination.
In older adults, side effects following Arexvy appear to be similar to other vaccines, with a sore arm and generalised aches and fatigue frequently reported.
Unlike influenza vaccines which are given each year, it is anticipated the RSV vaccine would be a one-off dose, at least at this stage.
Protecting young children from RSV
Younger babies don’t tend to respond well to some vaccines due to their immature immune system. To prevent other diseases, this can be overcome by giving multiple vaccine doses over time. But the highest risk group for RSV are those in the first few months of life.
To protect this youngest age group from the virus, there are two potential strategies available instead of vaccinating the child directly.
The first is to give a vaccine to the mother and rely on the protective antibodies passing to the infant through the placenta. This is similar to how we protect babies by vaccinating pregnant women against influenza and pertussis (whooping cough).
The second is to give antibodies directly to the baby as an injection. With both these strategies, the protection provided is only temporary as antibodies wane over time, but this is sufficient to protect infants through their highest risk period.
Women could be vaccinated during pregnancy to protect their baby in its first months of life.
Image Point Fr/ShutterstockAbrysvo, the Pfizer RSV vaccine, has been trialled in pregnant women. In clinical trials, this vaccine has been shown to reduce illness in infants for up to six months. It has been approved in pregnant women in the United States, but is not yet approved in Australia.
An antibody product called palivizumab has been available for many years, but is only partially effective and extremely expensive, so has only been given to a small number of children at very high risk.
A newer antibody product, nirsevimab, has been shown to be effective in reducing infections and hospitalisations in infants. It was approved by the TGA in November, but it isn’t yet clear how this would be accessed in Australia.
What now?
RSV, like influenza, is a major cause of respiratory illness, and the development of effective vaccines represents a major advance.
While the approval of the first vaccine for older people is an important step, many details are yet to be made available, including the cost and the timing of availability. GSK has indicated its vaccine should be available soon. While the vaccine will initially only be available on private prescription (with the costs paid by the consumer), GSK has applied for it to be made free under the National Immunisation Program.
In the near future, we expect to hear further news about the other vaccines and antibodies to protect those at higher risk from RSV disease, including young children.
Allen Cheng, Professor of Infectious Diseases, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A Fresh Take On Hypothyroidism
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
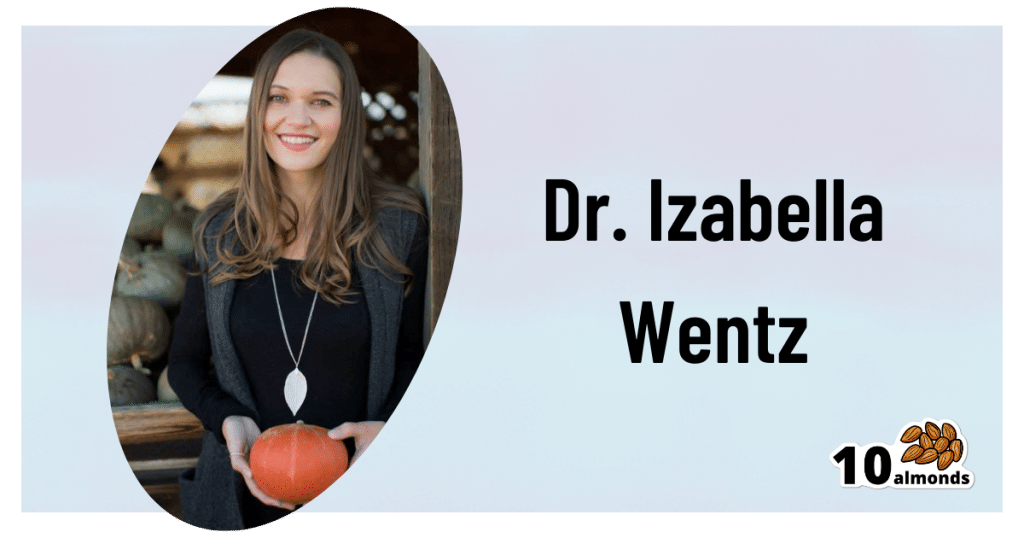
The Three Rs To Boost Thyroid-Related Energy Levels
This is Dr. Izabella Wentz. She’s a doctor of pharmacology, and after her own diagnosis with Hashimoto’s thyroiditis, she has taken it up as her personal goal to educate others on managing hypothyroidism.
Dr. Wentz is also trained in functional medicine through The Institute for Functional Medicine, Kalish Functional Medicine, and the American Academy of Anti-Aging Medicine. She is a Fellow of the American Society of Consultant Pharmacists, and holds certifications in Medication Therapy Management as well as Advanced Diabetes Care through the American Pharmacists Association. In 2013, she received the Excellence in Innovation Award from the Illinois Pharmacists Association.
Dr. Wentz’s mission
Dr. Wentz was disenchanted by the general medical response to hypothyroidism in three main ways. She tells us:
- Thyroid patients are not diagnosed appropriately.
- For this, she criticises over-reliance on TSH tests that aren’t a reliable marker of thyroid function, especially if you have Hashimoto’s.
- Patients should be better optimized on their medications.
- For this, she criticizes many prescribed drugs that are actually pro-drugs*, that don’t get converted adequately if you have an underactive thyroid.
- Lifestyle interventions are often ignored by mainstream medicine.
- Medicines are great; they truly are. But medicating without adjusting lifestyle can be like painting over the cracks in a crumbling building.
*a “pro-drug” is what it’s called when the drug we take is not the actual drug the body needs, but is a precursor that will get converted to that actual drug we need, inside our body—usually by the liver, but not always. An example in this case is T4, which by definition is a pro-drug and won’t always get correctly converted to the T3 that a thyroid patient needs.
Well that does indeed sound worthy of criticism. But what does she advise instead?
First, she recommends a different diagnostic tool
Instead of (or at least, in addition to) TSH tests, she advises to ask for TPO tests (thyroid peroxidase), and a test for Tg antibodies (thyroglobulin). She says these are elevated for many years before a change in TSH is seen.
Next, identify the root cause and triggers
These can differ from person to person, but in countries that add iodine to salt, that’s often a big factor. And while gluten may or may not be a factor, there’s a strong correlation between celiac disease and Hashimoto’s disease, so it is worth checking too. Same goes for lactose.
By “checking”, here we mean testing eliminating it and seeing whether it makes a difference to energy levels—this can be slow, though, so give it time! It is best to do this under the guidance of a specialist if you can, of course.
Next, get to work on repairing your insides.
Remember we said “this can be slow”? It’s because your insides won’t necessarily bounce back immediately from whatever they’ve been suffering from for what’s likely many years. But, better late than never, and the time will pass anyway, so might as well get going on it.
For this, she recommends a gut-healthy diet with specific dietary interventions for hypothyroidism. Rather than repeat ourselves unduly here, we’ll link to a couple of previous articles of ours, as her recommendations match these:
She also recommends regular blood testing to see if you need supplementary TSH, TPO antibodies, and T3 and T4 hormones—as well as vitamin B12.
Short version
After diagnosis, she recommends the three Rs:
- Remove the causes and triggers of your hypothyroidism, so far as possible
- Repair the damage caused to your body, especially your gut
- Replace the thyroid hormones and related things in which your body has become deficient
Learn more
If you’d like to learn more about this, she offers a resource page, with resources ranging from on-screen information, to books you can get, to links to hook you up with blood tests if you need them, as well as recommended supplements to consider.
She also has a blog, which has an interesting relevant article added weekly.
Enjoy, and take care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Thyroid patients are not diagnosed appropriately.
-
The Best Kind Of Fiber For Overall Health?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Fiber Of Good Health
We’ve written before about how most people in industrialized nations in general, and N. America in particular, do not get nearly enough fiber:
Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
Fiber’s important for many aspects of health, not least of all the heart:
What Matters Most For Your Heart? Eat More (Of This) For Lower Blood Pressure
As well, of course, as being critical for gut health:
Gut Health 101: Making Friends With Your Gut (You Can Thank Us Later)
But is all fiber “prebiotic fiber”, and/or are some better than others?
Beta-glucan
A recent study (it’s a mouse study, but promising in its applicability for humans) examined the health impacts of 5 different fiber types:
- pectin
- β-glucan
- wheat dextrin
- resistant starch
- cellulose (control)
As for health metrics, they measured:
- body weight
- adiposity
- indirect calorimetry
- glucose tolerance
- gut microbiota
- metabolites thereof
What they found was…
❝Only β-glucan supplementation during HFD-feeding decreased adiposity and body weight gain and improved glucose tolerance compared with HFD-cellulose, whereas all other fibers had no effect. This was associated with increased energy expenditure and locomotor activity in mice compared with HFD-cellulose.
All fibers supplemented into an HFD uniquely shifted the intestinal microbiota and cecal short-chain fatty acids; however, only β-glucan supplementation increased cecal butyrate concentrations. Lastly, all fibers altered the small-intestinal microbiota and portal bile acid composition. ❞
If you’d like to read more, the study itself is here:
If you’d like to read less, the short version is that they are all good but β-glucan scored best in several metrics.
It also acts indirectly as a GLP-1 agonist, by the way:
The right fiber may help you lose weight
You may be wondering: what is β-glucan found in?
It’s found in many (non-animal product) foods, but oats, barley, mushrooms, and yeasts are all good sources.
Is it available as a supplement?
More or less; there are supplements that contain it generously, here’s an example product on Amazon, a cordyceps extract, of which >30% is β-glucan.
As an aside, cordyceps itself has many other healthful properties too:
Cordyceps: Friend Or Foe? ← the answer is, it depends! If you’re human, it’s a friend.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: