Statins: Study Insights
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Q: Can you let us know about more studies that have been done on statins? Are they really worth taking?
That is a great question! We imagine it might have been our recent book recommendation that prompted it? It’s quite a broad question though, so we’ll do that as a main feature in the near future!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Asparagus vs Edamame – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing asparagus to edamame, we picked the edamame.
Why?
Perhaps it’s a little unfair comparing a legume to a vegetable that’s not leguminous (given legumes’ high protein content), but these two vegetables often serve a similar culinary role, and there is more to nutrition than protein. That said…
In terms of macros, edamame has a lot more protein and fiber; it also has more carbs, but the ratio is such that edamame still has the lower glycemic index. Thus, the macros category is a win for edamame in all relevant aspects.
When it comes to vitamins, things are a little closer; asparagus has more of vitamins A, B3, and C, while edamame has more of vitamins B1, B2, B5, B6, and B9. All in all, a moderate win for edamame, unless we want to consider the much higher vitamin C content of asparagus as particularly more relevant.
In the category of minerals, asparagus boasts only more selenium (and more sodium, not that that’s a good thing for most people in industrialized countries), while edamame has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. An easy win for edamame.
In short, enjoy both (unless you have a soy allergy, because edamame is young soy beans), but edamame is the more nutritionally dense by far.
Want to learn more?
You might like to read:
Take care!
Share This Post
-
Best Workouts for Women Over 40 To Give Your Metabolism A Makeover
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
After 40, the usual course of events goes: your lean muscle mass decreases, which slows your metabolism and makes it easier to gain fat. At the same time, bone density decreases, increasing the risk of osteoporosis and frailty. This leads to lower mobility, flexibility, and overall frustration.
But it doesn’t have to be that way! Fitness coach Jessica Cooke explains how:
It all depends on this
Strength training helps counteract these effects by increasing lean muscle mass, which boosts metabolism and fat burning. It also improves bone density, reducing the risk of osteoporosis. Plus, it builds strength, fitness, and a toned physique.
The best part? It doesn’t require long workouts—short, effective sessions work best.
While walking is very beneficial for general health, it doesn’t provide the resistance needed to build muscle. Without resistance, your body composition won’t change, and so your metabolism will remain the same. Strength training is essential for burning fat at rest and improving overall fitness.
You don’t have to do high-impact exercises or jumping to see results. Low-impact strength training is effective and gentle on the joints. Lifting weights or using your body weight in a controlled manner will help build muscle and improve strength.
Many women only do cardio and neglect strength training, leading to minimal progress. Another common mistake is overcomplicating workouts—simple, consistent strength training is all you need.
Aim to strength train three times per week for 20 minutes. Focus on compound movements that work multiple muscle groups, such as:
- squats
- lunges
- deadlifts
- press-ups
- shoulder presses
- upright rows
- planks
- glute bridges
- sit-ups
- Russian twists
Start with light (e.g. 2-3 kg) weights and maintain proper form.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Don’t Let Menopause Run You Down: 4 Critical Things Female Runners Should Know
Take care!
Share This Post
-
Superfood Kale & Dill Pâté
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most of us could do with eating more greens a lot of the time, but it’s not always easy to include them. This kale and dill pâté brings a healthy dose of green in luxurious style, along with abundant phytochemicals and more!
You will need
- 2 handfuls kale, stalks removed
- 1 cup soft cheese (you can use our Healthy Plant-Based Cream Cheese recipe if you like)
- 2 tbsp fresh dill, chopped
- 1 tsp capers
- 1 tsp black pepper, coarse ground
- ½ tsp MSG, or 1 tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Steam the kale for about 5 minutes or until wilted and soft. Run under cold water to halt the cooking process.
2) Combine all the ingredients, including the kale you just blanched, in a food processor and blitz to make a smooth pâté.
3) Serve with oatcakes or vegetable sticks, or keep in the fridge to enjoy it later:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
Take care!
Share This Post
Related Posts
-
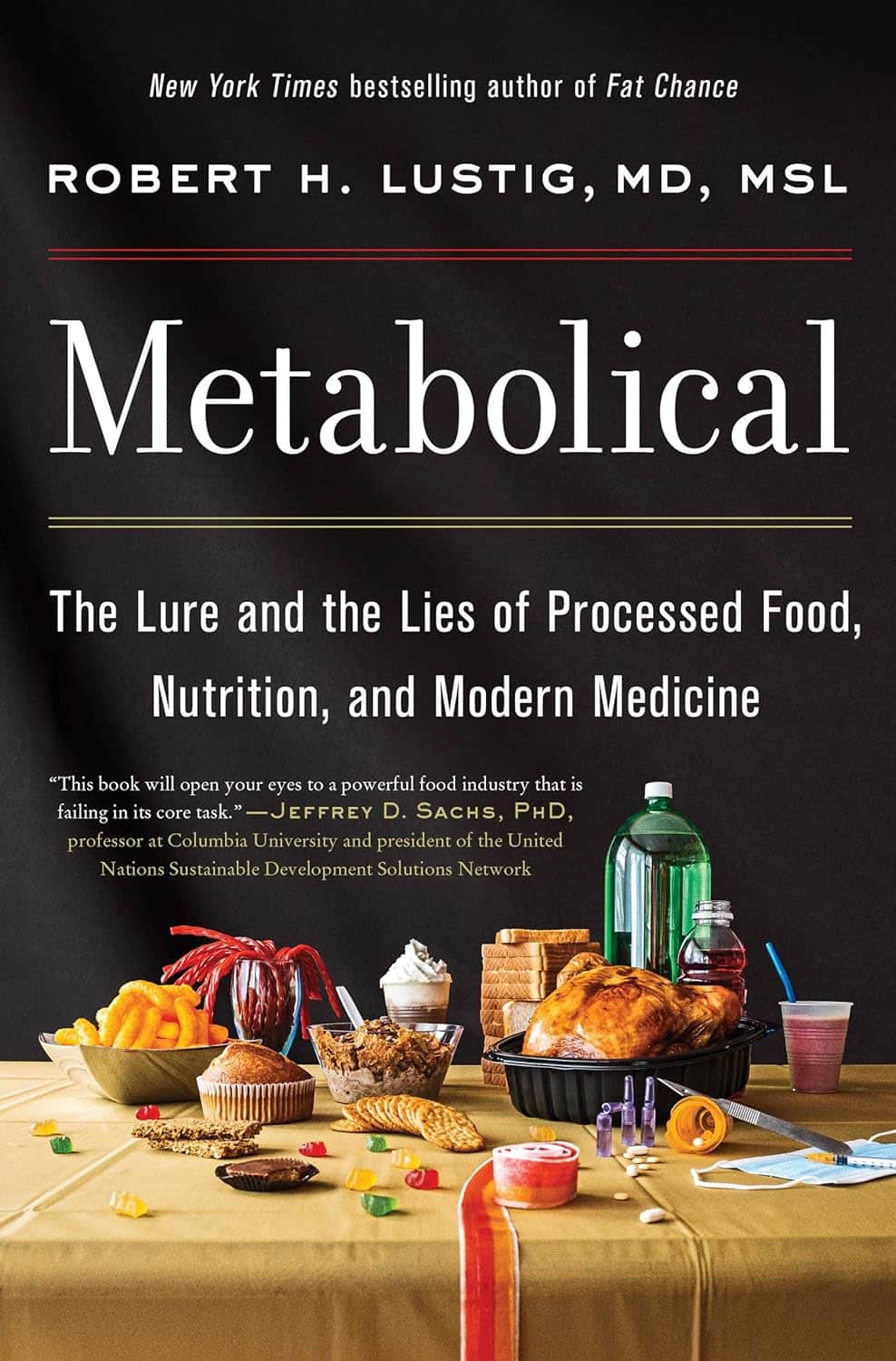
Metabolical – by Dr. Robert Lustig
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The premise of this book itself is not novel: processed food is bad, food giants lie to us, and eating better makes us less prone to disease (especially metabolic disease).
What this book does offer that’s less commonly found is a comprehensive guide, a walkthrough of each relevant what and why and how, with plenty of good science and practical real-world examples.
In terms of unique selling points, perhaps the greatest strength of this book is its focus on two things in particular that affect many aspects of health: looking after our liver, and looking after our gut.
The style is… A little dramatic perhaps, but that’s just the style; there’s no hyperbole, he is stating well-established scientific facts.
Bottom line: very much of chronic disease would be a lot less diseasey if we all ate with these aspects of our health in mind. This book’s a comprehensive guide to that.
Click here to check out Metabolical, and let food be thy medicine!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Winter Wellness & The Pills That Increase Your Alzheimer’s Risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This week in health news…
Do not go gentle into that good night
As wildfires rage in California, snow is falling from Texas to Georgia, meaning that a lot of people are facing weather they’re not accustomed to, in houses that were not built for it. And that’s the lucky ones; there are many thousands of people who are homeless, of whom many will die.
Hopefully all our readers are safe, but it pays to watch out for the signs of hypothermia as it is a condition that really sneaks up on people and, in the process, takes away their ability to notice the hypothermia. You and your loved ones are not immune to this, so it’s good to keep an eye on each other, looking out for:
- Shivering, first ← when this stops, assuming it’s not because the temperature has risen, it is often a sign of hypothermia entering a later stage, in which the body is no longer responding appropriately to the cold
- Slurred speech or mumbling
- Slow, shallow breathing
- A weak pulse
- Clumsiness or lack of coordination
- Drowsiness or very low energy
- Confusion or memory loss
- Loss of consciousness
- In infants, bright red, cold skin
How cold is too cold? It doesn’t even have to be sub-zero. According to the CDC, temperatures of 4℃ (40℉) can be low enough to cause hypothermia.
Read in full: The warning signs to notice if someone has hypothermia
Related: Cold Weather Health Risks
Lethal lottery of pathogens
In Minnesota, hospital emergency room waiting times have skyrocketed since yesterday (at time of writing), with 40% of Minnesota’s 1,763 flu-related hospitalizations this fall and winter occurring in the same week, according to yesterday’s report. To put it further into perspective, 17 out of 20 of this season’s flu outbreaks have occurred in the past two weeks.
And that’s just the flu, without considering COVID, RSV, and Norovirus, which are also all running rampant in MN right now.
The advice presently is:
❝Go to the ER if you are super-sick. If you are not super-sick, go to urgent care, go to your clinic, schedule a virtual appointment.❞
And if you’re not in Minneapolis? These stats won’t apply, but definitely consider, before going to the hospital, whether you might leave sicker than you arrived, and plan accordingly, making use of telehealth where reasonably possible.
Read in full: Minnesota ERs stressed by “quad-demic” of COVID, flu, RSV, norovirus
Related: Move over, COVID and Flu! We Have “Hybrid Viruses” To Contend With Now
Sleep, but at what cost?
This was a study looking at the effects of sleeping pills on the brain, specifically zolpidem (most well-known by its brand name of Ambien).
What they found is that while it does indeed effectively induce sleep, part of how it does that is suppressing norepinephrine oscillations (which might otherwise potentially wake you up, though in healthy people these oscillations and the micro-arousals that they cause shouldn’t disrupt sleep at all, and are just considered part of our normal sleep cycles), which oscillations are necessary to generate the pumping action required to move cerebrospinal fluid through the glymphatic system while asleep.
This is a big problem, because the glymphatic system is almost entirely responsible for keeping the brain free from waste products such as beta-amyloids (whose build-up is associated with Alzheimer’s disease and is considered to be a significant part of Alzheimer’s pathogensesis) and alpha-synuclein (same but for Parkinson’s disease), amongst others:
Read in full: Common sleeping pill may pave way for disorders like Alzheimer’s
Related: How To Clean Your Brain (Glymphatic Health Primer)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Before You Reach For That Tylenol…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, on names: we’ve titled this with “Tylenol” because that’s a well-known brand name, but the drug name is paracetamol or acetaminophen:
- paracetamol is the drug name used by the World Health Organization, and thus also most countries.
- acetaminophen is the drug name used in Canada, Colombia, Iran, Japan, US, and Venezuela.
They are absolutely the same drug.
Firstly, obviously, do avoid overdose
The safe dosage described on the packet is generally accurate (usually around 4g/day, spaced out at 1g per 4 hours), and the dose required for toxicity is generally about 10g, or 200mg/kg body weight, whichever is lower. Since a single dose usually contains 2x 500mg = 1g, that makes overdose all too easy.
The amount required for toxicity can be misleading too, because that’s assuming…
- a healthy liver
- no other health problems
- no other medications that interact or add to the toxicity
- no medications that strain the liver (as with many pro-drugs, and drugs in general that are metabolized by the liver, which is lots).
Which is a lot of assumptions! Especially given that the liver can only process so much at once, meaning that if your liver has a lot of things to do, it can get a backlog, and you think “I’m not taking anything with this painkiller that I shouldn’t” but your liver is still metabolizing the last of last night’s glass of wine and one of your regular medications from this morning, because previously it was still metabolizing things from the day before yesterday, and so on.
See also: How To Regenerate Your Liver ← the liver is an incredible organ that does an amazing job, but it can’t do that if you don’t do this
Please don’t overdose deliberately either. Intentional overdoses make up a very large portion of acetaminophen overdoses (exact figures vary from year to year and place to place, but it’s always high), and what a lot of people doing that don’t realize is:
- it’s a very unpleasant way to die. You’ll take it, you might get some initial symptoms within the first hours or you might not, then you’ll probably feel better, and then the next day or so, you’ll enter the organs-shutting-down stage that usually will take most of a week to kill you slowly and painfully. Often your kidneys will go first but it’ll usually be liver necrosis that deals the final blow.
- it’s very difficult to treat. Stomach-pumping might work if you get it within 1 hour of overdose, and activated charcoal might help if you get it within 2 hours. Acetylcysteine may reduce the toxicity if you get it within the 8–48 hour window (depending on the speed of gastric emptying), but whether or not that will help depends on the severity of the overdose and other factors, so this is not something to bet on. After 48 hours, a liver transplant is the last resort, without which, mortality is around 95%.
Unfortunately, this means that a lot of people who do not intend to die horribly, and hoped to either die peacefully or else be saved, die horribly instead.
Ok, that was not a cheerful topic but it is important, before moving on, we’ll just put this here for anyone it may benefit:
How To Stay Alive (When You Really Don’t Want To) ← this is about suicidality, in yourself or others
Secondly, that dosage is for occasional use only
The problem often starts like this:
❝Due to its perceived safety, paracetamol has long been recommended as the first line drug treatment for osteoarthritis by many treatment guidelines, especially in older people who are at higher risk of drug-related complications❞
People with chronic pain, whether high or low on the pain level of that chronic pain, can very easily get into a habit of “I’ll just take this to take the edge off”, for example when getting up in the morning (often a trigger for pain starting) or going to bed at night (one needs to sleep and the pain is a barrier to that).
But… Those events, getting up and going to bed, it means that taking the drug also becomes part of one’s morning/evening routine—with many people even metering the doses out into pill organizers for the week, with this in mind.
A large (n=582,961) study looked at two groups of people, all aged 65+:
- 180,483 people who had been prescribed paracetamol repeatedly (≥2 prescriptions within six months)
- 402,478 people of the same age who had never been prescribed paracetamol repeatedly
The findings? Bearing in mind that “≥2 prescriptions within six months” is not something generally considered excessive…
❝Acetaminophen use was associated with an increased risk of peptic ulcer bleeding (aHR 1.24; 95% CI 1.16, 1.34), uncomplicated peptic-ulcers (aHR 1.20; 95% CI 1.10, 1.31), lower gastrointestinal-bleeding (aHR 1.36; 95% CI 1.29, 1.46), heart-failure (aHR 1.09; 95% CI 1.06, 1.13), hypertension (aHR 1.07; 95% CI 1.04, 1.11), and chronic kidney disease (aHR 1.19; 95% CI 1.13, 1.24).❞
The researchers concluded:
❝Despite its perceived safety, acetaminophen is associated with several serious complications. Given its minimal analgesic effectiveness, the use of acetaminophen as the first-line oral analgesic for long-term conditions in older people requires careful reconsideration.❞
You can see the study itself here: Incidence of side effects associated with acetaminophen in people aged 65 years or more: a prospective cohort study using data from the Clinical Practice Research Datalink
What to use instead?
It’s been established that taking aspirin regularly isn’t great either:
See: Low-Dose Aspirin & Anemia and Aspirin, CVD Risk, & Potential Counter-Risks
And as for ibuprofen, we don’t have an article about that yet, but it’s gut-unhealthy (harms your microbiome), and besides, anything it can do, ginger can do as well or better (in head-to-head trials; we’re not speaking hyperbolically here):
Ginger Does A Lot More Than You Think ← in fact, it was even found as effective as the combination of acetaminophen, ibuprofen, and caffeine
There are other options though, and as pain is complicated and there’s no one-size-fits-all solution, we’ve compiled the following:
- Dial Down Your Pain
- Stop Pain Spreading
- Managing Chronic Pain (Realistically!)
- The 7 Approaches To Pain Management
- Science-Based Alternative Pain Relief ← when painkillers aren’t helping, these things might
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: