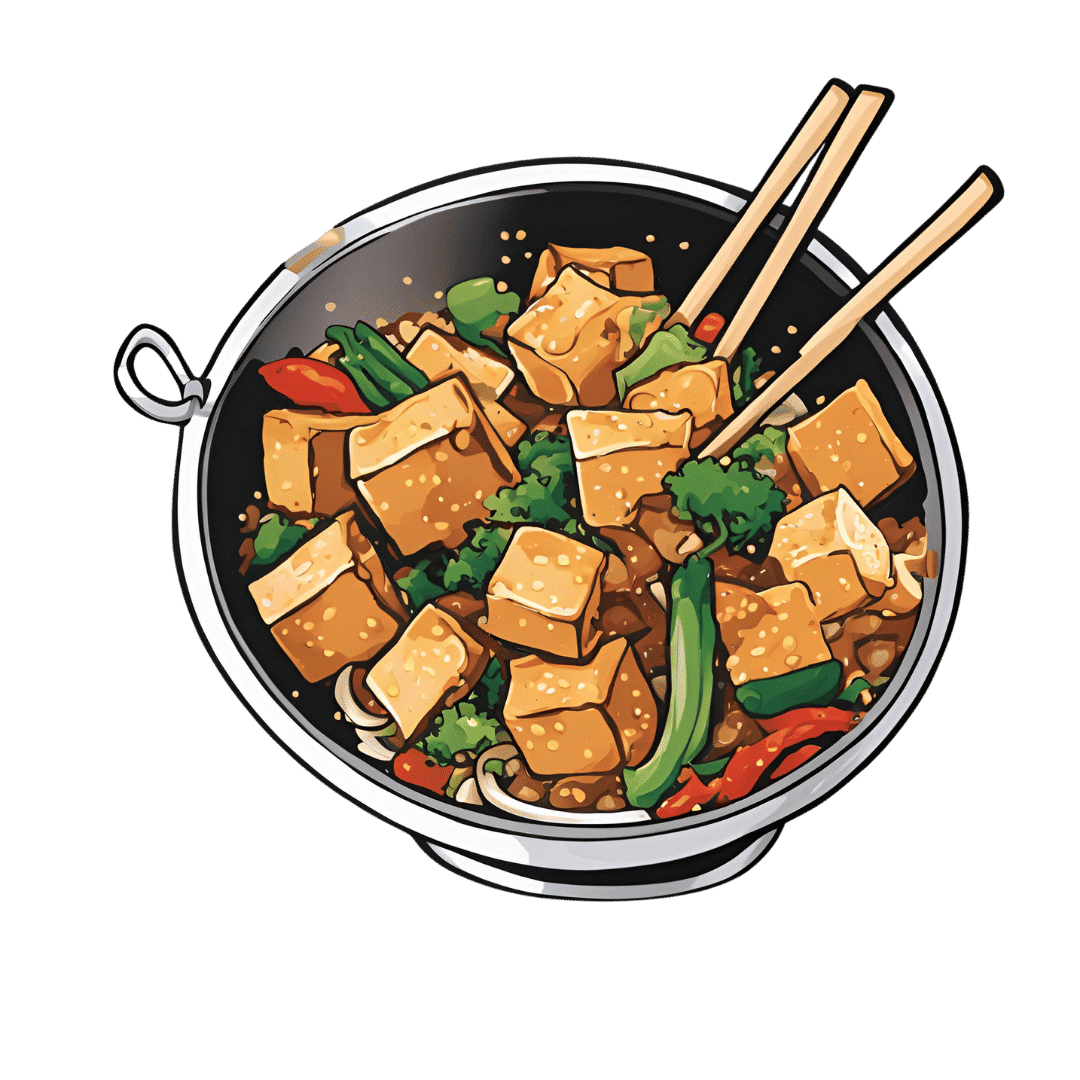
Sesame & Peanut Tofu
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Yesterday we learned how to elevate tofu from “nutrition” to “nutritious tasty snack” with our Basic Baked Tofu recipe; today we’re expanding on that, to take it from “nutritious tasty snack” to “very respectable meal”.
You will need
For the tofu:
- The Basic Baked Tofu that we made yesterday (consider making this to be “step zero” of today’s recipe if you don’t already have a portion in the fridge)
For the sauce:
- ⅓ cup peanut butter, ideally with no added sugar or salt (if allergic to peanuts specifically, use almond butter; if allergic to nuts generally, use tahini)
- ¼ bulb garlic, grated or crushed
- 1 tbsp tamarind paste
- 1½ tbsp tamari sauce (or low-sodium soy sauce, if a substitution is necessary)
- 1 tbsp sambal oelek (or sriracha sauce, if a substitution is necessary)
- 1 tsp ground coriander
- 1 tsp ground black pepper
- ½ tsp ground sweet cinnamon
- ½ tsp MSG (or else omit; do not substitute with salt in this case unless you have a particular craving)
- zest of 1 lime
For the vegetables:
- 14 oz broccolini / tenderstem broccoli, thick ends trimmed (failing that, any broccoli)
- 6 oz shelled edamame
- 1½ tsp toasted sesame oil
For serving:
- 4 cups cooked rice (we recommend our Tasty Versatile Rice recipe)
- ½ cup raw cashews, soaked in hot water for at least 5 minutes and then drained (if allergic, substitute cooked chickpeas, rinsed and drained)
- 1 tbsp toasted sesame seeds
- 1 handful chopped cilantro, unless you have the “this tastes like soap” gene, in which case substitute chopped parsley
Method
(we suggest you read everything at least once before doing anything)
1) Combine the sauce ingredients in a bowl and whisk well (or use a blender if you have one that’s comfortable with this relatively small quantity of ingredients). Taste it, and adjust the ingredient ratios if you’d like more saltiness, sweetness, sourness, spiciness, umami.
2) Prepare a bowl with cold water and some ice. Steam the broccolini and edamame for about 3 minutes; as soon as they become tender, dump them into the ice bathe to halt the cooking process. Let them chill for a few minutes, then drain, dry, and toss in the sesame oil.
3) Reheat the tofu if necessary (an air fryer is great for this), and then combine with half of the sauce in a bowl, tossing gently to coat well.
4) Add a little extra water to the remaining sauce, enough to make it pourable, whisking to an even consistency.
5) Assemble; do it per your preference, but we recommend the order: rice, vegetables, tofu, cashews, sauce, sesame seeds, herbs.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Tofu vs Seitan – Which is Healthier?
- Plant vs Animal Protein: Head to Head
- Sweet Cinnamon vs Regular Cinnamon – Which is Healthier?
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Alzheimer’s Sex Differences May Not Be What They Appear
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Alzheimer’s Sex Differences May Not Be What They Appear
Women get Alzheimer’s at nearly twice the rate than men do, and deteriorate more rapidly after onset, too.
So… Why?
There are many potential things to look at, but four stand out for quick analysis:
- Chromosomes: women usually have XX chromosomes, to men’s usual XY. There are outliers to both groups, people with non-standard combinations of chromosomes, but not commonly enough to throw out the stats.
- Hormones: women usually have high estrogen and low testosterone, compared to men. Again there are outliers and this is a huge oversimplification that doesn’t even look at other sex hormones, but broadly speaking (which sounds vague, but is actually what is represented in epidemiological studies), it will be so.
- Anatomy: humans have some obvious sexual dimorphism (again, there are outliers, but again, not enough to throw out the stats); this seems least likely to be relevant (Alzheimer’s is probably not stored in the breasts, for examples), though average body composition (per muscle:fat ratio) could admittedly be a factor.
- Social/lifestyle: once again, #NotAllWomen etc, but broadly speaking, women and men often tend towards different social roles in some ways, and as we know, of course lifestyle can play a part in disease pathogenesis.
As a quick aside before we continue, if you’re curious about those outliers, then a wiki-walk into the fascinating world of intersex conditions, for example, could start here. But by and large, this won’t affect most people.
So… Which parts matter?
Back in 2018, Dr. Maria Teresa Ferretti et al. kicked up some rocks in this regard, looking not just at genes (as much research has focussed on) or amyloid-β (again, well-studied) but also at phenotypes and metabolic and social factors—bearing in mind that all three of those are heavily influenced by hormones. Noting, for example, that (we’ll quote directly here):
- Men and women with Alzheimer disease (AD) exhibit different cognitive and psychiatric symptoms, and women show faster cognitive decline after diagnosis of mild cognitive impairment (MCI) or AD dementia.
- Brain atrophy rates and patterns differ along the AD continuum between the sexes; in MCI, brain atrophy is faster in women than in men.
- The prevalence and effects of cerebrovascular, metabolic and socio-economic risk factors for AD are different between men and women.
See: Sex differences in Alzheimer disease—the gateway to precision medicine
So, have scientists controlled for each of those factors?
Mostly not! But they have found clues, anyway, while noting the limitations of the previous way of conducting studies. For example:
❝Women are more likely to develop Alzheimer’s disease and experience faster cognitive decline compared to their male counterparts. These sex differences should be accounted for when designing medications and conducting clinical trials❞
~ Dr. Feixiong Cheng
Read: Research finds sex differences in immune response and metabolism drive Alzheimer’s disease
Did you spot the clue?
It was “differences in immune response and metabolism”. These things are both influenced by (not outright regulated by, but strongly influenced by) sex hormones.
❝As [hormonal] sex influences both the immune system and metabolic process, our study aimed to identify how all of these individual factors influence one another to contribute to Alzheimer’s disease❞
~ Dr. Justin Lathia
Ignoring for a moment progesterone’s role in metabolism, estrogen is an immunostimulant and testosterone is an immunosuppressant. These thus both also have an effect in inflammation, which yes, includes neuroinflammation.
But wait a minute, shouldn’t that mean that women are more protected, not less?
It should! Except… Alzheimer’s is an age-related disease, and in the age-bracket that generally gets Alzheimer’s (again, there are outliers), menopause has been done and dusted for quite a while.
Which means, and this is critical: post-menopausal women not on HRT are essentially left without the immune boost usually directed by estrogen, while men of the same age will be ticking over with their physiology that (unlike that of the aforementioned women) was already adapted to function with negligible estrogen.
Specifically:
❝The metabolic consequences of estrogen decline during menopause accelerate neuropathology in women❞
~ Dr. Rasha Saleh
Critical idea to take away from all this:
Alzheimer’s research is going to be misleading if it doesn’t take into account sex differences, and not just that, but also specifically age-relevant sex differences—because that can flip the narrative. If we don’t take age into account, we could be left thinking estrogen is to blame, when in fact, it appears to be the opposite.
In the meantime, if you’re a woman of a certain age, you might talk with a doctor about whether HRT could be beneficial for you, if you haven’t already:
❝Women at genetic risk for AD (carrying at least one APOE e4 allele) seem to be particularly benefiting from MHT❞
(MHT = Menopausal Hormone Therapy; also commonly called HRT, which is the umbrella term for Hormone Replacement Therapies in general)
~ Dr. Herman Depypere
Source study: Menopause hormone therapy significantly alters pathophysiological biomarkers of Alzheimer’s disease
Pop-sci press release version: HRT could ward off Alzheimer’s among at-risk women
Take care!
Share This Post
-
Childhood Vaccination Rates, a Rare Health Bright Spot in Struggling States, Are Slipping
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Jen Fisher can do only so much to keep her son safe from the types of infections that children can encounter at school. The rest, she said, is up to other students and parents in their hometown of Franklin, Tennessee.
Fisher’s son Raleigh, 12, lives with a congenital heart condition, which has left him with a weakened immune system. For his protection, Raleigh has received all the recommended vaccines for a child his age. But even with his vaccinations, a virus that might only sideline another child could sicken him and land him in the emergency room, Fisher said.
“We want everyone to be vaccinated so that illnesses like measles and things that have basically been eradicated don’t come back,” Fisher said. “Those can certainly have a very adverse effect on Raleigh.”
For much of Raleigh’s life, Fisher could take comfort in the high childhood vaccination rate in Tennessee — a public health bright spot in a conservative state with poor health outcomes and one of the shortest life expectancies in the nation.
Mississippi and West Virginia, two similarly conservative states with poor health outcomes and short life expectancies, also have some of the highest vaccination rates for kindergartners in the nation — a seeming contradiction that stems from the fact that childhood vaccination requirements don’t always align with states’ other characteristics, said James Colgrove, a Columbia University professor who studies factors that influence public health.
“The kinds of policies that states have don’t map neatly on to ‘red’ versus ‘blue’ or one region or another,” Colgrove said.
Advocates, doctors, public health officials, and researchers worry such public health bright spots in some states are fading: Many states have recently reported an increase in people opting out of vaccines for their kids as Americans’ views shift.
During the 2023-24 school year, the percentage of kindergartners exempted from one or more vaccinations rose to 3.3%, the highest ever reported, with increases in 40 states and Washington, D.C., according to Centers for Disease Control and Prevention data. Tennessee and Mississippi were among those with increases. Nearly all exemptions nationally were for nonmedical reasons.
Vaccine proponents worry anti-vaccine messaging could accelerate a growing “health freedom” movement that has been pushed by leaders in states such as Florida. Momentum against vaccines is likely to continue to grow with the election of Donald Trump as president and his proposed nomination of anti-vaccine activist Robert F. Kennedy Jr. as secretary of the Department of Health and Human Services.
Pediatricians in states with high exemption rates, such as Florida and Georgia, say they’re concerned by what they see — declining immunization levels for kindergartners, which could lead to a resurgence in vaccine-preventable diseases such as measles. The Florida Department of Health reported nonmedical exemption rates as high as 50% for children in some areas.
“The religious exemption is huge,” said Brandon Chatani, a pediatric infectious disease doctor in Orlando. “That has allowed for an easy way for these kids to enter schools without vaccines.”
In many states, it’s easier to get a religious exemption than a medical one, which often requires signoff from a doctor.
Over the past decade, California, Connecticut, Maine, and New York have removed religious and philosophical exemptions from school vaccination requirements. West Virginia has not had them.
Idaho, Alaska, and Utah had the highest exemption rates for the 2023-24 school year, according to the CDC. Those states allow parents or legal guardians to exempt their children for religious reasons by submitting a notarized form or a signed statement.
Florida and Georgia, with some of the lowest reported minimum vaccination rates for kindergartners, allow parents to exempt their children by submitting a form with the child’s school or day care.
Both states have reported declines in uptake of the measles, mumps, and rubella vaccine, which is one of the most common childhood shots. In Georgia, MMR coverage for kindergartners dropped to 88.4% in the 2023-24 school year from 93.1% in 2019-20, according to the CDC. Florida dropped to 88.1% from 93.5% during the same period.
Andi Shane, a pediatric infectious disease specialist in Atlanta, traces Georgia’s declining rates to families who lack access to a pediatrician. State policies on exemptions are also key, she said.
“There’s lots of data to support the fact that when personal belief exemptions are not permitted, that vaccination rates are higher,” she said.
In December, Georgia public health officials put out an advisory saying the state had recorded significantly more whooping cough cases than in the prior year. According to CDC data, Georgia reported 280 cases in 2024 compared with 96 the year before.
Until 2023, Mississippi was one of the few states that allowed parents to opt out of vaccinating their kids only for medical reasons — and only with the approval of a doctor. That gave it among the highest vaccination rates in the nation as of the 2023-24 school year.
“It’s one of the few things Mississippi has done well,” said Anita Henderson, a pediatrician who has practiced in the southern part of the state for nearly 30 years. In terms of health, she said, childhood vaccination rates were the state’s one “shining star.”
But that changed in April 2023 when a federal judge ordered state officials to start allowing religious exemptions. The ruling has emboldened many families, Henderson said.
“We are seeing more and more skepticism, more and more vaccine hesitancy, and a lack of confidence because of this ruling,” she said.
State officials have granted more than 5,000 religious exemptions since the court order allowing them, according to the state health department. Daniel Edney, the state health officer, said most of the requests have come from “more affluent” residents in “pockets” of the state.
“Most people listen to the expert opinions of their pediatricians and family medicine doctors to stay on the vaccine schedule, because it’s what is best to protect their children,” he said.
West Virginia’s vaccine law — which hasn’t allowed nonmedical exemptions — also could soon change, Matthew Christiansen said in December before he resigned as the state’s health officer.
A bill that would have broadened exemptions made it through the legislature last year but was vetoed by outgoing Republican Gov. Jim Justice. The new governor, Republican Pat Morrisey, has been a vocal critic of vaccine mandates. And just a day after being inaugurated, he issued an executive order to propose provisions by Feb. 1 that could allow religious and conscientious exemptions.
“I want to send a message that if you have a religious belief, then we’re going to have an exception,” he said at a Jan. 14 press conference. “We’re not going to be the outlier.”
People asserting their personal freedoms to decline vaccines for their kids can ultimately curtail the ability of others to live full lives, Christiansen said. “Kids getting measles and mumps and polio and being paralyzed for their whole life is an impediment on personal freedom and autonomy for those kids,” he said.
Since the covid pandemic, anti-vaccine sentiment has been growing in Tennessee. One organization, Stand for Health Freedom, drafted a letter for constituents to send to their state lawmakers calling for the resignation of the medical director of Tennessee’s Vaccine-Preventable Diseases and Immunization Program. The group said she demonstrated a “lack of respect for the informed consent rights” of the people.
“They feel emboldened by the idea that this presidential administration seems to feel very strongly that a lot of these issues should be taken back to the states,” said Emily Delikat, director of Tennessee Families for Vaccines, a pro-vaccine group.
Ultimately, like many effective public health interventions, vaccines are a victim of their own success, said Henderson, the Mississippi pediatrician. Most people haven’t seen outbreaks of measles or polio, so they forget how dangerous the diseases are, she said.
“It may unfortunately take a resurgence of those diseases to raise awareness to the fact that these are dangerous, these are deadly, these are preventable,” she said. “I hope it doesn’t come to that.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
Are Electrolyte Supplements Worth It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When To Take Electrolytes (And When We Shouldn’t!)
Any sports nutrition outlet will sell electrolyte supplements. Sometimes in the form of sports drinks that claim to be more hydrating than water, or tablets that can be dissolved in water to make the same. How do they work, and should we be drinking them?
What are electrolytes?
They’re called “electrolytes” because they are ionized particles (so, they have a positive or negative electrical charge, depending on which kind of ion they are) that are usually combined in the form of salts.
The “first halves” of the salts include:
- Sodium
- Potassium
- Calcium
- Magnesium
The “second halves” of the salts include:
- Chloride
- Phosphate
- Bicarbonate
- Nitrate
It doesn’t matter too much which way they’re combined, provided we get what we need. Specifically, the body needs them in a careful balance. Too much or too little, and bad things will start happening to us.
If we live in a temperate climate with a moderate lifestyle and a balanced diet, and have healthy working kidneys, usually our kidneys will keep them all in balance.
Why might we need to supplement?
Firstly, of course, you might have a dietary deficiency. Magnesium deficiency in particular is very common in North America, as people simply do not eat as much greenery as they ideally would.
But, also, you might sweat out your electrolytes, in which case, you will need to replace them.
In particular, endurance training and High Intensity Interval Training are likely to prompt this.
However… Are you in a rush? Because if not, you might just want to recover more slowly:
❝Vigorous exercise and warm/hot temperatures induce sweat production, which loses both water and electrolytes. Both water and sodium need to be replaced to re-establish “normal” total body water (euhydration).
This replacement can be by normal eating and drinking practices if there is no urgency for recovery.
But if rapid recovery (<24 h) is desired or severe hypohydration (>5% body mass) is encountered, aggressive drinking of fluids and consuming electrolytes should be encouraged to facilitate recovery❞
Source: Fluid and electrolyte needs for training, competition, and recovery
Should we just supplement anyway, as a “catch-all” to be sure?
Probably not. In particular, it is easy to get too much sodium in one’s diet, let alone by supplementation.And, oversupplementation of calcium is very common, and causes its own health problems. See:
To look directly to the science on this one, we see a general consensus amongst research reviews: “this is complicated and can go either way depending on what else people are doing”:
- Trace minerals intake: risks and benefits for cardiovascular health
- Electrolyte minerals intake and cardiovascular health
Well, that’s not helpful. Any clearer pointers?
Yes! Researchers Latzka and Mountain put together a very practical list of tips. Rather, they didn’t put it as a list, but the following bullet points are information extracted directly from their abstract, though we’ve also linked the full article below:
- It is recommended that individuals begin exercise when adequately hydrated.
- This can be facilitated by drinking 400 mL to 600 mL of fluid 2 hours before beginning exercise and drinking sufficient fluid during exercise to prevent dehydration from exceeding 2% body weight.
- A practical recommendation is to drink small amounts of fluid (150-300 mL) every 15 to 20 minutes of exercise, varying the volume depending on sweating rate.
- During exercise lasting less than 90 minutes, water alone is sufficient for fluid replacement
- During prolonged exercise lasting longer than 90 minutes, commercially available carbohydrate electrolyte beverages should be considered to provide an exogenous carbohydrate source to sustain carbohydrate oxidation and endurance performance.
- Electrolyte supplementation is generally not necessary because dietary intake is adequate to offset electrolytes lost in sweat and urine; however, during initial days of hot-weather training or when meals are not calorically adequate, supplemental salt intake may be indicated to sustain sodium balance.
Source: Water and electrolyte requirements for exercise
Bonus tip:
We’ve talked before about the specific age-related benefits of creatine supplementation, but if you’re doing endurance training or HIIT, you might also want to consider a creatine-electrolyte combination sports drink (even if you make it yourself):
Where can I get electrolyte supplements?
They’re easy to find in any sports nutrition store, or you can buy them online; here’s an example product on Amazon for your convenience
You can also opt for natural and/or homemade electrolyte drinks:
Healthline | 8 Healthy Drinks Rich in Electrolytes
Enjoy!
Share This Post
Related Posts
-
5 Ways To Beat Cancer (And Other Diseases)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Systematic Approach To Healthy Eating
This is Dr. William Li. He’s a physician, cancer researcher, and educator. He also founded the Angiogenesis Foundation back in 1994.
We recently reviewed one of his books, “Eat To Beat Disease”.
He has another book that we haven’t reviewed at time of writing, “Eat To Beat Your Diet“, which you might like to check out.
What does he want us to know?
He wants us to know how to eat to beat cancer and other diseases, by means of five specific angles:
Angiogenesis
This is about replacing blood vessels, which of course happens all the time, but it becomes a problem when it is feeding a cancer in the process.
Here, based on Dr. Li’s work, is what can be done about it:
A List of Anti-Angiogenic Foods for a Cancer-Fighting Diet
Regeneration
Generally speaking, we want to replace healthy cells early, because if we wait until they get damaged, then that damage will be copied forwards. As well as intermittent fasting, there are other things we can do to promote this—even, Dr. Li’s research shows, for stem cells:
Doctor’s Tip: Regeneration (stem cells)—one of your body’s five defense systems
Microbiome health
Healthy gut, healthy rest of the body. We’ve written about this before:
Making Friends With Your Gut (You Can Thank Us Later)
DNA protection
DNA gets unravelled and damaged with age, the telomere caps get shorter, and mistakes get copied forward. So there more we can protect our DNA, the longer we can live healthily. There are many ways to do this, but Dr. Li was one of the first to bring to light the DNA-protecting benefits of kiwi fruit:
Immunity
Paradoxically, what’s good for your immune system (making it stronger) also helps to protect against autoimmune diseases (for most people, for the most part).
In short: it’s good to have an immune system that’s powerful not just in its counterattacks, but also in its discerning nature. There are dietary and other lifestyle approaches to both, and they’re mostly the same things:
Beyond Supplements: The Real Immune-Boosters!
and thus see also:
Want to know more?
You might enjoy his blog or podcast, and here’s his TED talk:
Want to watch it, but not right now? Bookmark it for later
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Science of Yoga – by Ann Swanson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are a lot of yoga books out there to say “bend this way, hold this that way” and so forth, but few that really explain what is going on, how, and why. And understanding those things is of course key to motivation and adherence. So that’s what this book provides!
The book is divided into sections, and in the first part we have a tour of human anatomy and physiology. This may seem almost unrelated to yoga, but is valuable necessary-knowledge to get the most out of the next section:
The next few parts are given over to yoga asanas (stretches, positions, poses, call them what you will in English) and now we are given a clear idea of what it is doing: we get to understand exactly what’s being stretched, what blood flow is being increased and how, what organs are being settled into their correct place, and many other such things.
Importantly, this means we also understand why certain things are the way they are, and why they can’t be done in some other slightly different but perhaps superficially easier way.
The style of the book is like a school textbook, really, but without patronizing the reader. The illustrations, of which there are many, are simple enough to be clear while being detailed enough to be informative.
Bottom line: if you’re ever doing yoga at home and wondering if you should cut a certain corner, this is the book that will tell you why you shouldn’t.
Click here to check out Science of Yoga, and optimize your practice!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Exercise That Protects Your Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Neuroscientist In The Gym
This is Dr. Wendy Suzuki. She’s a neuroscientist, and an expert in the neurobiology of memory, as well as neuroplasticity, and the role of exercise in neuroprotection.
We’ve sneakily semi-featured her before when we shared her Big Think talk:
Brain Benefits In Three Months… Through Walking?
Today we’re going to expand on that a little!
A Quick Recap
To share the absolute key points of that already fairly streamlined rundown:
- Exercise boosts levels of neurotransmitters such as dopamine and serotonin (and, which wasn’t mentioned there, noradrenaline)
- These are responsible for motivation, happiness, and focus (amongst other things)
- Persistent exercise boosts certain regions of the brain in particular, most notably the pre-frontal cortex and the hippocampi*
- These are responsible for planning and memory (amongst other things)
Dr. Suzuki advocates for stepping up your exercise routine if you can, with more exercise generally being better than less (unless you have some special medical reason why that’s not the case for you).
*often referred to in the singular as the hippocampus, but you have one on each side of your brain (unless a serious accident/incident destroyed one, but you’ll know if that applies to you, unless you lost both, in which case you will not remember about it).
What kind(s) of workout?
While a varied workout is best for overall health, for these brain benefits specifically, what’s most important is that it raises your heart rate.
This is why in her Big Think talk we shared before, she talks about the benefits of taking a brisk walk daily. See also:
If that’s not your thing, though (and/or is for whatever reason an inaccessible form of exercise for you), there is almost certainly some kind of High Intensity Interval Training that is a possibility for you. That might sound intimidating, but if you have a bit of floor and can exercise for one minute at a time, then HIIT is an option for you:
How To Do HIIT (Without Wrecking Your Body)
Dr. Suzuki herself is an ardent fan of “intenSati” which blends cardio workouts with yoga for holistic mind-and-body fitness. In fact, she loves it so much that she became a certified exercise instructor:
How much is enough?
It’s natural to want to know the minimum we can do to get results, but Dr. Suzuki would like us to bear in mind that when it comes to our time spent exercising, it’s not so much an expense of time as an investment in time:
❝Exercise is something that when you spend time on it, it will buy you time when you start to work❞
Read more: A Neuroscientist Experimented on Her Students and Found a Powerful Way to Improve Brain Function
Ok, but we really want to know how much!
Dr. Suzuki recommends at least three to four 30-minute exercise sessions per week.
Note: this adds up to less than the recommended 150 minutes of moderate exercise per week, but high-intensity exercise counts for twice the minutes for these purposes, e.g. 1 minute of high-intensity exercise is worth 2 minutes of moderate exercise.
How soon will we see benefits?
Benefits start immediately, but stack up cumulatively with continued long-term exercise:
❝My lab showed that a single workout can improve your ability to shift and focus attention, and that focus improvement will last for at least two hours. ❞
…which is a great start, but what’s more exciting is…
❝The more you’re working out, the bigger and stronger your hippocampus and prefrontal cortex gets. Why is that important?
Because the prefrontal cortex and the hippocampus are the two areas that are most susceptible to neurodegenerative diseases and normal cognitive decline in aging. ❞
In other words, while improving your heart rate through regular exercise will help prevent neurodegeneration by the usual mechanism of reducing neuroinflammation… It’ll also build the parts of your brain most susceptible to decline, meaning that when/if decline sets in, it’ll take a lot longer to get to a critical level of degradation, because it had more to start with.
Read more:
Inspir Modern Senior Living | Dr. Wendy Suzuki Boosts Brain Health with Exercise
Want more from Dr. Suzuki?
You might enjoy her TED talk:
Click Here If The Embedded Video Doesn’t Load Automatically
Prefer text? TED.com has a transcript for you
Prefer lots of text? You might like her book, which we haven’t reviewed yet but will soon:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Exercise boosts levels of neurotransmitters such as dopamine and serotonin (and, which wasn’t mentioned there, noradrenaline)