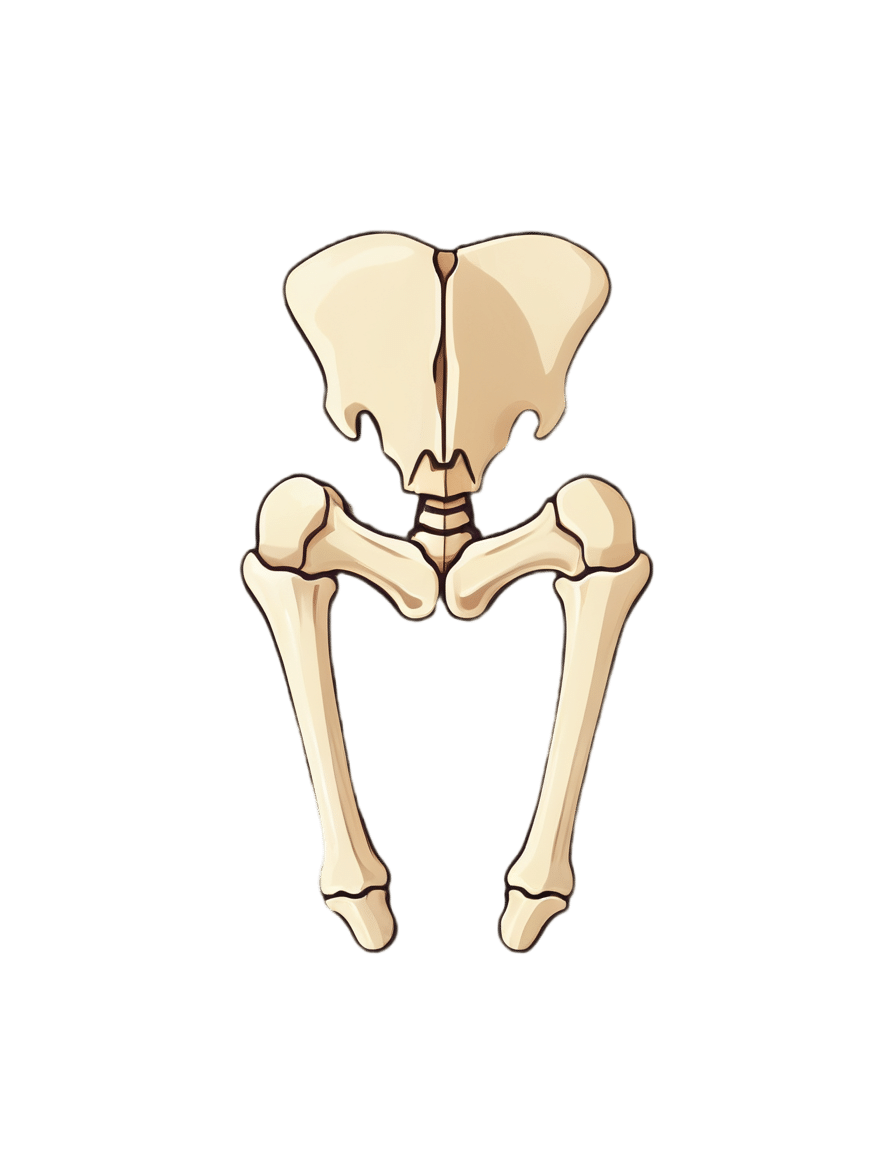
One Cause; Countless Aches
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What Is The Cause?
Zac Cupples’ video (below) makes an appealing claim: 90% of movement issues and discomforts we experience daily come from one source: reduced joint space due to increased muscle tension.
For Cupples, this could be causing anything from knee pain to foot pain to ankle pain to hip pain to generalized joint pain to…pretty much any sort of pain.
So, why do we describe this as “appealing”?
Well, if there’s just one cause, that means there is only one thing to fix
Can This Be True?
Whilst we normally stray away from oversimplifications, we found Cupples’ example quite powerful.
Cupples defends his thesis by illustrating it with a simple wrist movement experiment: try moving your wrist in a circle with your palm open, and then do the same with your fist clenched.
Did you notice a difference?
When you clench your fist, movement (normally) becomes restricted and uncomfortable, illustrating how increased tension limits joint space.
It’s a powerful analogy for understanding our body’s mechanics.
So How Do We Fix It?
To combat issues with reduced joint space, Cupples proposes a three-step solution: reducing muscle tension, increasing range of motion in commonly limited areas, and enhancing movement efficiency. He delves into strategies for achieving these, including adopting certain positions and breathing techniques.
There are also some elements of strategic muscle engagement, but we’ll leave that to him to describe:
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Glutathione: More Than An Antioxidant
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Glutathione’s Benefits: The Usual And The Unique
Glutathione is a powerful antioxidant that does all the things we might reasonably expect an antioxidant to do, plus some beneficial quirks of its own.
We do make glutathione in our bodies, but we can also get it from our diet, and of course, we can also supplement it.
What foods is it in?
It’s in a lot of foods, but some top examples include:
- turmeric
- avocado
- asparagus
- almonds
- cruciferous vegetables
- watermelon
- garlic
For a fuller list and discussion, see:
What does it do?
Let’s start with the obvious; as with most things that are antioxidant, it is also anti-inflammatory. Increasing or decreasing glutathione levels is associated with decreased or increased inflammation, respectively. For example:
It being anti-inflammatory also means it can be beneficial in calming autoimmune disorders:
Glutathione: a key player in autoimmunity
And to complete the triad of “those three things that generally go together”, yes, this means it also has anticancer potential, but watch out!
❝Although in healthy cells [glutathione] is crucial for the removal and detoxification of carcinogens, elevated [glutathione] levels in tumor cells are associated with tumor progression and increased resistance to chemotherapeutic drugs❞
~ Dr. Miroslava Cuperlovic-Culf et al.
Read in full: Role of Glutathione in Cancer: From Mechanisms to Therapies
So in other words, when it comes to cancer risk management, glutathione is a great preventative, but the opposite of a cure.
What were those “beneficial quirks of its own”?
They are mainly twofold, and the first is that it improves insulin sensitivity. There are many studies showing this, but here’s a recent one from earlier this year:
The Role of Glutathione and Its Precursors in Type 2 Diabetes
The other main “beneficial quirk of its own” is that it helps prevent and/or reverse non-alcoholic fatty liver disease, as in this study from last year:
Because of glutathione’s presence in nuts, fruits, and vegetables, this makes it a great thing to work in tandem with a dietary approach to preventing/reversing NAFLD, by the way:
Anything else?
It’s being investigated as a potential treatment for Parkinson’s disease symptoms, but the science is young for this one, so there is no definitive recommendation yet in this case. If you’re interested in that, though, do check out the current state of the science at:
Potential use of glutathione as a treatment for Parkinson’s disease
Is it safe?
While there is no 100% blanket statement of safety that can ever be made about anything (even water can kill people, and oxygen ultimately kills everyone that something else doesn’t get first), glutathione has one of the safest general safety profiles possible, with the exception we noted earlier (if you have cancer, it is probably better to skip this one unless an oncologist or similar advises you otherwise).
As ever, do speak with your doctor/pharmacist to be sure in any case, though!
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
-
Lobster vs Crab – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing lobster to crab, we picked the crab.
Why?
Generally speaking, most seafood is healthy in moderation (assuming it’s well-prepared, not poisonous, and you don’t have an allergy), and for most people, these two sea creatures are indeed considered a reasonable part of a healthy balanced diet.
In terms of macros, they’re comparable in protein, and technically crab has about 2x the fat, but in both cases it’s next to nothing, so 2x almost nothing is still almost nothing. And, if we break down the lipids profiles, crab has a sufficiently smaller percentage of saturated fat (compared to monounsaturated and polyunsaturated), that crab actually has less saturated fat than lobster. In balance, the category of macros is either a tie or a slight win for crab, depending on your personal priorities.
When it comes to vitamins, crab wins easily with more of vitamins A, B1, B2, B6, B9, B12, and C, in most cases by considerable margins (we’re talking multiples of what lobster has). Lobster, meanwhile, has more of vitamin B3 (tiny margin) and vitamin B5 (pantothenic acid, as in, the vitamin that’s in basically everything edible, and thus almost impossible to be deficient in unless literally starving).
The minerals scene is more balanced; lobster has more calcium, copper, manganese, and selenium, while crab has more iron, magnesium, phosphorus, potassium, and zinc. The margins are comparable from one creature to another, so all in all the 4:5 score means a modest win for crab.
Both of these creatures are good sources of omega-3 fatty acids, but crab is better.
Lobster and crab are both somewhat high in cholesterol, but crab is the relatively lower of the two.
In short: for most people most of the time, both are fine to enjoy in moderation, but if picking one, crab is the healthier by most metrics.
Want to learn more?
You might like to read:
Shrimp vs Caviar – Which is Healthier?
Take care!
Share This Post
-
How Useful Is Hydrotherapy?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hyyyyyyydromatic…
Hydrotherapy is a very broad term, and refers to any (external) use of water as part of a physical therapy. Today we’re going to look at some of the top ways this can be beneficial—maybe you’ll know them all already, but maybe there’s something you hadn’t thought about or done decently; let’s find out!
Notwithstanding the vague nature of the umbrella term, some brave researchers have done a lot of work to bring us lots of information about what works and what doesn’t, so we’ll be using this to guide us today. For example:
Scientific Evidence-Based Effects of Hydrotherapy on Various Systems of the Body
Swimming (and similar)
An obvious one, this can for most people be a very good full-body exercise, that’s exactly as strenuous (or not) as you want/need it to be.
It can be cardio, it can be resistance, it can be endurance, it can be high-intensity interval training, it can be mobility work, it can be just support for an aching body that gets to enjoy being in the closest to zero-gravity we can get without being in freefall or in space.
See also: How To Do HIIT (Without Wrecking Your Body)
Depending on what’s available for you locally (pool with a shallow area, for example), it can also be a place to do some exercises normally performed on land, but with your weight being partially supported (and as a counterpoint, a little resistance added to movement), and no meaningful risk of falling.
Tip: check out your local facilities, to see if they offer water aerobics classes; because the water necessitates slow movement, this can look a lot like tai chi to watch, but it’s great for mobility and balance.
Water circuit therapy
This isn’t circuit training! Rather, it’s a mixture of thermo- and cryotherapy, that is to say, alternating warm and cold water immersion. This can also be interspersed with the use of a sauna, of course.
See also:
- Ice Baths: To Dip Or Not To Dip?
- Saunas: Health Benefits (& Caveats)
- The Stress Prescription (Against Aging!)
this last one is about thermal shock-mediated hormesis, which sounds drastic, but it’s what we’re doing here with the hot and cold, and it’s good for most people!
Pain relief
Most of the research for this has to do with childbirth pain rather than, for example, back pain, but the science is promising:
Post-exercise recovery
It can be tempting to sink into a hot bath, or at least enjoy a good hot shower, after strenuous exercise. But does it help recovery too? The answer is probably yes:
Effect of hot water immersion on acute physiological responses following resistance exercise
For more on that (and other means of improving post-exercise recovery), check out our previous main feature:
How To Speed Up Recovery After A Workout (According To Actual Science)
Take care!
Share This Post
Related Posts
-
5 Things To Know About Passive Suicidal Ideation
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’ve ever wanted to go to sleep and never wake up, or have some accident/incident/illness take you with no action on your part, or a loved one has ever expressed such thoughts/feelings to you… Then this video is for you. Dr. Scott Eilers explains:
Tired of living
We’ll not keep them a mystery; here are the five things that Dr. Eilers wants us to know about passive suicidal ideation:
- What it is: a desire for something to end your life without taking active steps. While it may seem all too common, it’s not necessarily inevitable or unchangeable.
- What it means in terms of severity: it isn’t a clear indicator of how severe someone’s depression is. It doesn’t necessarily mean that the person’s depression is mild; it can be severe even without active suicidal thoughts, or indeed, suicidality at all.
- What it threatens: although passive suicidal ideation doesn’t usually involve active planning, it can still be dangerous. Over time, it can evolve into active suicidal ideation or lead to risky behaviors.
- What it isn’t: passive suicidal ideation is different from intrusive thoughts, which are unwanted, distressing thoughts about death. The former involves a desire for death, while the latter does not.
- What it doesn’t have to be: passive suicidal ideation is often a symptom of underlying depression or a mood disorder, which can be treated through therapy, medication, or a combination of both. Seeking treatment is crucial and can be life-changing.
For more on all of the above, here’s Dr. Eilers with his own words:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- The Mental Health First Aid You’ll Hopefully Never Need ← about depression generally
- How To Stay Alive (When You Really Don’t Want To) ← about suicidality specifically
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tomatoes vs Carrots – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing tomatoes to carrots, we picked the carrots.
Why?
Both known for being vitamin-A heavyweights, there is nevertheless a clear winner:
In terms of macros, carrots have a little over 2x the carbs, and/but also a little over 2x the fiber, so we consider category this a win for carrots.
In the category of vitamins, tomatoes have more vitamin C, while carrots have more of vitamins A, B1, B2, B3, B5, B6, B9, E, K, and choline. And about that vitamin A specifically: carrots have over 20x the vitamin A of tomatoes. An easy win for carrots here!
When it comes to minerals, tomatoes have a little more copper, while carrots have more calcium, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. Another clear win for carrots.
Looking at polyphenols, carrots are good but tomatoes have more, including a good healthy dose of quercetin; they also have more lycopene, not technically a polyphenol by virtue of its chemical structure (it’s a carotenoid), but a powerful phytochemical nonetheless (and much more prevalent in sun-dried tomatoes, in any case, which is not what we were looking at today—perhaps another day we’ll do sun-dried tomatoes and carrots head-to-head!).
Still, a) carrots are not short of carotenoids either (including lycopene), and b) we don’t think the moderate win on polyphenols is enough to outdo carrots having won all the other categories.
All in all, carrots win the day, but of course, do enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Lycopene’s Benefits For The Gut, Heart, Brain, & More
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Calm For Surgery – by Dr Chris Bonney
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As a general rule of thumb, nobody likes having surgery. We may like the results of the surgery, we may like having the surgery done and behind us, but surgery itself is not most people’s idea of fun, and honestly, the recovery period afterwards can be a pain in every sense of the word.
Dr. Chris Bonney, an anesthesiologist, gives us the industry-secrets low-down, and is the voice of experience when it comes to the things to know about and/or prepare in advance—the little things that make a world of difference to your in-hospital experience and afterwards.
Think of it like “frequent flyer traveller tips” but for surgeries, whereupon knowing a given tip can mean the difference between deeply traumatic suffering and merely not being at your usual best. We think that’s worth it.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: