Plant-Based Healthy Cream Cheese
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cream cheese is a delicious food, and having a plant-based diet isn’t a reason to miss out. Here we have a protein-forward nuts-based cream cheese that we’re sure you’ll love (unless you’re allergic to nuts, in which case, maybe skip this one).
You will need
- 1½ cups raw cashews, soaked in warm water and then drained
- ½ cup water
- ½ cup coconut cream
- Juice of ½ lemon
- 3 tbsp nutritional yeast
- ½ tsp onion powder
- ½ tsp garlic powder
- ½ tsp black pepper
- ½ tsp cayenne pepper
- ¼ tsp MSG, or ½ tsp low-sodium salt
- Optional: ⅓ cup fresh basil
Method
(we suggest you read everything at least once before doing anything)
1) Blend all of the ingredients until creamy.
2) Optional: leave on the countertop, covered, for 1–2 hours, if you want a more fermented (effectively: cheesy) taste.
3) Refrigerate, ideally overnight, before serving. Serving on bagels is a classic, but you can also enjoy with the Healthy Homemade Flatbreads we made yesterday

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Pistachios vs Cashews – Which is Healthier? ← Pistachios actually won here, but cashews are also great and are better (from a culinary perspective) for making cream cheese
- Why You Should Diversify Your Nuts!
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Nature Provides Us With A Surprisingly Powerful Painkiller
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s well-known (at least to regular 10almonds-readers) that seeing nature, ideally green leaves and blue sky, improves our mood by stimulating production of serotonin.
See also: Neurotransmitter Cheatsheet
But it does a lot more.
Reducing the actual signals of pain
Researchers at the University of Vienna have discovered that viewing nature scenes (even if just on video) alleviates physical pain—not just in self-reported subjective assessments, but also by a reduction of the neural activity that signals pain:
❝Pain is like a puzzle, made up of different pieces that are processed differently in the brain. Some pieces of the puzzle relate to our emotional response to pain, such as how unpleasant we find it. Other pieces correspond to the physical signals underlying the painful experience, such as its location in the body and its intensity.
Unlike placebos, which usually change our emotional response to pain, viewing nature changed how the brain processed early, raw sensory signals of pain.
Thus, the effect appears to be less influenced by participants’ expectations, and more by changes in the underlying pain signals❞
This was tested against, varyingly, viewing an urban environment or viewing an indoor environment, neither of which gave the same benefits.
The setup of the experiment is relevant, so…
Matching soundscape accompanied each visual stimulus. The three pain runs had a total duration of 9 min each, during which one environment was accompanied by 16 painful and 16 non-painful shocks. Neuroimaging was used for all parts, and participants were exposed to all environments:
- First, a cue indicating the intensity of the next shock (red = painful, yellow = not painful) was presented for 2000 milliseconds (ms).
- Second, a variable interval of 3500 ± 1500 ms was shown.
- Third, a cue indicating the intensity of the shock was presented for 1000 ms, accompanied by an electrical shock with a duration of 500 ms.
- Fourth, a variable interval of 3500 ± 1500 ms followed.
- Fifth, after each third trial, participants rated the shock’s intensity and unpleasantness at 6000 ms each.
- Sixth, each trial ended with an intertrial interval (ITI) presented for 2000 ms.
They found that as well as the self-assessment reports being as expected (nature scenes reduced subjective experience of pain),
❝In summary, the multivoxel and region of interest analyses converged in showing that pain responses when exposed to nature as compared to urban or indoor stimuli were associated with a decrease in neural processes related to lower-level nociception-related features (NPS, thalamus), as well as in regions of descending modulatory circuitry associated with attentional alterations of pain that also encode sensory-discriminative aspects (S2, pINS).❞
In other words—to the extent that pain can be quantified objectively by neural imaging—the pain was also objectively reduced, much like with a chemical painkiller.
You can read the paper in full, here:
Nature exposure induces analgesic effects by acting on nociception-related neural processing
How to benefit from this
Well, first there is the obvious, “view nature“.
However, note the timescales involved in the testing periods: 2000 milliseconds is two seconds, and that was the intertrial interval used—the equivalent of a washout phase in an interventional trial (but a drug/supplement/diet washout is usually a number of weeks).
The fact that the test periods were a matter of seconds, and the intertrial period was also literally two seconds, this means:
It works quickly, and the effect disappears quickly, too.
In other words: if you want pain relief from nature, the good news is you can get it immediately while viewing nature, and the bad news is that you have to keep viewing nature to continue enjoying the painkilling effect.
So that’s a limitation, but it’s still clearly a very worthy option for a little respite from chronic pain now and again, for example.
Want to learn more?
We’ve written quite a bit about pain management, including:
- Before You Reach For That Tylenol…
- How To Stop Pain Spreading
- How To Dial Down Your Pain
- Managing Chronic Pain (Realistically!)
- Get The Right Help For Your Pain
- The 7 Approaches To Pain Management
- Science-Based Alternative Pain Relief (When Painkillers Aren’t Helping, These Things Might)
Take care!
Share This Post
-
Four Habits That Drastically Improve Mobility
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mobility is critical for health living, but stretching isn’t the entire story:
Beyond just stretching
Liv Townsend, of LivInLeggings fames, recommends these four habits:
- Sit less: prolonged sitting affects hip and shoulder mobility. Specifically, it affects it negatively. It is also a bringer of woe in many other ways beyond the scope of what we’re doing here today, but the important thing for mobility is to sit less. So, if you spent a lot of time at a desk, invest in a standing desk (writer’s note: I dearly love mine, which is technically a sit-stand converter like this one on Amazon but I just keep it in the up position all the time, so it’s easy to forget it has multiple settings. Anyway, it’s sooooooo much better for my back than sitting for hours at a time.). For how to deal with other (i.e. not desk-related) reasons you might be sitting a lot, check out: Stand Up For Your Health (Or Don’t*)
- Take creatine: more than just for strength and muscle-building (and even aside from its brain-benefits that it bestows to older people, but not young ones), creatine also supports mobility and flexibility. Any brand is fine, so long as creatine monohydrate is the sole ingredient. Also, micronized or not is also fine—that’s just to do with whether it’s been pre-compacted into super-tiny beads (so small that it will still effectively be a powder), which helps it to avoid clumping when mixed in a liquid, that’s all. It shouldn’t have any additives either way (so, check labels to ensure it doesn’t).
- Spend more time under tension: no, we’re not talking about texting your spouse “we need to talk”, but rather, this means that when we do stretch, we should spend longer in the stretched position. While dynamic stretching has its place, passive stretching (holding stretches for longer periods) is essential and shouldn’t be overlooked.
- Incorporate “movement snacks”: this is about when we are going about our daily life, we should move more while doing everyday tasks. Get in some shoulder stretches while waiting for the kettle to boil, deep squat while petting the dog, etc. These are very important, because mobility is very much a “use it or lose it” thing, and so moving in many different ways, frequently, is the only way to ensure full coverage (no stretching regimen is going to be able to cover the many compound movements that we do in everyday life).
*That article also covers how to avoid the damage of sitting even if you cannot physically stand!
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Mobility As Though A Sporting Pursuit: Train For The Event Of Your Life!
Take care!
Share This Post
-
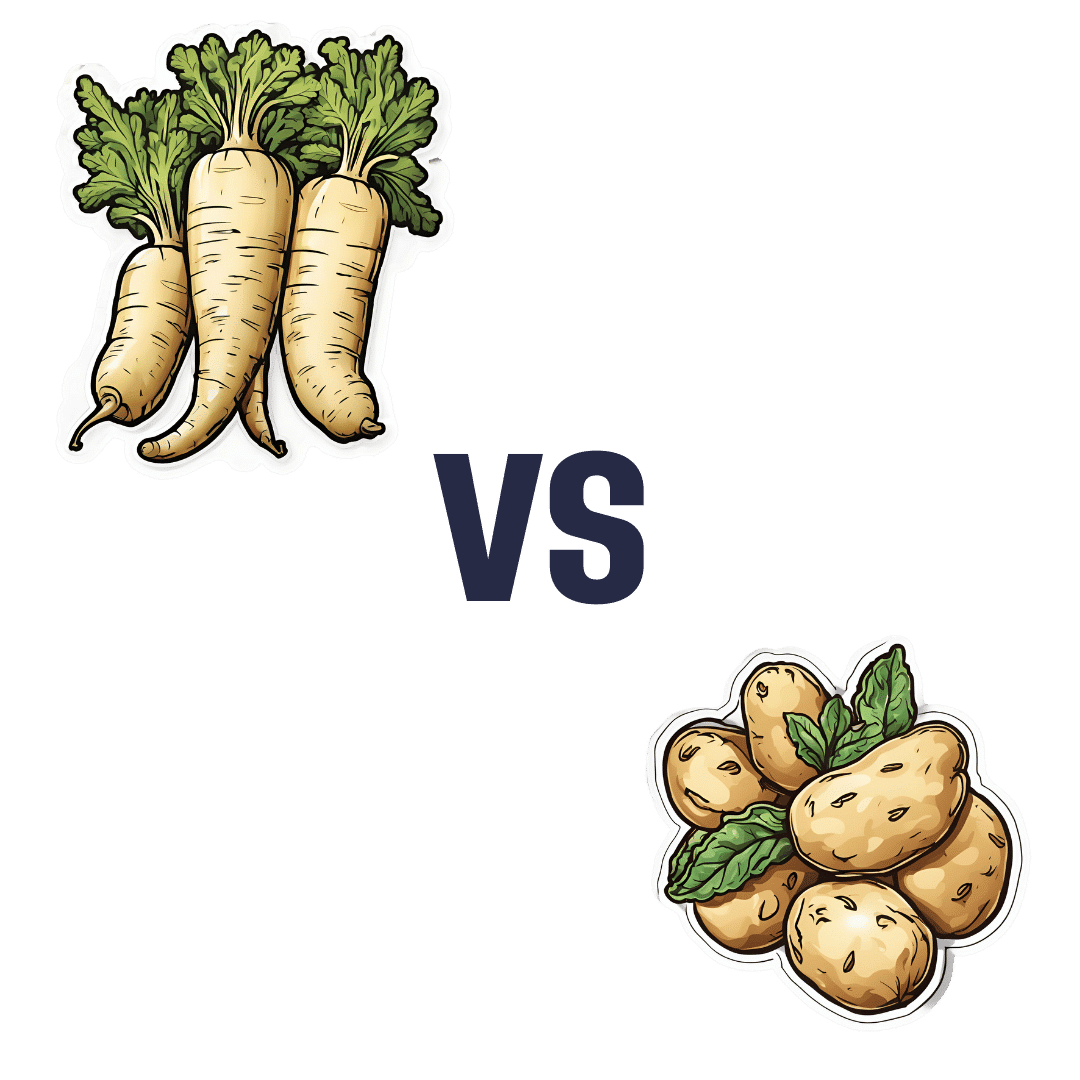
Parsnips vs Potatoes – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing parsnips to potatoes, we picked the parsnips.
Why?
To be more specific, we’re looking at russet potatoes, and in both cases we’re looking at cooked without fat or salt, skin on. In other words, the basic nutritional values of these plants in edible form, without adding anything. With this in mind, once we get to the root of things, there’s a clear winner:
Looking at the macros first, potatoes have more carbs while parsnips have more fiber. Potatoes do have more protein too, but given the small numbers involved when it comes to protein we don’t think this is enough of a plus to outweigh the extra fiber in the parsnips.
In the category of vitamins, again a champion emerges: parsnips have more of vitamins B1, B2, B5, B9, C, E, and K, while potatoes have more of vitamins B3, B6, and choline. So, a 7:3 win for parsnips.
When it comes to minerals, parsnips have more calcium copper, manganese, selenium, and zinc, while potatoes have more iron and potassium. Potatoes do also have more sodium, but for most people most of the time, this is not a plus, healthwise. Disregarding the sodium, this category sees a 5:2 win for parsnips.
In short: as with most starchy vegetables, enjoy both in moderation if you feel so inclined, but if you’re picking one, then parsnips are the nutritionally best choice here.
Want to learn more?
You might like to read:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Should You Go Light Or Heavy On Carbs?
Take care!
Share This Post
Related Posts
-
Natto, Taurine + Black Pepper, And Other Game-Changers
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Loved the info on nuts; of course I always eat pecans, which didn’t make the list of healthy nuts!❞
Dear subscriber, pardon the paraphrase of your comment—somehow it got deleted and now exists only in this writer’s memory. However, to address it:
Pecans are great too! We can’t include everything in every article (indeed, we got another feedback the same day saying the article was too long), but we love when you come to us with stuff for us to look at and write about (seriously, writer here: the more you ask, the easier it makes my job), so let’s talk pecans for a moment:
Pecans would have been number six on our list if we’d have written more!
Like many nuts, they’ve an abundance of healthy fats, fiber, vitamins, and minerals.
They’re particularly good for zinc, which is vital for immune function, healing (including normal recovery after normal exercise), and DNA synthesis (so: anti-aging).
Pecans are also great for reducing LDL (“bad” cholesterol) and triglycerides (which are also bad for heart health); check it out:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Here’s how to help protect babies and kids from RSV
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- RSV is a respiratory virus that is especially dangerous for babies and young children.
- There are two ways to help protect babies from RSV: vaccination during pregnancy and giving babies nirsevimab, an RSV antibody shot.
- If someone in your household has RSV, watch for signs of severe illness and take steps to help prevent it from spreading.
Respiratory syncytial virus, or RSV, is a very contagious seasonal respiratory illness that is especially dangerous for infants and young children. Cases rose dramatically last month, and an increasing number of kids and older adults with RSV are being hospitalized across the United States.
Fortunately, pregnant people can get vaccinated during pregnancy or get their infants and young children an RSV antibody shot to help them stay healthy.
Read on to learn about symptoms of RSV, how to help prevent infants and children from getting very sick, and what families should do if someone in their household is sick with the virus.
What are the symptoms of RSV in babies and young children?
RSV symptoms in young children may include a runny nose, decreased eating and drinking, and coughing, which may lead to wheezing and difficulty breathing.
Infants with RSV may show symptoms like irritability, decreased activity and appetite, and life-threatening pauses in breathing (apnea) that last for more than 10 seconds. Most infants with RSV will not develop a fever, but babies who are born prematurely, have weakened immune systems, or have chronic lung disease are more likely to become very sick.
Who is eligible for an RSV antibody shot?
The Centers for Disease Control and Prevention recommends that babies younger than 8 months whose gestational parent did not receive an RSV vaccine during pregnancy receive nirsevimab between October and March, when RSV typically peaks. This antibody shot delivers proteins that can help protect them against RSV.
Nirsevimab is also recommended for children between 8 and 19 months who are at increased risk of severe RSV, including children who are born prematurely, have chronic lung disease or severe cystic fibrosis, are immunocompromised, or are American Indians or Alaska Natives.
Nirsevimab is typically covered by insurance or costs $495 out of pocket. Children who are eligible for the CDC’s Vaccines for Children Program can receive nirsevimab at no cost.
How can families help prevent RSV from spreading?
It’s recommended that children and adults who are sick with RSV stay home and away from others. If your infant or child has difficulty breathing or develops blue or gray skin, take them to an emergency room right away.
People who are infected with RSV can spread the disease when they cough or sneeze; have close contact with others; or touch, cough, or sneeze on shared surfaces. Help protect your family from catching and spreading RSV at home and in public places by ensuring that everyone covers their mouths during coughing and sneezing, washes their hands often, and wears a high-quality, well-fitting mask.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Being Mortal – by Dr. Atul Gawande
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Maybe you want to “live forever or die trying”, and that’s an understandable goal… But are you prepared for “or die trying” being the outcome?
This is not a cheerful book, if you’re anything like this reviewer, you will need a little towel or something to mop up the tears while you read. But it’s worth it.
Dying is one thing; fighting for life is even generally considered a noble endeavor. Suffering alone isn’t fun, losing independence can feel humiliating, and seeing someone who was always a tower of strength, now a frail shadow of their former self, reduced to begging for something that they’re “not allowed”, can be worse.
Do we want that for ourselves? For our loved ones? Can there be a happy medium between that, and the alternative to indeed “go gentle into that good night”?
Dr. Gawande, a surgeon well-acquainted with death and dying, thinks so. But it involves work on our part, and being prepared for hard decisions.
- What is most important to us, and what tradeoffs are we willing to make for it?
- What, even, is actually an option to us with the resources available?
- Can we make peace with a potentially bad lot? And… Should we?
- When is fighting important, and when is it self-destructive?
These (and others) are all difficult questions posed by Dr. Gawande, but critical ones.
We don’t usually quote other people’s reviews when reviewing books here, but let’s consider the following words from the end of a long review on Amazon:
❝If “dying as we lived” is some kind of standard for how we should go, then maybe alone and medicalized makes some sense right now after all.❞
Bottom line: we all deserve better than that. And if we don’t take the time to think about what’s most important, then time will take it from us. This very insightful book may not have all the answers, but it has the questions, and it can help a lot in exploring them and deciding what matters most to us in the end, really.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: