The 7 Approaches To Pain Management
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More Than One Way To Kill Pain
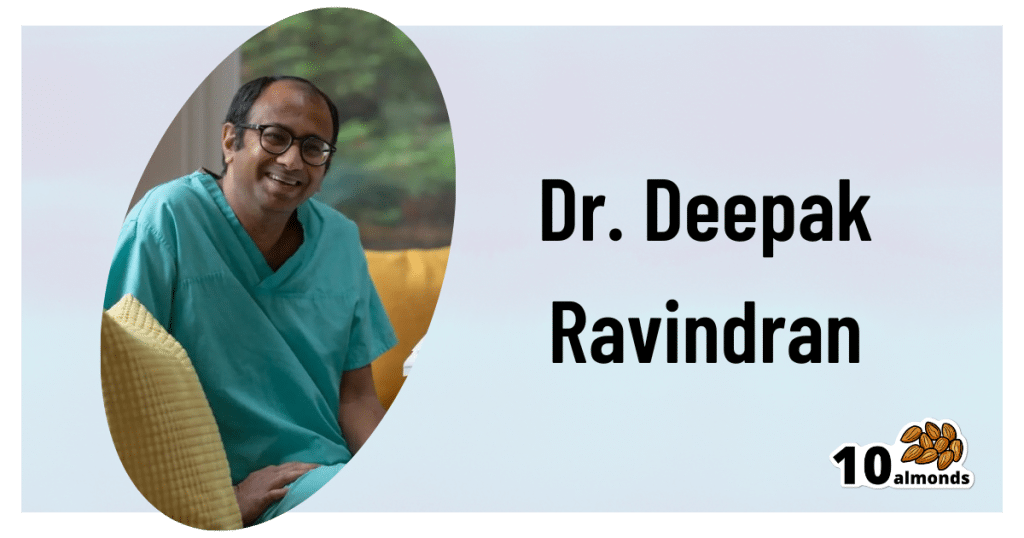
This is Dr. Deepak Ravindran (MD, FRCA. FFPMRCA, EDRA. FIPP, DMSMed). He has decades of experience and is a specialist in acute and chronic pain management, anesthesia, musculoskeletal medicine, and lifestyle medicine.
A quick catch-up, first:
We’ve written about chronic pain management before:
Managing Chronic Pain (Realistically!)
As well as:
Science-Based Alternative Pain Relief
Dr. Ravindran’s approach
Dr. Ravindran takes a “trauma-informed care” approach to his professional practice, and recommends the same for others.
In a nutshell, this means starting from a position of not “what’s wrong with you?”, but rather “what happened to you?”.
This seemingly subtle shift is important, because it means actually dealing with a person’s issues, instead of “take one of these and call my secretary next month”. Read more:
Pain itself can be something of a many-headed hydra. Dr. Ravindran’s approach is equally many-headed; specifically, he has a 7-point plan:
Medications
Dr. Ravindran sees painkillers (and a collection of other drugs, like antidepressants and muscle relaxants) as a potential means to an end worth exploring, but he doesn’t expect them to be the best choice for everyone, and nor does he expect them to be a cure-all. Neither should we. He also advises being mindful of the drawbacks and potential complications of these drugs, too.
Interventions
Sometimes, surgery is the right choice. Sometimes it isn’t. Often, it will change a life—one way or the other. Similar to with medications, Dr. Ravindran is very averse to a “one size fits all” approach here. See also:
The Insider’s Guide To Making Hospital As Comfortable As Possible
Neuroscience and stress management
Often a lot of the distress of pain is not just the pain itself, but the fear associated with it. Will it get worse if I move wrong or eat the wrong thing? How long will it last? Will it ever get better? Will it get worse if I do nothing?. Dr. Ravindran advises tackling this, with the same level of importance as the pain itself. Here’s a good start:
Stress, And Building Psychological Resilience
Diet and the microbiome
Many chronic illnesses are heavily influenced by this, and Dr. Ravindran’s respect for lifestyle medicine comes into play here. While diet might not fix all our ills, it certainly can stop things from being a lot worse. Beyond the obvious “eat healthily” (Mediterranean diet being a good starting point for most people), he also advises doing elimination tests where appropriate, to screen out potential flare-up triggers. You also might consider:
Four Ways To Upgrade The Mediterranean Diet
Sleep
“Get good sleep” is easy advice for those who are not in agonizing pain that sometimes gets worse from staying in the same position for too long. Nevertheless, it is important, and foundational to good health. So it’s important to explore—whatever limitations one might realistically have—what can be done to improve it.
If you can only sleep for a short while at a time, you may get benefit from this previous main feature of ours:
How To Nap Like A Pro (No More “Sleep Hangovers”!)
Exercise and movement
The trick here is to move little and often; without overdoing it, but without permitting loss of mobility either. See also:
The Doctor Who Wants Us To Exercise Less, And Move More
Therapies of the mind and body
This is about taking a holistic approach to one’s wellness. In Dr. Ravindran’s words:
❝Mind-body therapies are often an extremely sensitive topic about which people hold very strong opinions and sometimes irrational beliefs.
Some, like reiki and spiritual therapy and homeopathy, have hardly any scientific evidence to back them up, while others like yoga, hypnosis, and meditation/mindfulness are mainstream techniques with many studies showing the benefits, but they all work for certain patients.❞
In other words: evidence-based is surely the best starting point, but if you feel inclined to try something else and it works for you, then it works for you. And that’s a win.
Want to know more?
You might like his book…
The Pain-Free Mindset: 7 Steps to Taking Control and Overcoming Chronic Pain
He also has a blog and a podcast.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
‘Naked carbs’ and ‘net carbs’ – what are they and should you count them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
According to social media, carbs come in various guises: naked carbs, net carbs, complex carbs and more.
You might be wondering what these terms mean or if all carbs are really the same. If you are into “carb counting” or “cutting carbs”, it’s important to make informed decisions about what you eat.
What are carbs?
Carbohydrates, or “carbs” for short, are one of the main sources of energy we need for brain function, muscle movement, digestion and pretty much everything our bodies do.
There are two classifications of carbs, simple and complex. Simple carbs have one or two sugar molecules, while complex carbs are three or more sugar molecules joined together. For example, table sugar is a simple carb, but starch in potatoes is a complex carb.
All carbs need to be broken down into individual molecules by our digestive enzymes to be absorbed. Digestion of complex carbs is a much slower process than simple carbs, leading to a more gradual blood sugar increase.
Fibre is also considered a complex carb, but it has a structure our body is not capable of digesting. This means we don’t absorb it, but it helps with the movement of our stool and prevents constipation. Our good gut bacteria also love fibre as they can digest it and use it for energy – important for a healthy gut.
What about ‘naked carbs’?
“Naked carbs” is a popular term usually used to refer to foods that are mostly simple carbs, without fibre or accompanying protein or fat. White bread, sugary drinks, jams, sweets, white rice, white flour, crackers and fruit juice are examples of these foods. Ultra-processed foods, where the grains are stripped of their outer layers (including fibre and most nutrients) leaving “refined carbs”, also fall into this category.
One of the problems with naked carbs or refined carbs is they digest and absorb quickly, causing an immediate rise in blood sugar. This is followed by a rapid spike in insulin (a hormone that signals cells to remove sugar from blood) and then a drop in blood sugar. This can lead to hunger and cravings – a vicious cycle that only gets worse with eating more of the same foods.
Naked carbs can make blood sugars spike then crash.
Pexels/Alexander GreyWhat about ‘net carbs’?
This is another popular term tossed around in dieting discussions. Net carbs refer to the part of the carb food that we actually absorb.
Again, fibre is not easily digestible. And some carb-rich foods contain sugar alcohols, such as sweeteners (like xylitol and sorbitol) that have limited absorption and little to no effect on blood sugar. Deducting the value of fibre and sugar alcohols from the total carbohydrate content of a food gives what’s considered its net carb value.
For example, canned pear in juice has around 12.3g of “total carbohydrates” per 100g, including 1.7g carb + 1.7g fibre + 1.9g sugar alcohol. So its net carb is 12.3g – 1.7g – 1.9g = 8.7g. This means 8.7g of the 12.3g total carbs impacts blood sugar.
The nutrition labels on packaged foods in Australia and New Zealand usually list fibre separately to carbohydrates, so the net carbs have already been calculated. This is not the case in other countries, where “total carbohydrates” are listed.
Does it matter though?
Whether or not you should care about net or naked carbs depends on your dietary preferences, health goals, food accessibility and overall nutritional needs. Generally speaking, we should try to limit our consumption of simple and refined carbs.
The latest World Health Organization guidelines recommend our carbohydrate intake should ideally come primarily from whole grains, vegetables, fruits and pulses, which are rich in complex carbs and fibre. This can have significant health benefits (to regulate hunger, improve cholesterol or help with weight management) and reduce the risk of conditions such as heart disease, obesity and colon cancer.
In moderation, naked carbs aren’t necessarily bad. But pairing them with fats, protein or fibre can slow down the digestion and absorption of sugar. This can help to stabilise blood sugar levels, prevent spikes and crashes and support personal weight management goals. If you’re managing diabetes or insulin resistance, paying attention to the composition of your meals, and the quality of your carbohydrate sources is essential.
A ketogenic (high fat, low carb) diet typically restricts carb intake to between 20 and 50g each day. But this carb amount refers to net carbs – so it is possible to eat more carbs from high-fibre sources.
Choose complex carbohydrates with lots of fibre.
ShutterstockSome tips to try
Some simple strategies can help you get the most out of your carb intake:
reduce your intake of naked carbs and foods high in sugar and white flour, such as white bread, table sugar, honey, lollies, maple syrup, jam, and fruit juice
opt for protein- and fibre-rich carbs. These include oats, sweet potatoes, nuts, avocados, beans, whole grains and broccoli
if you are eating naked carbs, dress them up with some protein, fat and fibre. For example, top white bread with a nut butter rather than jam
if you are trying to reduce the carb content in your diet, be wary of any symptoms of low blood glucose, including headaches, nausea, and dizziness
- working with a health-care professional such as an accredited practising dietitian or your GP can help develop an individualised diet plan that meets your specific needs and goals.
Correction: this article has been updated to indicate how carbohydrates are listed on food nutrition labels in Australia and New Zealand.
Saman Khalesi, Senior Lecturer and Discipline Lead in Nutrition, School of Health, Medical and Applied Sciences, CQUniversity Australia; Anna Balzer, Lecturer, Medical Science School of Health, Medical and Applied Sciences, CQUniversity Australia; Charlotte Gupta, Postdoctoral research fellow, CQUniversity Australia; Chris Irwin, Senior Lecturer in Nutrition and Dietetics, School of Health Sciences & Social Work, Griffith University, and Grace Vincent, Senior Lecturer, Appleton Institute, CQUniversity Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Are You Stuck Playing These Three Roles in Love?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The psychology of Transactional Analysis holds that our interpersonal dynamics can be modelled in the following fashion:
The roles
- Child: vulnerable, trusting, weak, and support-seeking
- Parent: strong, dominant, responsible—but also often exhausted and critical
- Adult: balanced, thoughtful, creative, and kind
Ideally we’d be able to spend most of our time in “Adult” mode, and occasionally go into “Child” or “Parent” mode when required, e.g. child when circumstances have rendered us vulnerable and we need help; parent when we need to go “above and beyond” in the pursuit of looking after others. That’s all well and good and healthy.
However, in relationships, often it happens that partners polarize themselves and/or each other, with one shouldering all of the responsibility, and the other willfully losing their own agency.
The problem lies in that either role can be seductive—on the one hand, it’s nice to be admired and powerful and it’s a good feeling to look after one’s partner; on the other hand, it’s nice to have someone who will meet your every need. What love and trust!
Only, it becomes toxic when these roles stagnate, and each forgets how to step out of them. Each can become resentful of the other (for not pulling their weight, on one side, and for not being able to effortlessly solve all life problems unilaterally and provide endlessly in both time and substance, on the other), digging in to their own side and exacerbating the less healthy qualities.
As to the way out? It’s about self-exploration and mutual honesty—and mutual support:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
While we haven’t (before today) written about TA per se, we have previously written about AT (Attachment Theory), and on this matter, the two can overlap, where certain attachment styles can result in recreating parent/child/adult dynamics:
How To Leverage Attachment Theory In Your Relationship ← this is about understanding and recognizing attachment styles, and then making sure that both you and your partner(s) are armed with the necessary knowledge and understanding to meet each other’s needs.
Take care!
Share This Post
-
How White Is Your Tongue?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝So its normal to develop a white sort of coating on the tongue, right? It develops when I eat, and is able to (somewhat) easily be brushed off❞
If (and only if) there is no soreness and the coverage of the whiteness is not extreme, then, yes, that is normal and fine.
Your mouth has a microbiome, and it’s supposed to have one (helps keep the conditions in your mouth correct, so that food is broken down and/but your gums and teeth aren’t).
Read more: The oral microbiome: Role of key organisms and complex networks in oral health and disease
The whiteness you often see on a healthy tongue is, for the most part, bacteria and dead cells—harmless.
Cleaning the whiteness off with your brush is fine. You can also scrape off with floss is similar if you prefer. Or a tongue-scraper! Those can be especially good for people for whom brushing the tongue is an unpleasant sensation. Or you can just leave it, if it doesn’t bother you.
By the way, that microbiome is a reason it can be good to go easy on the mouthwash. Moderate use of mouthwash is usually fine, but you don’t want to wipe out your microbiome then have it taken over by unpleasantries that the mouthwash didn’t kill (unpleasantries like C. albicans).
There are other mouthwash-related considerations too:
Toothpastes and mouthwashes: which kinds help, and which kinds harm?
If you start to get soreness, that probably means the papillae (little villi-like things) are inflamed. If there is soreness, and/or the whiteness is extreme, then it could be a fungal infection (usually C. albicans, also called Thrush), in which case, antifungal medications will be needed, which you can probably get over the counter from your pharmacist.
Do not try to self-treat with antibiotics.
Antibiotics will make a fungal infection worse (indeed, antibiotic usage is often the reason for getting fungal growth in the first place) by wiping out the bacteria that normally keep it in check.
Other risk factors include a sugary diet, smoking, and medications that have “dry mouth” as a side effect.
Read more: Can oral thrush be prevented?
If you have any symptoms more exciting than the above, then definitely see a doctor.
Take care!
Share This Post
Related Posts
-
Stevia vs Acesulfame Potassium – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing stevia to acesulfame potassium, we picked the stevia.
Why?
You may be wondering: is acesulfame potassium a good source of potassium?
And the answer is: no, it is not. Obviously, it does contain potassium, but let’s do some math here:
- Acesulfame potassium is 200x sweeter than sugar
- Therefore replacing a 15g teaspoon of sugar = 75mg acesulfame potassium
- Acesulfame potassium’s full name is “potassium 6-methyl-2,2-dioxo-2H-1,2λ6,3-oxathiazin-4-olate”
- That’s just one potassium atom in there with a lot of other stuff
- Acesulfame potassium has a molar mass of 201.042 g/mol
- Potassium itself has a molar mass of 39.098 g/mol
- Therefore acesulfame potassium is 100(39.098/201.042) = 19.45% potassium by mass
- So that 75mg of acesulfame potassium contains just under 15mg of potassium, which is less than 0.5% of your recommended daily amount of potassium. Please consider eating a fruit instead.
So, that’s that, and the rest of the nutritional values of both sweeteners are just a lot of zeros.
What puts stevia ahead? Simply, based on studies available so far, moderate consumption of stevia improves gut microdiversity, whereas acesulfame potassium harms gut microdiversity:
- The Effects of Stevia Consumption on Gut Bacteria: Friend or Foe?
- The Artificial Sweetener Acesulfame Potassium Affects the Gut Microbiome
Want to give stevia a try?
Here’s an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Without Medicare Part B’s Shield, Patient’s Family Owes $81,000 for a Single Air-Ambulance Flight
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Without Medicare Part B’s Shield, Patient’s Family Owes $81,000 for a Single Air-Ambulance Flight
Debra Prichard was a retired factory worker who was careful with her money, including what she spent on medical care, said her daughter, Alicia Wieberg. “She was the kind of person who didn’t go to the doctor for anything.”
That ended last year, when the rural Tennessee resident suffered a devastating stroke and several aneurysms. She twice was rushed from her local hospital to Vanderbilt University Medical Center in Nashville, 79 miles away, where she was treated by brain specialists. She died Oct. 31 at age 70.
One of Prichard’s trips to the Nashville hospital was via helicopter ambulance. Wieberg said she had heard such flights could be pricey, but she didn’t realize how extraordinary the charge would be — or how her mother’s skimping on Medicare coverage could leave the family on the hook.
Then the bill came.
The Patient: Debra Prichard, who had Medicare Part A insurance before she died.
Medical Service: An air-ambulance flight to Vanderbilt University Medical Center.
Service Provider: Med-Trans Corp., a medical transportation service that is part of Global Medical Response, an industry giant backed by private equity investors. The larger company operates in all 50 states and says it has a total of 498 helicopters and airplanes.
Total Bill: $81,739.40, none of which was covered by insurance.
What Gives: Sky-high bills from air-ambulance providers have sparked complaints and federal action in recent years.
For patients with private insurance coverage, the No Surprises Act, which went into effect in 2022, bars air-ambulance companies from billing people more than they would pay if the service were considered “in-network” with their health insurers. For patients with public coverage, such as Medicare or Medicaid, the government sets payment rates at much lower levels than the companies charge.
But Prichard had opted out of the portion of Medicare that covers ambulance services.
That meant when the bill arrived less than two weeks after her death, her estate was expected to pay the full air-ambulance fee of nearly $82,000. The main assets are 12 acres of land and her home in Decherd, Tennessee, where she lived for 48 years and raised two children. The bill for a single helicopter ride could eat up roughly a third of the estate’s value, said Wieberg, who is executor.
The family’s predicament stems from the complicated nature of Medicare coverage.
Prichard was enrolled only in Medicare Part A, which is free to most Americans 65 or older. That section of the federal insurance program covers inpatient care, and it paid most of her hospital bills, her daughter said.
But Prichard declined other Medicare coverage, including Part B, which handles such things as doctor visits, outpatient treatment, and ambulance rides. Her daughter suspects she skipped that coverage to avoid the premiums most recipients pay, which currently are about $175 a month.
Loren Adler, a health economist for the Brookings Institution who studies ambulance bills, estimated the maximum charge that Medicare would have allowed for Prichard’s flight would have been less than $10,000 if she’d signed up for Part B. The patient’s share of that would have been less than $2,000. Her estate might have owed nothing if she’d also purchased supplemental “Medigap” coverage, as many Medicare members do to cover things like coinsurance, he said.
Nicole Michel, a spokesperson for Global Medical Response, the ambulance provider, agreed with Adler’s estimate that Medicare would have limited the charge for the flight to less than $10,000. But she said the federal program’s payment rates don’t cover the cost of providing air-ambulance services.
“Our patient advocacy team is actively engaged with Ms. Wieberg’s attorney to determine if there was any other applicable medical coverage on the date of service that we could bill to,” Michel wrote in an email to KFF Health News. “If not, we are fully committed to working with Ms. Wieberg, as we do with all our patients, to find an equitable solution.”
The Resolution: In mid-February, Wieberg said the company had not offered to reduce the bill.
Wieberg said she and the attorney handling her mother’s estate both contacted the company, seeking a reduction in the bill. She said she also contacted Medicare officials, filled out a form on the No Surprises Act website, and filed a complaint with Tennessee regulators who oversee ambulance services. She said she was notified Feb. 12 that the company filed a legal claim against the estate for the entire amount.
Wieberg said other health care providers, including ground ambulance services and the Vanderbilt hospital, wound up waiving several thousand dollars in unpaid fees for services they provided to Prichard that are normally covered by Medicare Part B.
But as it stands, Prichard’s estate owes about $81,740 to the air-ambulance company.
More from Bill of the Month
- The Colonoscopies Were Free. But the ‘Surgical Trays’ Came With $600 Price Tags. Jan 25, 2024
- When a Quick Telehealth Visit Yields Multiple Surprises Beyond a Big Bill Dec 19, 2023
- Out for Blood? For Routine Lab Work, the Hospital Billed Her $2,400 Nov 21, 2023
The Takeaway: People who are eligible for Medicare are encouraged to sign up for Part B, unless they have private health insurance through an employer or spouse.
“If someone with Medicare finds that they are having difficulty paying the Medicare Part B premiums, there are resources available to help compare Medicare coverage choices and learn about options to help pay for Medicare costs,” Meena Seshamani, director of the federal Center for Medicare, said in an email to KFF Health News.
She noted that every state offers free counseling to help people navigate Medicare.
In Tennessee, that counseling is offered by the State Health Insurance Assistance Program. Its director, Lori Galbreath, told KFF Health News she wishes more seniors would discuss their health coverage options with trained counselors like hers.
“Every Medicare recipient’s experience is different,” she said. “We can look at their different situations and give them an unbiased view of what their next best steps could be.”
Counselors advise that many people with modest incomes enroll in a Medicare Savings Program, which can cover their Part B premiums. In 2023, Tennessee residents could qualify for such assistance if they made less than $1,660 monthly as a single person or $2,239 as a married couple. Many people also could obtain help with other out-of-pocket expenses, such as copays for medical services.
Wieberg, who lives in Missouri, has been preparing the family home for sale.
She said the struggle over her mother’s air-ambulance bill makes her wonder why Medicare is split into pieces, with free coverage for inpatient care under Part A, but premiums for coverage of other crucial services under Part B.
“Anybody past the age of 70 is likely going to need both,” she said. “And so why make it a decision of what you can afford or not afford, or what you think you’re going to use or not use?”
Bill of the Month is a crowdsourced investigation by KFF Health News and NPR that dissects and explains medical bills. Do you have an interesting medical bill you want to share with us? Tell us about it!
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
High-Octane Brain – by Dr. Michelle Braun
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
True to the title, Dr. Braun jumps straight into action here, making everything as practical as possible as quickly as possible and giving the most attention to the science-based steps to take. Thereafter, and almost as an addendum, she gives examples of “brain role models” from various age groups, to show how these things can be implemented and benefitted-from in the real world.
The greatest strength of this book is that it is the product of a lot of hard science made easy; this book has hundreds of scientific references (of which, many RCTs etc), and many contributions from other professionals in her field, to make one of the most evidence-based guidebooks around, and all presented in one place and in a manner that is perfectly readable to the layperson.
The style, thus, is easy-reading, with references for those who want to jump into further reading but without that being required for applying the advice within.
Bottom line: if you’d like to improve your brain with an evidence-based health regiment and minimal fluff, this is the book for you.
Click here to check out High-Octane Brain, and level-up yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: