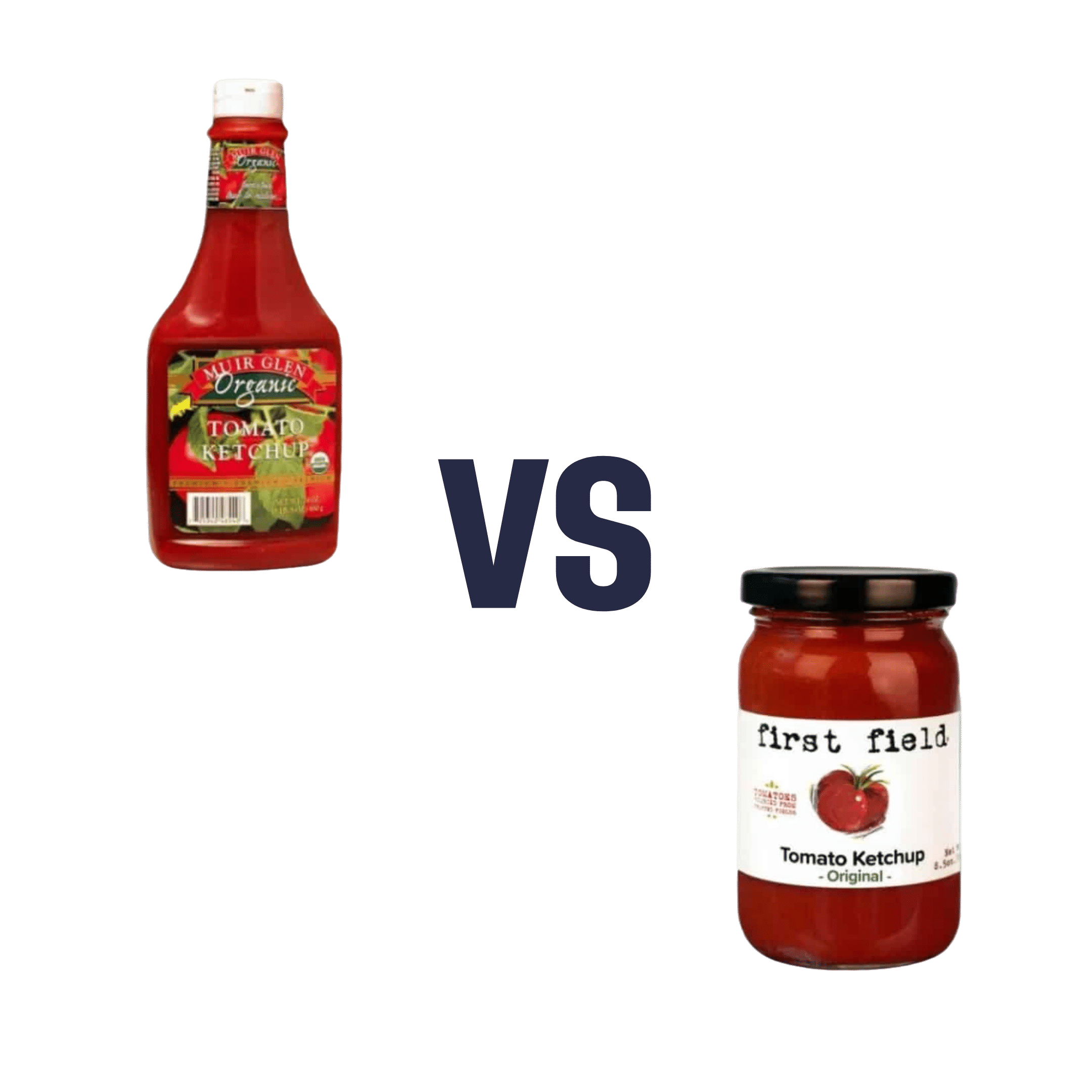
Muir Glen Organic vs First Field Original – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Muir Glen Organic Ketchup to First Field Original Ketchup, we picked the First Field.
Why?
This one was a little unfair to you, as you can’t turn them around to read the ingredients here. But the point we want to share the most today is: you have to turn them around and read the ingredients! You absolutely cannot rely on appearances!
While the Muir Glen Organic may have a very “greenwashed” aesthetic going on and the word “organic” is more eye-catching than any other word on the label, it contains 4x as much sugar and 4x as much sodium.
Side-by-side, they have, per tablespoon:
First Field Original: 1g sugar, 60mg sodium
Muir Glen Organic: 4g sugar, 240mg sodium
But what about the importance of being organic?
Well, we have one more surprise for you: the First Field ketchup is organic too, non-GMO, and contains no added concentrates either.
This isn’t an ad for First Field (by all means enjoy their products or don’t; we’re not invested), but it is a heartfelt plea to always check the backs of products and read the labels, because fronts of products can’t be relied upon at all.
I’m sure we all get caught out sometimes, but the less often, the better!
PS: we write this, of course, before seeing the results of your voting. Maybe it won’t be a “Muir Glen Organic” sweep in the polls. But either way, it’s a call to vigilance, and a “very good, carry on” to everyone who does this already
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why do I need to take some medicines with food?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever been instructed to take your medicine with food and wondered why? Perhaps you’ve wondered if you really need to?
There are varied reasons, and sometimes complex science and chemistry, behind why you may be advised to take a medicine with food.
To complicate matters, some similar medicines need to be taken differently. The antibiotic amoxicillin with clavulanic acid (sold as Amoxil Duo Forte), for example, is recommended to be taken with food, while amoxicillin alone (sold as Amoxil), can be taken with or without food.
Different brands of the same medicine may also have different recommendations when it comes to taking it with food.
Ron Lach/Pexels Food impacts drug absorption
Food can affect how fast and how much a drug is absorbed into the body in up to 40% of medicines taken orally.
When you have food in your stomach, the makeup of the digestive juices change. This includes things like the fluid volume, thickness, pH (which becomes less acidic with food), surface tension, movement and how much salt is in your bile. These changes can impair or enhance drug absorption.
Eating a meal also delays how fast the contents of the stomach move into the small intestine – this is known as gastric emptying. The small intestine has a large surface area and rich blood supply – and this is the primary site of drug absorption.
Eating a meal with medicine will delay its onset. Farhad/Pexels Eating a larger meal, or one with lots of fibre, delays gastric emptying more than a smaller meal. Sometimes, health professionals will advise you to take a medicine with food, to help your body absorb the drug more slowly.
But if a drug can be taken with or without food – such as paracetamol – and you want it to work faster, take it on an empty stomach.
Food can make medicines more tolerable
Have you ever taken a medicine on an empty stomach and felt nauseated soon after? Some medicines can cause stomach upsets.
Metformin, for example, is a drug that reduces blood glucose and treats type 2 diabetes and polycystic ovary syndrome. It commonly causes gastrointestinal symptoms, with one in four users affected. To combat these side effects, it is generally recommended to be taken with food.
The same advice is given for corticosteroids (such as prednisolone/prednisone) and certain antibiotics (such as doxycycline).
Taking some medicines with food makes them more tolerable and improves the chance you’ll take it for the duration it’s prescribed.
Can food make medicines safer?
Ibuprofen is one of the most widely used over-the-counter medicines, with around one in five Australians reporting use within a two-week period.
While effective for pain and inflammation, ibuprofen can impact the stomach by inhibiting protective prostaglandins, increasing the risk of bleeding, ulceration and perforation with long-term use.
But there isn’t enough research to show taking ibuprofen with food reduces this risk.
Prolonged use may also affect kidney function, particularly in those with pre-existing conditions or dehydration.
The Australian Medicines Handbook, which guides prescribers about medicine usage and dosage, advises taking ibuprofen (sold as Nurofen and Advil) with a glass of water – or with a meal if it upsets your stomach.
If it doesn’t upset your stomach, ibuprofen can be taken with water. Tbel Abuseridze/Unsplash A systematic review published in 2015 found food delays the transit of ibuprofen to the small intestine and absorption, which delays therapeutic effect and the time before pain relief. It also found taking short courses of ibuprofen without food reduced the need for additional doses.
To reduce the risk of ibuprofen causing damage to your stomach or kidneys, use the lowest effective dose for the shortest duration, stay hydrated and avoid taking other non-steroidal anti-inflammatory medicines at the same time.
For people who use ibuprofen for prolonged periods and are at higher risk of gastrointestinal side effects (such as people with a history of ulcers or older adults), your prescriber may start you on a proton pump inhibitor, a medicine that reduces stomach acid and protects the stomach lining.
How much food do you need?
When you need to take a medicine with food, how much is enough?
Sometimes a full glass of milk or a couple of crackers may be enough, for medicines such as prednisone/prednisolone.
However, most head-to-head studies that compare the effects of a medicine “with food” and without, usually use a heavy meal to define “with food”. So, a cracker may not be enough, particularly for those with a sensitive stomach. A more substantial meal that includes a mix of fat, protein and carbohydrates is generally advised.
Your health professional can advise you on which of your medicines need to be taken with food and how they interact with your digestive system.
Mary Bushell, Clinical Associate Professor in Pharmacy, University of Canberra
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Willpower: A Muscle To Flex, Or Spoons To Conserve?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Willpower: A Muscle To Flex, Or Spoons To Conserve?
We have previously written about motivation; this one’s not about that.
Rather, it’s about willpower itself, and especially, the maintenance of such. Which prompts the question…
Is willpower something that can be built up through practice, or something that is a finite resource that can be expended?
That depends on you—and your experiences.
- Some people believe willpower is a metaphorical “muscle” that must be exercised to be built up
- Some people believe willpower is a matter of metaphorical “spoons” that can be used up
A quick note on spoon theory: this traces its roots to Christine Miserandino’s 2003 essay about chronic illness and the management of limited energy. She details how she explained this to a friend in a practical fashion, she gave her a bunch of spoons from her kitchen, as an arbitrary unit of energy currency. These spoons would then need to be used to “pay” for tasks done; soon her friend realised that if she wanted to make it through the day, she was going to have to give more forethought to how she would “spend” her spoons, or she’d run out and be helpless (and perhaps hungry and far from home) before the day’s end. So, the kind of forethought and planning that a lot of people with chronic illnesses have to give to every day’s activities.
You can read it here: But You Don’t Look Sick? The Spoon Theory
So, why do some people believe one way, and some believe the other? It comes down to our experiences of our own willpower being built or expended. Researchers (Dr. Vanda Siber et al.) studied this, and concluded:
❝The studies support the idea that what people believe about willpower depends, at least in part, on recent experiences with tasks as being energizing or draining.❞
Source: Autonomous Goal Striving Promotes a Nonlimited Theory About Willpower
In other words, there’s a difference between going out running each morning while healthy, and doing so with (for example) lupus.
On a practical level, this translates to practicable advice:
- If something requires willpower but is energizing, this is the muscle kind! Build it.
- If something requires willpower and is draining, this is the spoons kind! Conserve it.
Read the above two bullet-points as many times as necessary to cement them into your hippocampus, because they are the most important message of today’s newsletter.
Do you tend towards the “nonlimited” belief, despite getting tired? If so, here’s why…
There is something that can continue to empower us even when we get physically fatigued, and that’s the extent to which we truly get a choice about what we’re doing. In other words, that “Autonomous” at the front of the title of the previous study, isn’t just word salad.
- If we perceive ourselves as choosing to do what we are doing, with free will and autonomy (i.e., no externally created punitive consequences), we will feel much more empowered, and that goes for our willpower too.
- If we perceive ourselves as doing what we have to (or suffer the consequences), we’ll probably do it, but we’ll find it draining, and that goes for our willpower too.
Until such a time as age-related physical and mental decline truly take us, we as humans tend to gradually accumulate autonomy in our lives. We start as literal babies, then are children with all important decisions made for us, then adolescents building our own identity and ways of doing things, then young adults launching ourselves into the world of adulthood (with mixed results), to a usually more settled middle-age that still has a lot of external stressors and responsibilities, to old age, where we’ve often most things in order, and just ourselves and perhaps our partner to consider.
Consequently…
Age differences in implicit theories about willpower: why older people endorse a nonlimited theory
…which explains why the 30-year-old middle-manager might break down and burn out and stop going to work, while an octogenarian is busy training for a marathon daily before getting back to their daily book-writing session, without fail.
One final thing…
If you need a willpower boost, have a snack*. If you need to willpower boost to avoid snacking, then plan for this in advance by finding a way to keep your blood sugars stable. Because…
The physiology of willpower: linking blood glucose to self-control
*Something that will keep your blood sugars stable, not spike them. Nuts are a great example, unless you’re allergic to such, because they have a nice balance of carbohydrates, protein, and healthy fats.
Want more on that? Read: 10 Ways To Balance Blood Sugars
Share This Post
-
You, Happier – by Dr. Daniel Amen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The implicit question “what’s your brain type?” makes this book sound a little like a horoscope for science-enjoyers, but really, the “brain type” in question is simply a way of expressing which neurochemicals one’s brain makes most and/or least easily.
That’s something that a) really does differ from one person to another b) isn’t necessarily fixed forever, but will tend to remain mostly the same most of the time for most people.
And yes, the book does cover figuring out which neurotransmitter(s) it might be for you. On a secondary level, it also talks about more/less active parts of the brain for each of us, but the primary focus is on neurotransmitters.
It’s easy to assume “everyone wants more [your favorite neurotransmitter here]” but in fact, most people most of the time have most of what they need.
For those of us who don’t, those of us who perhaps have to work more to keep our level(s) of one or more neurotransmitters where they should be, this book is a great guide to optimizing aspects of our diet and lifestyle to compensate for what our brains might lack—potentially reducing the need to go for pharmaceutical approaches.
The style of the book is very much pop-science, but it is all well-informed and well-referenced.
Bottom line: if you sometimes (or often!) think “if only my brain would just make/acknowledge more [neurotransmitter], this book is for you.
Click here to check out You, Happier, and discover a happier you!
Share This Post
Related Posts
-
Lime-Charred Cauliflower Popcorn
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Called “popcorn” for its appearance and tasty-snackness, this one otherwise bears little relation to the usual movie theater snack, and it’s both tastier and healthier. All that said, it can be eaten on its own as a snack (even with a movie, if you so wish), or served as one part of a many-dish banquet, or (this writer’s favorite) as a delicious appetizer that also puts down a healthy bed of fiber ready for the main course to follow it.
You will need
- 1 cauliflower, cut into small (popcorn-sized) florets
- 2 tbsp extra virgin olive oil
- 1 tbsp lime pickle
- 1 tsp cumin seeds
- 1 tsp smoked paprika
- 1 tsp chili flakes
- 1 tsp black pepper, coarse ground
- ½ tsp ground turmeric
Method
(we suggest you read everything at least once before doing anything)
1) Preheat your oven as hot as it will go
2) Mix all the ingredients in a small bowl except the cauliflower, to form a marinade
3) Drizzle the marinade over the cauliflower in a larger bowl (i.e. big enough for the cauliflower), and mix well until the cauliflower is entirely, or at least almost entirely, coated. Yes, it’s not a lot of marinade but unless you picked a truly huge cauliflower, the proportions we gave will be enough, and you want the end result to be crisp, not dripping.
4) Spread the marinaded cauliflower florets out on a baking tray lined with baking paper. Put it in the oven on the middle shelf, so it doesn’t cook unevenly, but keeping the temperature as high as it goes.
5) When it is charred and crispy golden, it’s done—this should take about 20 minutes, but we’ll say ±5 minutes depending on your oven, so do check on it periodically—and time to serve (it is best enjoyed warm).
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- We must do a main feature on the merits of cruciferous vegetables! Watch this space.
- All About Olive Oils (Extra Virgin & Otherwise)
- Capsaicin For Weight Loss And Against Inflammation
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Why Curcumin (Turmeric) Is Worth Its Weight In Gold
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Aspirin vs Cancer Metastasis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aspirin is a bit of a mixed bag.
In the category of things in its favor, it’s a modest analgesic with few side effects from occasional use, so it’s a good option if you have a headache, for example.
Unless you’re already on blood thinners or having a bleeding disorder, in which case, aspirin is not the thing to reach for.
About aspirin and heart disease
This is actually a complicated one, and we covered it at length in a dedicated main feature. If you want a one-line summary, it’s “chronic low-dose aspirin use can lower overall CVD risk, but does not reduce CVD mortality or all-cause mortality, and you may pay for it with gastrointestinal bleeding, and increased risk of ulcers“.
For a more nuanced explanation, see: Aspirin, CVD Risk, & Potential Counter-Risks
On the other hand, if you are having a heart attack and are waiting for the ambulance that you already called, and have aspirin to hand that you don’t have to go looking for, then it can be good to take a dose then.
For more on that, see: How To Survive A Heart Attack When You’re Alone
There are more problems
In the case of chronic use of low-dose aspirin, not only does it increase the risks of bleeding, especially gastrointestinal bleeding, and ulcers, but also it increases the risk of anemia. Given that anemia also gives the symptom “dizziness”, this is also a significant threat for increasing the incidence of falls in the older population, too, which can of course lead to serious complications and ultimately death.
For the science about this, see: Low-Dose Aspirin & Anemia
Now, about aspirin and cancer metastasis
This one’s a point in aspirin’s favor.
Cancer is, in and of itself, obviously a big problem. In terms of when it’s most likely to kill someone, that is usually when the cancer becomes metastatic, that is to say, it has spread.
So, while preventing cancer and, failing that, killing cancer are very important goals, there is a third axis to cancer care, which is preventing metastasis in someone who has cancer.
And that’s what aspirin does. How, you ask?
Scientists found this one out by accident!
They were doing genetic research in mice, to find genes that had an effect on metastasis. In the process, they found a certain gene that instructs the creation of a certain protein, and mice that lacked that gene (and thus its associated protein) had less metastasis.
The protein in question suppresses T-cells, which are programmed to recognize and kill metastatic cancer cells (amongst having other great jobs; they are an important part of the immune system in general, and one that declines with aging; most people in their 60s or older are producing very few T-cells).
About that, see: Focusing On Health In Our Sixties
Tracing the cell signaling, the researchers found that the protein is activated when T-cells are exposed to thromboxane A2 (or TXA2 to its friends).
And TXA2? That’s produced by platelets, and aspirin works by inhibiting TXA2 production, effectively making platelets (and thus the blood as a whole) less sticky.
So, that’s quite a few steps in the process, but ultimately:
- Aspirin inhibits TXA2 production
- Lower TXA2 levels mean ARHGEF1 (that’s the protein) isn’t activated
- ARHGEF1 not being activated means T-cells are free to do their thing
- T-cells are now free to kill metastatic cancer cells
You can read the paper here:
Aspirin prevents metastasis by limiting platelet TXA2 suppression of T cell immunity
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Pain-Free Mindset – by Dr. Deepak Ravindran
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First: please ignore the terrible title. This is not the medical equivalent of “think and grow rich”. A better title would have been something like “The Pain-Free Plan”.
Attentive subscribers may notice that this author was our featured expert yesterday, so you can learn about his “seven steps” described in our article there, without us repeating that in our review here.
This book’s greatest strength is also potentially its greatest weakness, depending on the reader: it contains a lot of detailed medical information.
This is good or bad depending on whether you like lots of detailed medical information. Dr. Ravindran doesn’t assume prior knowledge, so everything is explained as we go. However, this means that after his well-referenced clinical explanations, high quality medical diagrams, etc, you may come out of this book feeling like you’ve just done a semester at medical school.
Knowledge is power, though, so understanding the underlying processes of pain and pain management really does help the reader become a more informed expert on your own pain—and options for reducing that pain.
Bottom line: this, disguised by its cover as a “think healing thoughts” book, is actually a science-centric, information-dense, well-sourced, comprehensive guide to pain management from one of the leading lights in the field.
Click here to check out The Pain-Free Mindset, and manage yours more comfortably!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: