The Vegan Instant Pot Cookbook – by Nisha Vora
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We all know that we should “eat the rainbow” (and that no, Skittles do not count)… So why do we often find ourselves falling into the same familiar habits and well-worn comfort foods?
Nisha Vora, of “Rainbow Plant Life“, is here to make things a lot easier—brightening up our plates is her mission!
In this Instant Pot-authorized, beautifully illustrated cookbook, Vora offers us 90 recipes to do just that. And because it’s an Instant Pot cookbook, they’re all super easy.
What if you don’t have an Instant Pot? Well, don’t tell Instant Pot we said this, but another pressure cooker brand will work too. And if you don’t have any pressure cooker, the recipes are modifiable for regular pots and pans. The recipes also lend themselves well to slow-cooker cooking, for that matter!
Where Vora really excels though is in making mostly-one-pot dishes beautiful and tasty.
The recipes, by the way, are drawn from cuisines from all around the world, and cover:
- summer and winter dishes
- breakfasts, sides, mains, desserts
- the healthy and the decadent (and sometimes both!)
As for the presentation of each recipe, we get at least one full-page photo of the finished dish and sometimes extras of the steps. We get a little intro, the usual information about ingredients etc, and a no-fuss step-by-step method. It’s very easy to use.
If you have allergies or other dietary considerations, this book is pretty mindful of those, making substitutions minimal and easy.
Bottom line: this comprehensive book will seriously brighten up the colors of your cooking!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
From eye exams to blood tests and surgery: how doctors use light to diagnose disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is the next article in our ‘Light and health’ series, where we look at how light affects our physical and mental health in sometimes surprising ways. Read other articles in the series.
You’re not feeling well. You’ve had a pounding headache all week, dizzy spells and have vomited up your past few meals.
You visit your GP to get some answers and sit while they shine a light in your eyes, order a blood test and request some medical imaging.
Everything your GP just did relies on light. These are just some of the optical technologies that have had an enormous impact in how we diagnose disease.
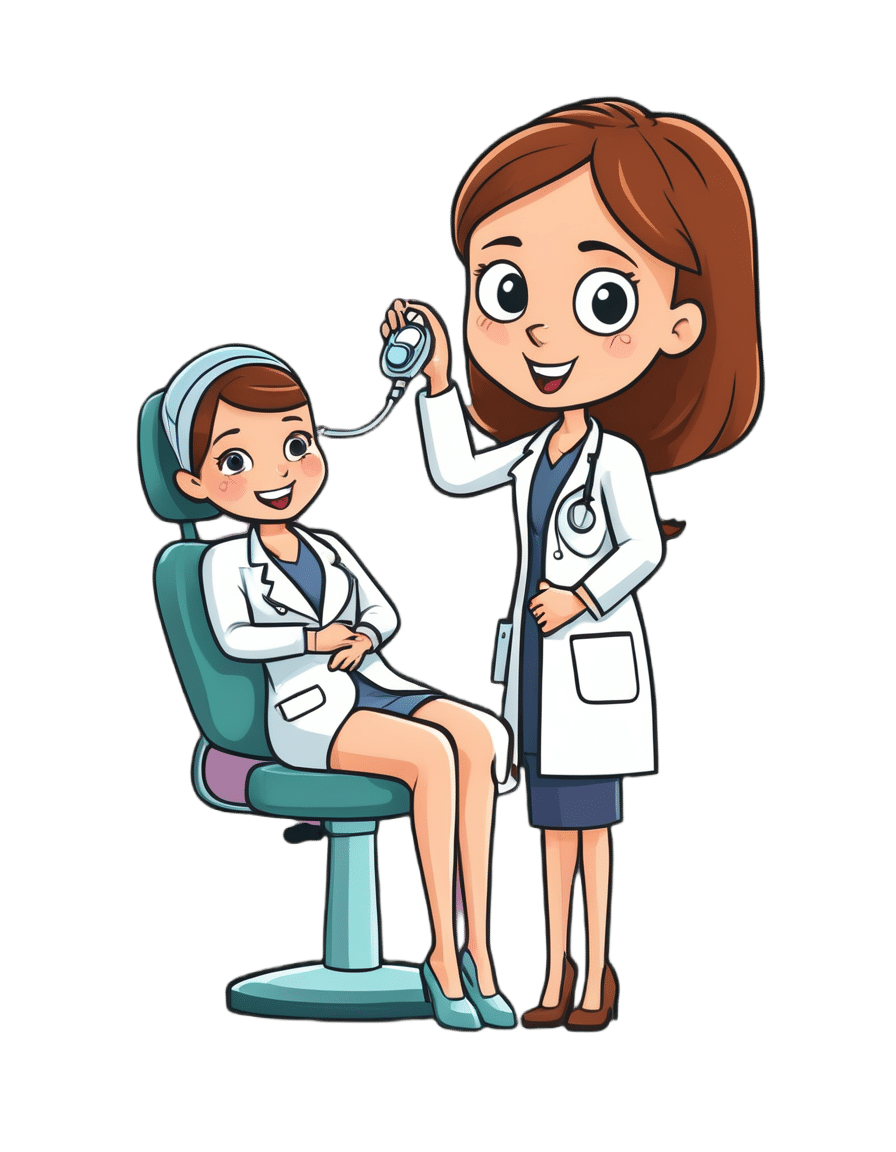
megaflopp/Shutterstock 1. On-the-spot tests
Point-of-care diagnostics allow doctors to test patients on the spot and get answers in minutes, rather than sending samples to a lab for analysis.
The “flashlight” your GP uses to view the inside of your eye (known as an ophthalmoscope) is a great example. This allows doctors to detect abnormal blood flow in the eye, deformations of the cornea (the outermost clear layer of the eye), or swollen optical discs (a round section at the back of the eye where the nerve link to the brain begins). Swollen discs are a sign of elevated pressure inside your head (or in the worst case, a brain tumour) that could be causing your headaches.
The invention of lasers and LEDs has enabled many other miniaturised technologies to be provided at the bedside or clinic rather than in the lab.
Pulse oximetry is a famous example, where a clip attached to your finger reports how well your blood is oxygenated. It does this by measuring the different responses of oxygenated and de-oxygenated blood to different colours of light.
Pulse oximetry is used at hospitals (and sometimes at home) to monitor your respiratory and heart health. In hospitals, it is also a valuable tool for detecting heart defects in babies.
See that clip on the patient’s finger? That’s a pulse oximeter, which relies on light to monitor respiratory and heart health. CGN089/Shutterstock 2. Looking at molecules
Now, back to that blood test. Analysing a small amount of your blood can diagnose many different diseases.
A machine called an automated “full blood count analyser” tests for general markers of your health. This machine directs focused beams of light through blood samples held in small glass tubes. It counts the number of blood cells, determines their specific type, and reports the level of haemoglobin (the protein in red blood cells that distributes oxygen around your body). In minutes, this machine can provide a snapshot of your overall health.
For more specific disease markers, blood serum is separated from the heavier cells by spinning in a rotating instrument called a centrifuge. The serum is then exposed to special chemical stains and enzyme assays that change colour depending on whether specific molecules, which may be the sign of a disease, are present.
These colour changes can’t be detected with the naked eye. However, a light beam from an instrument called a spectrometer can detect tiny amounts of these substances in the blood and determine if the biomarkers for diseases are present, and at what levels.
Light shines through the blood sample and tells us whether biomarkers for disease are present. angellodeco/Shutterstock 3. Medical imaging
Let’s re-visit those medical images your GP ordered. The development of fibre-optic technology, made famous for transforming high-speed digital communications (such as the NBN), allows light to get inside the body. The result? High-resolution optical imaging.
A common example is an endoscope, where fibres with a tiny camera on the end are inserted into the body’s natural openings (such as your mouth or anus) to examine your gut or respiratory tracts.
Surgeons can insert the same technology through tiny cuts to view the inside of the body on a video screen during laparoscopic surgery (also known as keyhole surgery) to diagnose and treat disease.
Doctors can insert this flexible fibre-optic tube with a camera on the end into your body. Eduard Valentinov/Shutterstock How about the future?
Progress in nanotechnology and a better understanding of the interactions of light with our tissues are leading to new light-based tools to help diagnose disease. These include:
- nanomaterials (materials on an extremely small scale, many thousands of times smaller than the width of a human hair). These are being used in next-generation sensors and new diagnostic tests
- wearable optical biosensors the size of your fingernail can be included in devices such as watches, contact lenses or finger wraps. These devices allow non-invasive measurements of sweat, tears and saliva, in real time
- AI tools to analyse how blood serum scatters infrared light. This has allowed researchers to build a comprehensive database of scatter patterns to detect any cancer
- a type of non-invasive imaging called optical coherence tomography for more detailed imaging of the eye, heart and skin
- fibre optic technology to deliver a tiny microscope into the body on the tip of a needle.
So the next time you’re at the GP and they perform (or order) some tests, chances are that at least one of those tests depend on light to help diagnose disease.
Matthew Griffith, Associate Professor and ARC Future Fellow and Director, UniSA Microscopy and Microanalysis Facilities, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Mammography AI Can Cost Patients Extra. Is It Worth It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As I checked in at a Manhattan radiology clinic for my annual mammogram in November, the front desk staffer reviewing my paperwork asked an unexpected question: Would I like to spend $40 for an artificial intelligence analysis of my mammogram? It’s not covered by insurance, she added.
I had no idea how to evaluate that offer. Feeling upsold, I said no. But it got me thinking: Is this something I should add to my regular screening routine? Is my regular mammogram not accurate enough? If this AI analysis is so great, why doesn’t insurance cover it?
I’m not the only person posing such questions. The mother of a colleague had a similar experience when she went for a mammogram recently at a suburban Baltimore clinic. She was given a pink pamphlet that said: “You Deserve More. More Accuracy. More Confidence. More power with artificial intelligence behind your mammogram.” The price tag was the same: $40. She also declined.
In recent years, AI software that helps radiologists detect problems or diagnose cancer using mammography has been moving into clinical use. The software can store and evaluate large datasets of images and identify patterns and abnormalities that human radiologists might miss. It typically highlights potential problem areas in an image and assesses any likely malignancies. This extra review has enormous potential to improve the detection of suspicious breast masses and lead to earlier diagnoses of breast cancer.
While studies showing better detection rates are extremely encouraging, some radiologists say, more research and evaluation are needed before drawing conclusions about the value of the routine use of these tools in regular clinical practice.
“I see the promise and I hope it will help us,” said Etta Pisano, a radiologist who is chief research officer at the American College of Radiology, a professional group for radiologists. However, “it really is ambiguous at this point whether it will benefit an individual woman,” she said. “We do need more information.”
The radiology clinics that my colleague’s mother and I visited are both part of RadNet, a company with a network of more than 350 imaging centers around the country. RadNet introduced its AI product for mammography in New York and New Jersey last February and has since rolled it out in several other states, according to Gregory Sorensen, the company’s chief science officer.
Sorensen pointed to research the company conducted with 18 radiologists, some of whom were specialists in breast mammography and some of whom were generalists who spent less than 75% of their time reading mammograms. The doctors were asked to find the cancers in 240 images, with and without AI. Every doctor’s performance improved using AI, Sorensen said.
Among all radiologists, “not every doctor is equally good,” Sorensen said. With RadNet’s AI tool, “it’s as if all patients get the benefit of our very top performer.”
But is the tech analysis worth the extra cost to patients? There’s no easy answer.
“Some people are always going to be more anxious about their mammograms, and using AI may give them more reassurance,” said Laura Heacock, a breast imaging specialist at NYU Langone Health’s Perlmutter Cancer Center in New York. The health system has developed AI models and is testing the technology with mammograms but doesn’t yet offer it to patients, she said.
Still, Heacock said, women shouldn’t worry that they need to get an additional AI analysis if it’s offered.
“At the end of the day, you still have an expert breast imager interpreting your mammogram, and that is the standard of care,” she said.
About 1 in 8 women will be diagnosed with breast cancer during their lifetime, and regular screening mammograms are recommended to help identify cancerous tumors early. But mammograms are hardly foolproof: They miss about 20% of breast cancers, according to the National Cancer Institute.
The FDA has authorized roughly two dozen AI products to help detect and diagnose cancer from mammograms. However, there are currently no billing codes radiologists can use to charge health plans for the use of AI to interpret mammograms. Typically, the federal Centers for Medicare & Medicaid Services would introduce new billing codes and private health plans would follow their lead for payment. But that hasn’t happened in this field yet and it’s unclear when or if it will.
CMS didn’t respond to requests for comment.
Thirty-five percent of women who visit a RadNet facility for mammograms pay for the additional AI review, Sorensen said.
Radiology practices don’t handle payment for AI mammography all in the same way.
The practices affiliated with Boston-based Massachusetts General Hospital don’t charge patients for the AI analysis, said Constance Lehman, a professor of radiology at Harvard Medical School who is co-director of the Breast Imaging Research Center at Mass General.
Asking patients to pay “isn’t a model that will support equity,” Lehman said, since only patients who can afford the extra charge will get the enhanced analysis. She said she believes many radiologists would never agree to post a sign listing a charge for AI analysis because it would be off-putting to low-income patients.
Sorensen said RadNet’s goal is to stop charging patients once health plans realize the value of the screening and start paying for it.
Some large trials are underway in the United States, though much of the published research on AI and mammography to date has been done in Europe. There, the standard practice is for two radiologists to read a mammogram, whereas in the States only one radiologist typically evaluates a screening test.
Interim results from the highly regarded MASAI randomized controlled trial of 80,000 women in Sweden found that cancer detection rates were 20% higher in women whose mammograms were read by a radiologist using AI compared with women whose mammograms were read by two radiologists without any AI intervention, which is the standard of care there.
“The MASAI trial was great, but will that generalize to the U.S.? We can’t say,” Lehman said.
In addition, there is a need for “more diverse training and testing sets for AI algorithm development and refinement” across different races and ethnicities, said Christoph Lee, director of the Northwest Screening and Cancer Outcomes Research Enterprise at the University of Washington School of Medicine.
The long shadow of an earlier and largely unsuccessful type of computer-assisted mammography hangs over the adoption of newer AI tools. In the late 1980s and early 1990s, “computer-assisted detection” software promised to improve breast cancer detection. Then the studies started coming in, and the results were often far from encouraging. Using CAD at best provided no benefit, and at worst reduced the accuracy of radiologists’ interpretations, resulting in higher rates of recalls and biopsies.
“CAD was not that sophisticated,” said Robert Smith, senior vice president of early cancer detection science at the American Cancer Society. Artificial intelligence tools today are a whole different ballgame, he said. “You can train the algorithm to pick up things, or it learns on its own.”
Smith said he found it “troubling” that radiologists would charge for the AI analysis.
“There are too many women who can’t afford any out-of-pocket cost” for a mammogram, Smith said. “If we’re not going to increase the number of radiologists we use for mammograms, then these new AI tools are going to be very useful, and I don’t think we can defend charging women extra for them.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
The Cluttered Mind – by Deborah McKenna
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Coming from an eclectic psychotherapy background, Deborah McKenna outlines a wide array of techniques to “do what it says on the tin”, that is:
Organizing the junk drawer of your mind.
McKenna argues that it’s natural for something so gargantuan as our mind to get cluttered… but that it’s perfectly possible, with a good system, to tidy up considerably.
The benefit of this is much like the benefit of tidying a room:
Imagine a kitchen in which half the things have not been put away; there are dishes in the sink, something is growing behind the trash can… and you have a vague suspicion that if you open a certain cupboard, its contents are going to come falling out on your head. How are you going to cook a meal here?
Imagine a mind when many thoughts have been left untended; there are things you needed to process, and there’s a steady resentment of something growing in some dark part of your mind… and there’s some part of your memory that you’re afraid to even look at it, because of all it’ll cause to come surging back at you. How are you going to strategize your life here?
Fortunately, McKenna is here to guide you through doing for your mind what Marie Kondo would do for your home. And, even better, McKenna does it with a simple and clear writing style, assorted diagrams, and a step-by-step approach to getting everything in order.
Give Your Mind A Spring-Cleaning With This Book From Amazon Today
Share This Post
Related Posts
-
Antihistamines for Runny Nose?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Do you have any articles about using Anti-Histamines? My nose seems to be running a lot. I don’t have a cold or any allergies that I know of. I tried a Nasal spray Astepro, but it doesn’t do much.?❞
Just for you, we wrote such an article yesterday in response to this question!
The Astepro that you tried, by the way, is a brand name of the azelastine we mentioned near the end, before we got to talking about systemic corticosteroids such as beclometasone dipropionate—this latter might help you if antihistamines haven’t, and if your doctor advises there’s no contraindication (for most people it is safe for there are exceptions, such as if you are immunocompromised and/or currently fighting some infection).
You can find more details on all this in yesterday’s article, which in case you missed it, can be found at:
Antihistamines’ Generation Gap: Are You Ready For Allergy Season?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Good Health From Head To Toe
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Q: I am now in the “aging” population. A great concern for me is Alzheimers. My father had it and I am so worried. What is the latest research on prevention?
Very important stuff! We wrote about this not long back:
- See: How To Reduce Your Alzheimer’s Risk
- See also: Brain Food? The Eyes Have It!
(one good thing to note is that while Alzheimer’s has a genetic component, it doesn’t appear to be hereditary per se. Still, good to be on top of these things, and it’s never too early to start with preventive measures!)
Q: Foods that help build stronger bones and cut inflammation? Thank you!
We’ve got you…
For stronger bones / To cut inflammation
That “stronger bones” article is about the benefits of collagen supplementation for bones, but there’s definitely more to say on the topic of stronger bones, so we’ll do a main feature on it sometime soon!
Q: Veganism, staying mentally sharp, best exercises for weight gain?
All great stuff! Let’s do a run-down:
- Veganism? As a health and productivity newsletter, we’ll only be focusing veganism’s health considerations, but it does crop up from time to time! For example:
- Which Plant Milk? (entirely about such)
- Plant vs Animal Protein (mostly about such)
- Making Friends With Your Gut (You Can Thank Us Later) (discusses one benefit of such)
- Staying mentally sharp? You might like the things-against-dementia pieces we linked to in the previous response!
- It’s also worth noting that some kinds of dementia, such as Alzheimer’s, can begin the neurodegenerative process 20 years before symptoms show, and can be influenced by lifestyle choices 20 years before that, so it’s definitely never too early be on top of these things!
- Best exercises for weight gain? We’ll do a main feature one of these days (filled with good science and evidence), but in few words meanwhile: core exercises, large muscle groups, heavy weights, few reps, build up slowly. Squats are King.
Q: I am interested in the following: Aging, Exercise, Diet, Relationships, Purpose, Lowering Stress
You’re going to love our Psychology Sunday editions of 10almonds! You might like some of these…
- Relationships: Seriously Useful Communication Skills!
- Purpose: Are You Flourishing? (There’s a Scale)
- Managing stress: Lower Your Cortisol! (Here’s Why & How)
- Also about managing stress: Sunday Stress-Buster
- Also applicable to stress: How To Set Your Anxiety Aside
Q: I’d like to know more about type 2 diabetic foot problems
You probably know that the “foot problems” thing has less to do with the feet and more to do with blood and nerves. So, why the feet?
The reason feet often get something like the worst of it, is because they are extremities, and in the case of blood sugars being too high for too long too often, they’re getting more damage as blood has to fight its way back up your body. Diabetic neuropathy happens when nerves are malnourished because the blood that should be keeping them healthy, is instead syrupy and sluggish.
We’ll definitely do a main feature sometime soon on keeping blood sugars healthy, for both types of diabetes plus pre-diabetes and just general advice for all.
In the meantime, here’s some very good advice on keeping your feet healthy in the context of diabetes. This one’s focussed on Type 1 Diabetes, but the advice goes for both:
! Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eye Exercises That Measurably Improve Your Vision
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our eyesight, like most of the rest of our body’s functions, will decline if not adequately maintained. Modern lifestyles see most of us indoors for most of the day (which means a reduced maximum focal length) and often looking at screens (even further reduced focal length), which means that part of our eyes responsible for focus will tend to atrophy and wither. And if we want to see something better, we adjust the settings instead of adjusting our eyes. However, it is perfectly possible to recover our clear youthful vision:
See the results for yourself (and see them clearly!)
The exercises that gave him the results he showed between the two tests, are:
- Blink for 30 seconds
- Focus on something in front and (keeping your focus on that stationary point) move your head left & right, upwards & downwards, and diagonally
- Take a break and blink for 30 seconds
- Keep your head still while you move your eyes left & right, upwards & downwards, and diagonally
- Focus on something in front while you move move your head left & right, upwards & downwards, and diagonally
This should temporarily improve your vision immediately, because of what has been going on in the capillaries in and around your eyes, but sustained results require sustained (i.e. daily) practice. This is because the vasculature is only part of the mechanism; it’s also a matter of improving the muscles responsible for focusing the eyes—and like any muscles, it’s not a case of “do it once and enjoy the results forever”. So, even just 2–3 minutes each day is recommended.
For more on all of this plus a visual demonstration, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Are Your Glasses Making Your Eyesight Worse?
or, if you are very serious about having excellent vision for life:
Vision for Life, Revised Edition – by Dr. Meir Schneider ← this one’s a book, and a very good one at that
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: