Alzheimer’s Sex Differences May Not Be What They Appear
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Alzheimer’s Sex Differences May Not Be What They Appear
Women get Alzheimer’s at nearly twice the rate than men do, and deteriorate more rapidly after onset, too.
So… Why?
There are many potential things to look at, but four stand out for quick analysis:
- Chromosomes: women usually have XX chromosomes, to men’s usual XY. There are outliers to both groups, people with non-standard combinations of chromosomes, but not commonly enough to throw out the stats.
- Hormones: women usually have high estrogen and low testosterone, compared to men. Again there are outliers and this is a huge oversimplification that doesn’t even look at other sex hormones, but broadly speaking (which sounds vague, but is actually what is represented in epidemiological studies), it will be so.
- Anatomy: humans have some obvious sexual dimorphism (again, there are outliers, but again, not enough to throw out the stats); this seems least likely to be relevant (Alzheimer’s is probably not stored in the breasts, for examples), though average body composition (per muscle:fat ratio) could admittedly be a factor.
- Social/lifestyle: once again, #NotAllWomen etc, but broadly speaking, women and men often tend towards different social roles in some ways, and as we know, of course lifestyle can play a part in disease pathogenesis.
As a quick aside before we continue, if you’re curious about those outliers, then a wiki-walk into the fascinating world of intersex conditions, for example, could start here. But by and large, this won’t affect most people.
So… Which parts matter?
Back in 2018, Dr. Maria Teresa Ferretti et al. kicked up some rocks in this regard, looking not just at genes (as much research has focussed on) or amyloid-β (again, well-studied) but also at phenotypes and metabolic and social factors—bearing in mind that all three of those are heavily influenced by hormones. Noting, for example, that (we’ll quote directly here):
- Men and women with Alzheimer disease (AD) exhibit different cognitive and psychiatric symptoms, and women show faster cognitive decline after diagnosis of mild cognitive impairment (MCI) or AD dementia.
- Brain atrophy rates and patterns differ along the AD continuum between the sexes; in MCI, brain atrophy is faster in women than in men.
- The prevalence and effects of cerebrovascular, metabolic and socio-economic risk factors for AD are different between men and women.
See: Sex differences in Alzheimer disease—the gateway to precision medicine
So, have scientists controlled for each of those factors?
Mostly not! But they have found clues, anyway, while noting the limitations of the previous way of conducting studies. For example:
❝Women are more likely to develop Alzheimer’s disease and experience faster cognitive decline compared to their male counterparts. These sex differences should be accounted for when designing medications and conducting clinical trials❞
~ Dr. Feixiong Cheng
Read: Research finds sex differences in immune response and metabolism drive Alzheimer’s disease
Did you spot the clue?
It was “differences in immune response and metabolism”. These things are both influenced by (not outright regulated by, but strongly influenced by) sex hormones.
❝As [hormonal] sex influences both the immune system and metabolic process, our study aimed to identify how all of these individual factors influence one another to contribute to Alzheimer’s disease❞
~ Dr. Justin Lathia
Ignoring for a moment progesterone’s role in metabolism, estrogen is an immunostimulant and testosterone is an immunosuppressant. These thus both also have an effect in inflammation, which yes, includes neuroinflammation.
But wait a minute, shouldn’t that mean that women are more protected, not less?
It should! Except… Alzheimer’s is an age-related disease, and in the age-bracket that generally gets Alzheimer’s (again, there are outliers), menopause has been done and dusted for quite a while.
Which means, and this is critical: post-menopausal women not on HRT are essentially left without the immune boost usually directed by estrogen, while men of the same age will be ticking over with their physiology that (unlike that of the aforementioned women) was already adapted to function with negligible estrogen.
Specifically:
❝The metabolic consequences of estrogen decline during menopause accelerate neuropathology in women❞
~ Dr. Rasha Saleh
Critical idea to take away from all this:
Alzheimer’s research is going to be misleading if it doesn’t take into account sex differences, and not just that, but also specifically age-relevant sex differences—because that can flip the narrative. If we don’t take age into account, we could be left thinking estrogen is to blame, when in fact, it appears to be the opposite.
In the meantime, if you’re a woman of a certain age, you might talk with a doctor about whether HRT could be beneficial for you, if you haven’t already:
❝Women at genetic risk for AD (carrying at least one APOE e4 allele) seem to be particularly benefiting from MHT❞
(MHT = Menopausal Hormone Therapy; also commonly called HRT, which is the umbrella term for Hormone Replacement Therapies in general)
~ Dr. Herman Depypere
Source study: Menopause hormone therapy significantly alters pathophysiological biomarkers of Alzheimer’s disease
Pop-sci press release version: HRT could ward off Alzheimer’s among at-risk women
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

From straight to curly, thick to thin: here’s how hormones and chemotherapy can change your hair
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Head hair comes in many colours, shapes and sizes, and hairstyles are often an expression of personal style or cultural identity.
Many different genes determine our hair texture, thickness and colour. But some people’s hair changes around the time of puberty, pregnancy or after chemotherapy.
So, what can cause hair to become curlier, thicker, thinner or grey?
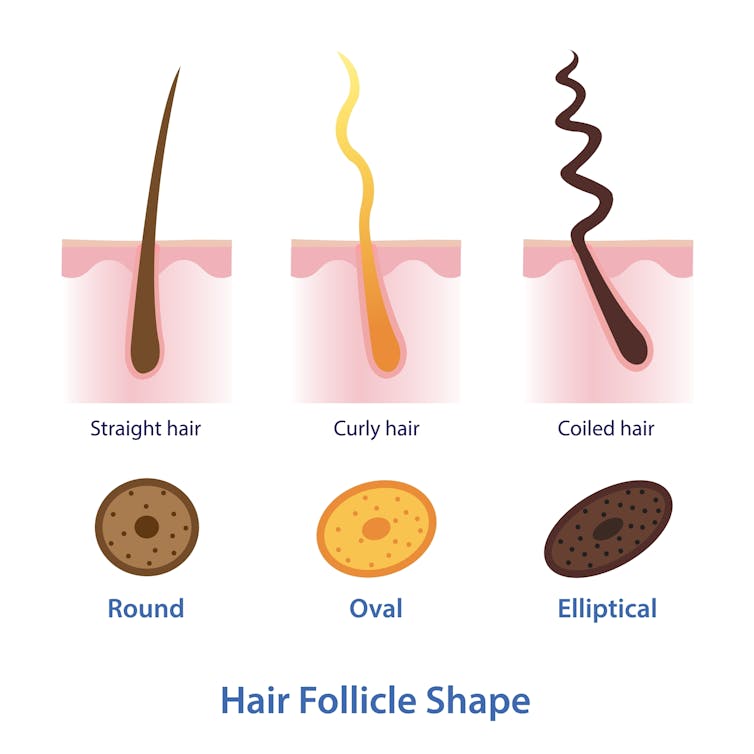
Curly or straight? How hair follicle shape plays a role
Hair is made of keratin, a strong and insoluble protein. Each hair strand grows from its own hair follicle that extends deep into the skin.
Curly hair forms due to asymmetry of both the hair follicle and the keratin in the hair.
Follicles that produce curly hair are asymmetrical and curved and lie at an angle to the surface of the skin. This kinks the hair as it first grows.
The asymmetry of the hair follicle also causes the keratin to bunch up on one side of the hair strand. This pulls parts of the hair strand closer together into a curl, which maintains the curl as the hair continues to grow.
Follicles that are symmetrical, round and perpendicular to the skin surface produce straight hair.

Each hair strand grows from its own hair follicle.
Mosterpiece/ShutterstockLife changes, hair changes
Our hair undergoes repeated cycles throughout life, with different stages of growth and loss.
Each hair follicle contains stem cells, which multiply and grow into a hair strand.
Head hairs spend most of their time in the growth phase, which can last for several years. This is why head hair can grow so long.
Let’s look at the life of a single hair strand. After the growth phase is a transitional phase of about two weeks, where the hair strand stops growing. This is followed by a resting phase where the hair remains in the follicle for a few months before it naturally falls out.
The hair follicle remains in the skin and the stems cells grow a new hair to repeat the cycle.
Each hair on the scalp is replaced every three to five years.

Each hair on the scalp is replaced every three to five years.
Just Life/ShutterstockHormone changes during and after pregnancy alter the usual hair cycle
Many women notice their hair is thicker during pregnancy.
During pregnancy, high levels of oestrogen, progesterone and prolactin prolong the resting phase of the hair cycle. This means the hair stays in the hair follicle for longer, with less hair loss.
A drop in hormones a few months after delivery causes increased hair loss. This is due to all the hairs that remained in the resting phase during pregnancy falling out in a fairly synchronised way.
Hair can change around puberty, pregnancy or after chemotherapy
This is related to the genetics of hair shape, which is an example of incomplete dominance.
Incomplete dominance is when there is a middle version of a trait. For hair, we have curly hair and straight hair genes. But when someone has one curly hair gene and one straight hair gene, they can have wavy hair.
Hormonal changes that occur around puberty and pregnancy can affect the function of genes. This can cause the curly hair gene of someone with wavy hair to become more active. This can change their hair from wavy to curly.
Researchers have identified that activating specific genes can change hair in pigs from straight to curly.
Chemotherapy has very visible effects on hair. Chemotherapy kills rapidly dividing cells, including hair follicles, which causes hair loss. Chemotherapy can also have genetic effects that influence hair follicle shape. This can cause hair to regrow with a different shape for the first few cycles of hair regrowth.

Your hair can change at different stages of your life.
Igor Ivakhno/ShutterstockHormonal changes as we age also affect our hair
Throughout life, thyroid hormones are essential for production of keratin. Low levels of thyroid hormones can cause dry and brittle hair.
Oestrogen and androgens also regulate hair growth and loss, particularly as we age.
Balding in males is due to higher levels of androgens. In particular, high dihydrotestosterone (sometimes shortened to DHT), which is produced in the body from testosterone, has a role in male pattern baldness.
Some women experience female pattern hair loss. This is caused by a combination of genetic factors plus lower levels of oestrogen and higher androgens after menopause. The hair follicles become smaller and smaller until they no longer produce hairs.
Reduced function of the cells that produce melanin (the pigment that gives our hair colour) is what causes greying.

Theresa Larkin, Associate professor of Medical Sciences, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post

Dealing with Thirst!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Busting The Myth of “Eight Glasses Of Water A Day”
Everyone knows we must drink 8 glasses of water a day, or else we’re going to get a failing grade at being a healthy human—like not flossing, or not using adequate sunscreen.
But… Do we? And does tea count? How about (we dare but whisper it) coffee? And soda drinks are mostly water, right? But aren’t some drinks dehydrating? Are special electrolyte drinks really better? There are so many things to consider, so many differing advices, and it’s easy to give up, or just choose what to believe in as a leap of faith.
A quick brain-teaser for you first, though:
If coffee and soda don’t count because they’re dehydrating, then what if you were to take:
– A concentrated tiny cup of espresso, and then a glass of water, would the glass of water count?
– Or (we don’t relish the thought) what if you took a spoonful of soda syrup, and then a glass of water, would the glass of water count?
If your answer was “yes, it’s a glass of water”, then why would it not count if it were taken all at once (e.g. as an Americano coffee, or a regular soda)?
If your answer was “yes, but that water might only offset the dehydration caused by the coffee/syrup, so I might only be breaking even”, then you were thinking about this the right way:
How much water you need depends on many factors that can be affected by what else you are consuming and what else you are doing. Science loves averages, so eight glasses a day may be great if you are of average health, and average body size, in a temperate climate, doing moderate exercise, and so on and so on.
If you’re not the most average person of all time? You may need to take into account a lot of factors, ranging from what you ate for dinner to how much you perspired during your morning exercises. As you (probably) don’t live in laboratory conditions, this can become an impossible task—and if you missed (or guessed incorrectly) even one factor, the whole calculation will be thrown off. But is there any other way to know?
What of the infamous pee test? Drink enough to make your urine as clear as possible, and if it’s dark, you’re dehydrated, common wisdom says.
In reality, however, that tells you not what’s in your body, but rather, what got ejected from your body. If your urine is dark, it might mean you had too little water, but it also could just mean you had the right amount of water but too much sodium, for instance. A study of this was done on athletes, and found no correlation between urine color and actual bodily hydration when measured directly via a blood test.
So, if we can’t just have an app tell us “drink this many glasses of water”, and we can’t trust urine color, what can we do?
What we can do is trust that our body comes with (for free!) a wonderful homeostatic system and it will try to correct any imbalances. If you are thirsty, you’re dehydrated. Drink something with plenty of water in, if not plain water.
But what about special electrolyte drinks? If you need salts, you will crave them. Craving a salty snack? Go for it! Or if you prefer not to snack, do a salt lick test (just put a little salt on your finger, and taste it; if it tastes good, wait a minute or two, and then have a little more, and repeat until it doesn’t).
Bonus Tip:
- Make sure you always have a source of hydration (that you enjoy!) to hand. Maybe it’s chilled water, maybe it’s a pot of tea, maybe it’s a sports drink, it doesn’t matter too much. Even coffee is actually fine, by the way (but don’t overdo it).
- Make a personal rule: “I will always make time for hydration”. That means, if you’re thirsty, have something with water in it now. Not when you’ve finished what you’re doing (unless you really can’t stop, because you are a racecar driver mid-race, or a surgeon mid-operation, or something), but now. Do not postpone it until after you’ve done some other thing first; you will forget and it will keep getting postponed. Always make time for water.
Share This Post

What Your Doctor May Not Tell You About Fibromyalgia – by Dr. R. Paul St Amand
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The core claim of the book is that guaifenesin, an over-the-counter expectorant (with a good safety profile) usually taken to treat a chesty cough, is absorbed from the gastrointestinal tract, and is rapidly metabolized and excreted into the urine—and on the way, it lowers uric acid levels, which is a big deal for fibromyalgia sufferers.
He goes on to explain how the guaifenesin, by a similar biochemical mechanism, additionally facilitates the removal of other excess secretions that are associated with fibromyalgia.
The science for all this is… Compelling and logical, while not being nearly so well-established yet as his confidence would have us believe.
In other words, he could be completely wrong, because adequate testing has not yet been done. However, he also could be right; scientific knowledge is, by the very reality of scientific method, always a step behind hypothesis and theory (in that order).
Meanwhile, there are certainly many glowing testimonials from fibromyalgia sufferers, saying that this helped a lot.
Bottom line: if you have fibromyalgia and do not mind trying a relatively clinically untested (yet logical and anecdotally successful) protocol to lessen then symptoms (allegedly, to zero), then this book will guide you through that and tell you everything to watch out for.
Share This Post
Related Posts

From Cucumbers To Kindles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You’ve Got Questions? We’ve Got Answers!
Q: Where do I get cucumber extract?
A: You can buy it from BulkSupplements.com (who, despite their name, start at 100g packs)
Alternatively: you want it as a topical ointment (for skin health) rather than as a dietary supplement (for bone and joint health), you can extract it yourself! No, it’s not “just juice cucumbers”, but it’s also not too tricky.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

We created a VR tool to test brain function. It could one day help diagnose dementia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you or a loved one have noticed changes in your memory or thinking as you’ve grown older, this could reflect typical changes that occur with ageing. In some cases though, it might suggest something more, such as the onset of dementia.
The best thing to do if you have concerns is to make an appointment with your GP, who will probably run some tests. Assessment is important because if there is something more going on, early diagnosis can enable prompt access to the right interventions, supports and care.
But current methods of dementia screening have limitations, and testing can be daunting for patients.
Our research suggests virtual reality (VR) could be a useful cognitive screening tool, and mitigate some of the challenges associated with current testing methods, opening up the possibility it may one day play a role in dementia diagnosis.
Where current testing is falling short
If someone is worried about their memory and thinking, their GP might ask them to complete a series of quick tasks that check things like the ability to follow simple instructions, basic arithmetic, memory and orientation.
These sorts of screening tools are really good at confirming cognitive problems that may already be very apparent. But commonly used screening tests are not always so good at detecting early and more subtle difficulties with memory and thinking, meaning such changes could be missed until they get worse.
A clinical neuropsychological assessment is better equipped to detect early changes. This involves a comprehensive review of a patient’s personal and medical history, and detailed assessment of cognitive functions, including attention, language, memory, executive functioning, mood factors and more. However, this can be costly and the testing can take several hours.
Testing is also somewhat removed from everyday experience, not directly tapping into activities of daily living.
Enter virtual reality
VR technology uses computer-generated environments to create immersive experiences that feel like real life. While VR is often used for entertainment, it has increasingly found applications in health care, including in rehabilitation and falls prevention.
Using VR for cognitive screening is still a new area. VR-based cognitive tests generally create a scenario such as shopping at a supermarket or driving around a city to ascertain how a person would perform in these situations.
Notably, they engage various senses and cognitive processes such as sight, sound and spatial awareness in immersive ways. All this may reveal subtle impairments which can be missed by standard methods.
VR assessments are also often more engaging and enjoyable, potentially reducing anxiety for those who may feel uneasy in traditional testing environments, and improving compliance compared to standard assessments.

Millions of people around the world have dementia.
pikselstock/ShutterstockMost studies of VR-based cognitive tests have explored their capacity to pick up impairments in spatial memory (the ability to remember where something is located and how to get there), and the results have been promising.
Given VR’s potential for assisting with diagnosis of cognitive impairment and dementia remains largely untapped, our team developed an online computerised game (referred to as semi-immersive VR) to see how well a person can remember, recall and complete everyday tasks. In our VR game, which lasts about 20 minutes, the user role plays a waiter in a cafe and receives a score on their performance.
To assess its potential, we enlisted more than 140 people to play the game and provide feedback. The results of this research are published across three recent papers.
Testing our VR tool
In our most recently published study, we wanted to verify the accuracy and sensitivity of our VR game to assess cognitive abilities.
We compared our test to an existing screening tool (called the TICS-M) in more than 130 adults. We found our VR task was able to capture meaningful aspects of cognitive function, including recalling food items and spatial memory.
We also found younger adults performed better in the game than older adults, which echoes the pattern commonly seen in regular memory tests.

Adults of a range of ages tried our computerised game.
pikselstock/ShutterstockIn a separate study, we followed ten adults aged over 65 while they completed the game, and interviewed them afterwards. We wanted to understand how this group – who the tool would target – perceived the task.
These seniors told us they found the game user-friendly and believed it was a promising tool for screening memory. They described the game as engaging and immersive, expressing enthusiasm to continue playing. They didn’t find the task created anxiety.
For a third study, we spoke to seven health-care professionals about the tool. Overall they gave positive feedback, and noted its dynamic approach to age-old diagnostic challenges.
However, they did flag some concerns and potential barriers to implementing this sort of tool. These included resource constraints in clinical practice (such as time and space to carry out the assessment) and whether it would be accessible for people with limited technological skills. There was also some scepticism about whether the tool would be an accurate method to assist with dementia diagnosis.
While our initial research suggests this tool could be a promising way to assess cognitive performance, this is not the same as diagnosing dementia. To improve the test’s ability to accurately detect those who likely have dementia, we’ll need to make it more specific for that purpose, and carry out further research to validate its effectiveness.
We’ll be conducting more testing of the game soon. Anyone interested in giving it a go to help with our research can register on our team’s website.

Joyce Siette, Research Theme Fellow in Health and Wellbeing, Western Sydney University and Paul Strutt, Senior Lecturer in Psychology, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Curious Kids: what are the main factors in forming someone’s personality?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“What are the main factors in forming someone’s personality?” – Emma, age 10, from Shanghai
Hello Emma, and thank you for this very interesting question!
Let’s start by exploring what we mean by personality. Have you noticed no two people are completely alike? We all see, experience, and understand the world in different ways.
For example, some people love spending time with friends and being the centre of attention, whereas other people are more shy and enjoy having time to themselves.
Your unique personality is shaped by your genes as well as various influences in your environment. And your personality plays an important role in how you interact with the world.
The big five
Did you know there are scientists who spend time researching personality? Their research is concerned with describing the ways people differ from each other, and understanding how these differences could be important for other parts of life such as our health and how well we do in school or at work.
There are many different perspectives on personality. A widely accepted viewpoint based on a lot of research is called the five factor model or the “big five”. According to this theory, a great deal of a person’s personality can be summarised in terms of where they sit on five dimensions, called traits:
- the introversion-extraversion trait refers to how much someone is outgoing and social (extroverted) or prefers being with smaller groups of friends or focusing on their own thoughts (introverted)
- agreeableness captures how much someone tends to be cooperative and helps others
- openness to experience refers to how much a person is creative and enjoys experiencing new things
- neuroticism describes a person’s tendency to experience negative feelings, like worrying about things that could go wrong
- conscientiousness encompasses how much a person is organised, responsible, and dedicated to things that are important to them, like schoolwork or training for a sports team.
A person can have high, low, or moderate levels of each of these traits. And understanding whether someone has higher or lower levels of the big five can tell us a lot about how we might expect them to behave in different situations.
So what shapes our personalities?
A number of factors shape our personalities, including our genes and social environment.
Our bodies are made up of many very small structures called cells. Within these cells are genes. We inherit genes from our parents, and they carry the information needed to make our bodies and personalities. So, your personality may be a bit like your parents’ personalities. For example, if you’re an outgoing sort of person who loves to meet new people, perhaps one or both of your parents are very social too.

Our personalities are influenced by the genes we get from our parents.
KieferPix/ShutterstockPersonalities are also affected by our environment, such as our experiences and our relationships with family and friends. For example, some research has shown our relationships with our parents can influence our personality. If we have loving and warm relationships, we may be more agreeable and open. But if our relationships are hurtful or stressful, this may increase our neuroticism.
Another study showed that, over time, young children who were more physically active were less introverted (less shy) and less likely to get very upset when things don’t go their way, compared to children who were less physically active. Although we don’t know why this is for sure, one possible explanation is that playing sport leads to reduced shyness because it introduces children to different people.
While we’re learning more about personality development all the time, research in this area presents quite a few challenges. Many different biological, cultural and environmental influences shape our development, and these factors can interact with each other in complex ways.
Is our personality fixed once we become adults?
Although we develop most of our personality when we are young, and people’s personalities tend to become more stable as they get older, it is possible for aspects of a person’s personality to change, even when they are fully grown.
A good example of this can be seen among people who seek treatment for conditions like anxiety or depression. People who respond well to working with a psychologist can show decreases in neuroticism, indicating they become less likely to worry a lot or feel strong negative feelings when something stressful happens.
Hello, Curious Kids! Do you have a question you’d like an expert to answer? Ask an adult to send your question to mailto:curiouskids@theconversation.edu.au

Tim Windsor, Professor, Director, Generations Research Initiative, College of Education, Psychology and Social Work, Flinders University and Natalie Goulter, Lecturer, College of Education, Psychology and Social Work, Flinders University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: