Rainbow Roasted Potato Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This salad has potatoes in it, but it’s not a potato salad as most people know it. The potatoes are roasted, but in a non-oily-dressing, that nevertheless leaves them with an amazing texture—healthy and delicious; the best of both worlds. And the rest? We’ve got colorful vegetables, we’ve got protein, we’ve got seasonings full of healthy spices, and more.
You will need
- 1½ lbs new potatoes (or any waxy potatoes; sweet potato is also a great option; don’t peel them, whichever you choose) cut into 1″ chunks
- 1 can / 1 cup cooked cannellini beans (or your preferred salad beans)
- 1 carrot, grated
- 2 celery stalks, finely chopped
- 3 spring onions, finely chopped
- ½ small red onion, finely sliced
- 2 tbsp white wine vinegar
- 1 tbsp balsamic vinegar
- 1 tbsp lemon juice
- 1 tbsp nutritional yeast
- 1 tsp garlic powder
- 1 tsp black pepper
- ½ tsp red chili powder
- We didn’t forget salt; it’s just that with the natural sodium content of the potatoes plus the savory flavor-enhancing properties of the nutritional yeast, it’s really not needed here. Add if you feel strongly about it, opting for low-sodium salt, or MSG (which has even less sodium).
- To serve: 1 cup basil pesto (we’ll do a recipe one of these days; meanwhile, store-bought is fine, or you can use the chermoula we made the other day, ignoring the rest of that day’s recipe and just making the chermoula component)
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven as hot as it goes!
2) Combine the potatoes, white wine vinegar, nutritional yeast, garlic powder, black pepper, and red chili powder, mixing thoroughly (but gently!) to coat.
3) Spread the potatoes on a baking tray, and roast in the middle of the oven (for best evenness of cooking); because of the small size of the potato chunks, this should only take about 25 minutes (±5mins depending on your oven); it’s good to turn them halfway through, or at least jiggle them if you don’t want to do all that turning.
4) Allow to cool while still on the baking tray (this allows the steam to escape immediately, rather than the steam steaming the other potatoes, as it would if you put them in a bowl).
5) Now put them in a serving bowl, and mix in the beans, vegetables, balsamic vinegar, and lemon juice, mixing thoroughly but gently
6) Add generous lashings of the pesto to serve; it should be gently mixed a little too, so that it’s not all on top.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- White Potato vs Sweet Potato – Which is Healthier?
- Eat More (Of This) For Lower Blood Pressure
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Apple vs Peach – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apples to peaches, we picked the peaches.
Why?
Both have their merits, but apples can’t compete with peaches’ micronutrient profile!
In terms of macros, apples have more carbs and fiber, for a comparable glycemic index, so we give apples a marginal win in the macros category to start with.
In the category of vitamins, apples have more vitamin B6, while peaches have more of vitamins A, B1, B2, B3, B5, B7, B9, C, E, K, and choline—an easy win for peaches.
When it comes to minerals, apples are not higher in any minerals, while peaches have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. Another clear win for peaches!
Looking at polyphenols, peaches have a higher total amount (in mg/100g) of polyphenols, as well as more variety thereof. One more win for peaches.
Adding up the sections makes for a clear win for peaches, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Top 8 Fruits That Prevent & Kill Cancer ← peaches are number 2 on the list! They contain phytochemicals that induce cell death in cancer cells while sparing healthy ones 😎
Enjoy!
Share This Post
-
Change Your Brain, Change Your Life – by Dr. Daniel G. Amen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
To what extent can we change our brains, and to what extent are we stuck with what we have?
Dr. Amen tells us that being mindful of both ends of this is critical:
- Neuroplasticity means we can, indeed, change our brains
- We do, however, have fundamental “brain types” based on our neurochemistry and physical brain structure
He argues for the use of brain imaging technology to learn more about the latter… In order to better go about doing what we can with the former.
The book looks at how these different brain types can lead to situations where what works as a treatment for one person can often not work for another. It’s also prescriptive, about what sorts of treatments (and lifestyle adjustments) are more likely to do better for each.
Where the book excels is in giving ideas and pointers for exploration… Things to take to one’s doctor, and—for example—request certain tests, and then what to do with those.
Where the book is a little light is on including hard science in the explanations. The hard science is referred to, but is considered beyond the scope of the book, or perhaps beyond the interest of the reader. That’s unfortunate, as we’d have liked to have seen more of it, rather than taking claims at face value without evidence.
Bottom line: this is distinctly “pop science” in presentation, but can give a lot of great ideas for learning more about our own brains and brain health… And then optimizing such.
Click here to check out “Change Your Brain; Change Your Life” on Amazon today!
Share This Post
-
The Problem With Sweeteners
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The WHO’s view on sugar-free sweeteners
The WHO has released a report offering guidance regards the use of sugar-free sweeteners as part of a weight-loss effort.
In a nutshell, the guidance is: don’t
- Here’s the report itself: Use of non-sugar sweeteners: WHO guideline
- Here’s the WHO’s own press release about it: WHO advises not to use non-sugar sweeteners for weight control in newly released guideline
- And it was based on this huge systematic review: Health effects of the use of non-sugar sweeteners: a systematic review and meta-analysis
They make for interesting reading, so if you don’t have time now, you might want to just quickly open and bookmark them for later!
Some salient bits and pieces:
Besides that some sweeteners can cause gastro-intestinal problems, a big problem is desensitization:
Because many sugar substitutes are many times (in some cases, hundreds of times) sweeter than sugar, this leads to other sweet foods tasting more bland, causing people to crave sweeter and sweeter foods for the same satisfaction level.
You can imagine how that’s not a spiral that’s good for the health!
The WHO recommendation applies to artificial and naturally-occurring non-sugar sweeteners, including:
- Acesulfame K
- Advantame
- Aspartame
- Cyclamates
- Neotame
- Saccharin
- Stevia
Sucralose and erythritol, by the way, technically are sugars, just not “that kind of sugar” so they didn’t make the list of non-sugar sweeteners.
That said, a recent study did find that erythritol was linked to a higher risk of heart attack, stroke, and early death, so it may not be an amazing sweetener either:
Read: The artificial sweetener erythritol and cardiovascular event risk
Want to know a good way of staying healthy in the context of sweeteners?
Just get used to using less. Your taste buds will adapt, and you’ll get just as much pleasure as before, from progressively less sweetening agent.
Share This Post
Related Posts
-
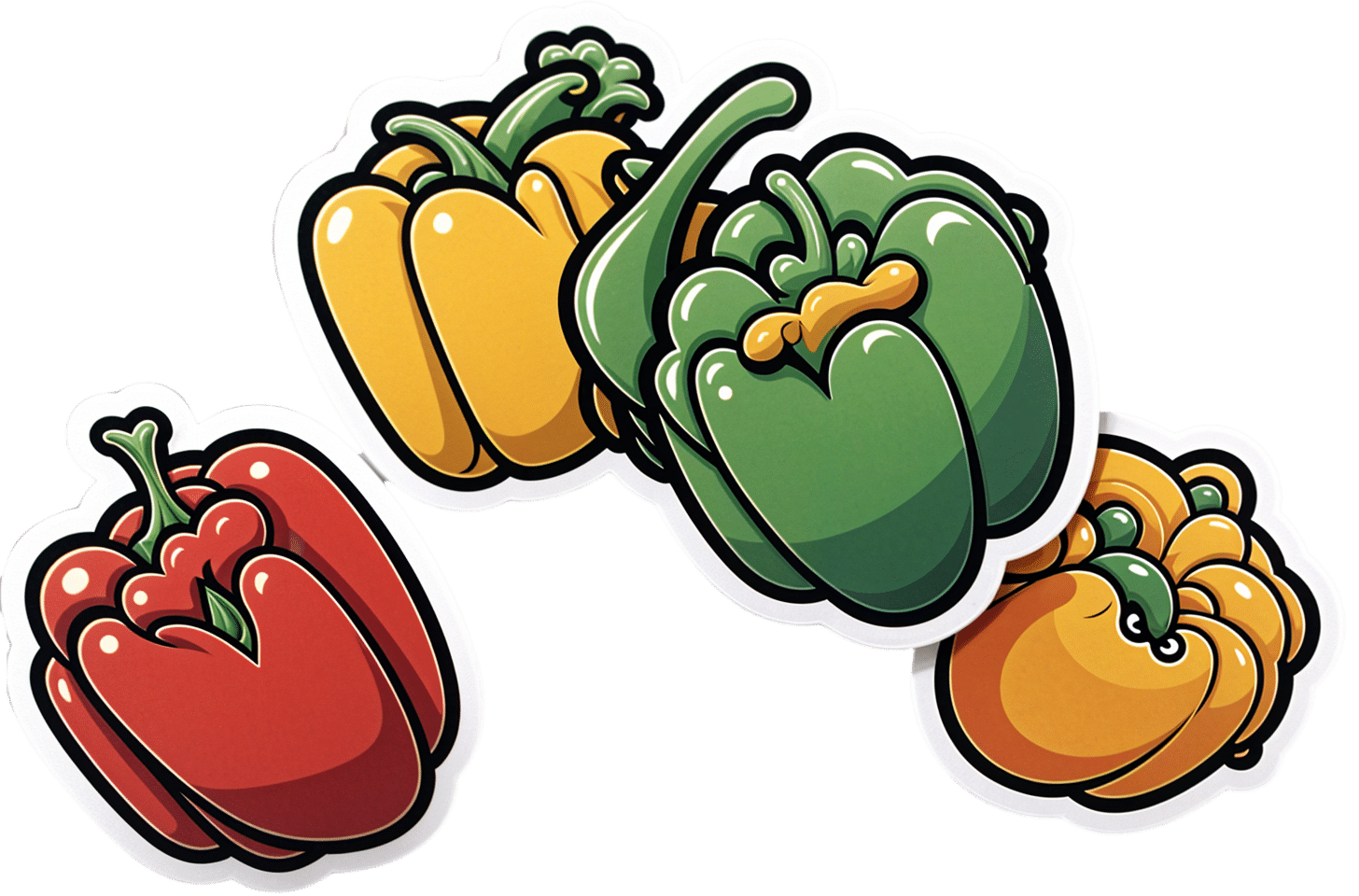
Which Bell Peppers To Pick?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Bell Peppers: A Spectrum Of Specialties
We were going to do this as part of our ongoing “This Or That?” challenge, but as there are four main types all with many different benefits, we thought this bunch of fruits deserved a main feature.
And yes, they’re botanically fruits, even if culinarily used as vegetables—much like tomatoes, famously!
They’re all the same (but also very much not)
A thing to know is that whether bell peppers be green, yellow, orange, or red, they’re all the same plant, Capiscum anuum. All that differs is how early or late they’re harvested.
Notwithstanding the “Capiscum” genus, they don’t contain capsaicin (as is found in hot peppers). Capsaicin’s a wonderful phytochemical:
Capsaicin For Weight Loss And Against Inflammation
…but today we’re all about the bell peppers.
So, let’s see how they stack up!
💚 Green for lutein
Lutein is especially important for the eyes and [the rest of the] brain, to the point that there’s now an Alzheimer’s test that measures lutein concentration in the eye:
Green peppers have most of this important carotenoid, though the others all have some too. See also:
💛 Yellow for vitamin C
Yellow peppers are technically highest in vitamin C, but all of them contain far more than the daily dose per fruit already, so if there’s any color of pepper that’s nutritionally the most expendable, it’s yellow, since any other color pepper can take its place.
Watch out, though! Cooking destroys vitamin C, so if you want to get your Cs in, you’re going to want to do it raw.
🧡 Orange for zeaxanthin and cryptoxanthins
Similar in their benefits to lutein, these antioxidant carotenoids are found most generously in orange peppers (20x as much as in yellow, 10x as much as in red, and slightly more than in green).
❤️ Red for vitamins A & B6
Red peppers are richest by far in vitamin A, with one fruit giving the daily dose already. The others have about 10% of that, give or take.
Red peppers also have the most vitamin B6, though the others also have nearly as much.
❤️ Red for lycopene
We must do a main feature for lycopene sometime, as unlike a lot of antioxidant carotenoids, lycopene is found in comparatively very few foods (most famously it’s present in tomatoes).
Red is the only color of pepper to have lycopene.
10almonds tip: to get the most out of your lycopene, cook these ones!
Lycopene becomes 4x more bioavailable when cooked:
Lycopene in tomatoes: chemical and physical properties affected by food processing ← this paper is about tomatoes but lycopene is lycopene and this applies to the lycopene in red peppers, too
And the overall winner is…
You! Because you get to eat all four of them
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Peanuts vs Walnuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing peanuts to walnuts, we picked the peanuts.
Why?
What heresy is this?!
“But walnuts are more expensive!”, we hear you cry. “They have omega-3s! They look like little brains!”
And, we must confess, all of these things are true. However…
In terms of macros, peanuts have much more protein, and a little more fiber, while walnuts have more fat. And yes, those fats are healthy, and yes, the omega-3 content of walnuts is worth noting. However, while walnuts are higher in total and polyunsaturated fats, peanuts are higher in monounsaturated fats, which are also beneficial. All in all, we’re calling it either a tie on macros, or a win for peanuts, as it really is a lot more protein, and we always consider fiber of top importance.
In the category of vitamins, peanuts have (a lot) more of vitamins B1, B3, B5, B9, E, and choline, while walnuts have a (very) little more of vitamins B2 and B6. So, a clear win for peanuts here, and that’s without considering that in terms of margins of difference, peanuts have 11x the vitamin E, for example.
Looking at minerals, peanuts have more iron, magnesium, phosphorus, potassium, selenium, and zinc, while walnuts have more calcium, copper, and manganese. Another clear win for peanuts.
When it comes to polyphenols, peanuts have more diverse polyphenols, while walnuts have a greater total mass of polyphenols. A tie here, or possibly a subjective win for walnuts.
In short, both are great and both have their merits, but by the numbers, and adding up the sections, peanuts take the win today. Still (assuming no allergy), by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Why You Should Diversify Your Nuts
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
In Plain English…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Time!
This is the bit whereby each week, we respond to subscriber questions/requests/etc
Have something you’d like to ask us, or ask us to look into? Hit reply to any of our emails, or use the feedback widget at the bottom, and a Real Human™ will be glad to read it!
Q: Love to have someone research all the additives in our medicines, (risk of birth control and breast cancer) and what goes in all of our food and beverages. So much info out there, but there are so many variations, you never know who to believe.
That’s a great idea! There are a lot of medicines and food and beverages out there, so that’s quite a broad brief, but! We could well do a breakdown of very common additives, and demystify them, sorting them into good/bad/neutral, e.g:
- Ascorbic acid—Good! This is Vitamin C
- Acetic acid—Neutral! This is vinegar
- Acetylsalicylic acid—Good or Bad! This is aspirin (a painkiller and blood-thinning agent, can be good for you or can cause more problems than it solves, depending on your personal medical situation. If in doubt, check with your doctor)
- Acesulfame K—Generally Neutral! This is a sweetener that the body can’t metabolize, so it’s also not a source of potassium (despite containing potassium) and will generally do nothing. Unless you have an allergy to it, which is rare but is a thing.
- Sucralose—Neutral! This is technically a sugar (as is anything ending in -ose), but the body can’t metabolize it and processes it as a dietary fiber instead. We’d list it as good for that reason, but honestly, we doubt you’re eating enough sucralose to make a noticeable difference to your daily fiber intake.
- Sucrose—Bad! This is just plain sugar
Sometimes words that sound the same can ring alarm bells when they need not, for example there’s a big difference between:
- Potassium iodide (a good source of potassium and iodine)
- Potassium cyanide (the famous poison; 300mg will kill you; half that dose will probably kill you)
- Cyanocobalamine (Vitamin B12)
Let us know if there are particular additives (or particular medications) you’d like us to look at!
While for legal reasons we cannot give medical advice, talking about common contraindications (e.g., it’s generally advised to not take this with that, as one will stop the other from working, etc) is definitely something we could do.
For example! St. John’s Wort, very popular as a herbal mood-brightener, is on the list of contraindications for so many medications, including:
- Antidepressants
- Birth control pills
- Cyclosporine, which prevents the body from rejecting transplanted organs
- Some heart medications, including digoxin and ivabradine
- Some HIV drugs, including indinavir and nevirapine
- Some cancer medications, including irinotecan and imatinib
- Warfarin, an anticoagulant (blood thinner)
- Certain statins, including simvastatin
Q: As I am a retired nurse, I am always interested in new medical technology and new ways of diagnosing. I have recently heard of using the eyes to diagnose Alzheimer’s. When I did some research I didn’t find too much. I am thinking the information may be too new or I wasn’t on the right sites.
(this is in response to last week’s piece on lutein, eyes, and brain health)
We’d readily bet that the diagnostic criteria has to do with recording low levels of lutein in the eye (discernible by a visual examination of macular pigment optical density), and relying on the correlation between this and incidence of Alzheimer’s, but we’ve not seen it as a hard diagnostic tool as yet either—we’ll do some digging and let you know what we find! In the meantime, we note that the Journal of Alzheimer’s Disease (which may be of interest to you, if you’re not already subscribed) is onto this:
See also:
- Journal of Alzheimer’s Disease (mixture of free and paid content)
- Journal of Alzheimer’s Disease Reports (open access—all content is free)
Q: As to specific health topics, I would love to see someone address all these Instagram ads targeted to women that claim “You only need to ‘balance your hormones’ to lose weight, get ripped, etc.” What does this mean? Which hormones are they all talking about? They all seem to be selling a workout program and/or supplements or something similar, as they are ads, after all. Is there any science behind this stuff or is it mostly hot air, as I suspect?
Thank you for asking this, as your question prompted yesterday’s main feature, What Does “Balancing Your Hormones” Even Mean?
That’s a great suggestion also about addressing ads (and goes for health-related things in general, not just hormonal stuff) and examining their claims, what they mean, how they work (if they work!), and what’s “technically true but may
be misleading* cause confusion”*We don’t want companies to sue us, of course.
Only, we’re going to need your help for this one, subscribers!
See, here at 10almonds we practice what we preach. We limit screen time, we focus on our work when working, and simply put, we don’t see as many ads as our thousands of subscribers do. Also, ads tend to be targeted to the individual, and often vary from country to country, so chances are good that we’re not seeing the same ads that you’re seeing.
So, how about we pull together as a bit of a 10almonds community project?
- Step 1: add our email address to your contacts list, if you haven’t already
- Step 2: When you see an ad you’re curious about, select “share” (there is usually an option to share ads, but if not, feel free to screenshot or such)
- Step 3: Send the ad to us by email
We’ll do the rest! Whenever we have enough ads to review, we’ll do a special on the topic.
We will categorically not be able to do this without you, so please do join in—Many thanks in advance!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: