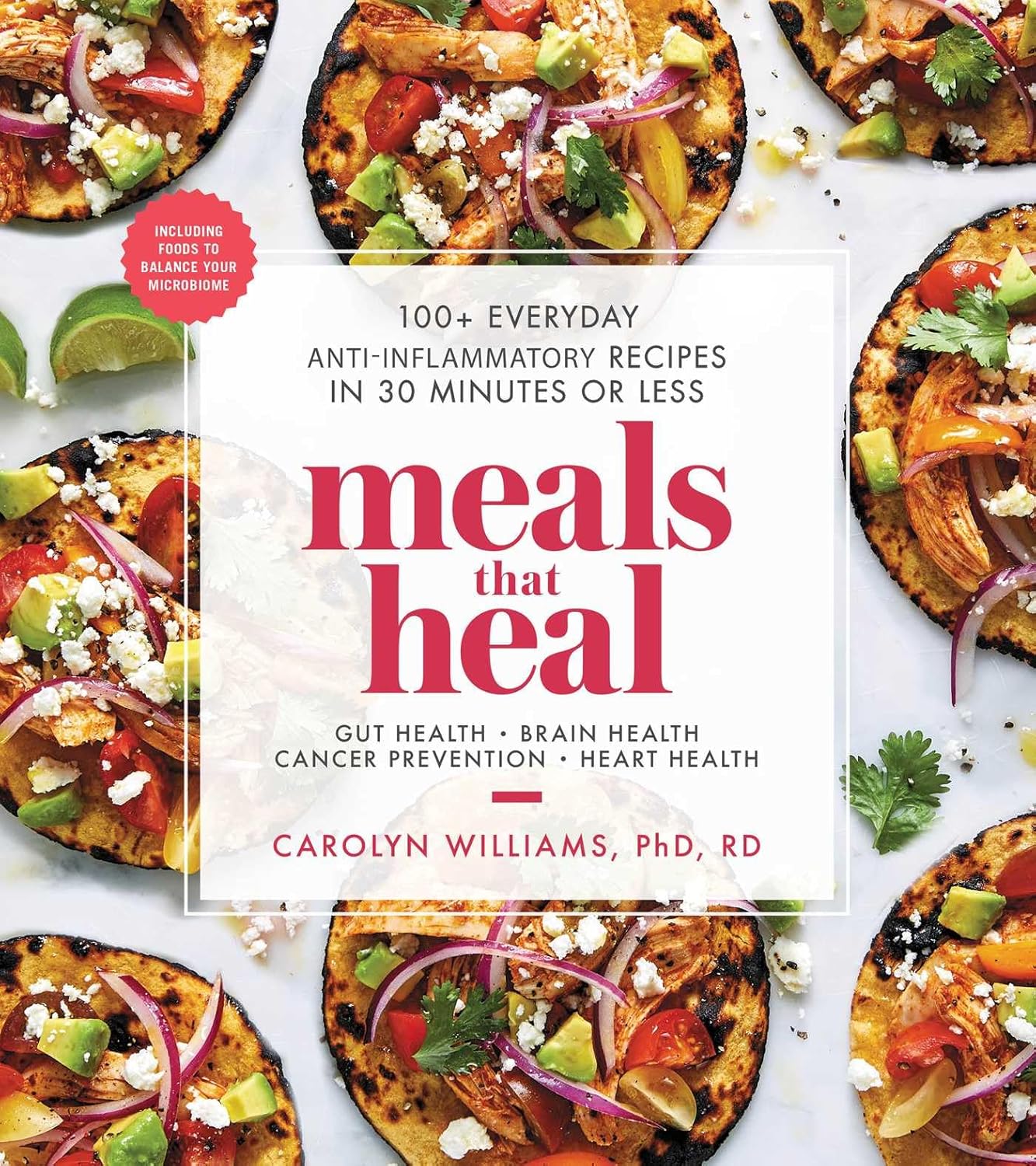
Meals That Heal – by Dr. Carolyn Williams
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Inflammation is implicated as a contributory or casual factor in almost all chronic diseases (and still exacerbates the ones in which it’s not directly implicated causally), so if there’s one area of health to focus on with one’s diet, then reducing inflammation is a top candidate.
This book sets about doing exactly that.
You may be wondering whether, per the book’s subtitle, they can really all be done in 30 minutes or under. The answer is: no, not unless you have a team of sous-chefs to do all the prep work for you, and line up everything mise-en-place style for when you start the clock. If you do have that team of sous-chefs working for you, then you can probably do most of them in under 30 minutes. If you don’t have that team, then budget about an hour in total, sometimes less, sometimes more, depending on the recipe.
The recipes themselves are mostly Mediterranean-inspired, though you might want to do a few swaps where the author has oddly recommended using seed oils instead of olive oil, or plant milk in place of where she has used dairy milk in a couple of “recipes” for smoothies. You might also want to be a little more generous with the seasonings, if you’re anything like this reviewer.
Bottom line: if you’re looking for an anti-inflammatory starter cookbook, you could do worse than this. You could probably do better, too, such as starting with The Inflammation Spectrum – by Dr. Will Cole.
Alternatively, click here if you want to check out Meals That Heal, and dive straight in!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Omega-3 Mushroom Spaghetti
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The omega-3 is not the only healthy fat in here; we’re also going to have medium-chain triglycerides, as well as monounsaturates. Add in the ergothioneine from the mushrooms and a stack of polyphenols from, well, most of the ingredients, not to mention the fiber, and this comes together as a very healthy dish. There’s also about 64g protein in the entire recipe, so you do the math for how much that is per serving, depending on how big you want the servings to be.
You will need
- 1lb wholewheat spaghetti (or gluten-free equivalent, such as a legume-based pasta, if avoiding gluten/wheat)
- 12oz mushrooms, sliced (any non-poisonous edible variety)
- ½ cup coconut milk
- ½ onion, finely chopped
- ¼ cup chia seeds
- ¼ bulb garlic, minced (or more, if you like)
- 2 tbsp extra virgin olive oil
- 1 tbsp black pepper, coarse ground
- 1 tbsp lime juice
Method
(we suggest you read everything at least once before doing anything)
1) Cook the spaghetti according to packet instructions, or your own good sense, aiming for al dente. When it’s done, drain it, and lastly rinse it (with cold water), and set it aside.
2) Heat the olive oil in a skillet and add the onion, cooking for 5 minutes
3) Add the garlic, mushrooms, and black pepper, cooking for another 8 minutes.
4) Add the coconut milk, lime juice, and chia seeds, stirring well and cooking for a further two minutes
5) Reheat the spaghetti by passing boiling water through it in a colander (the time it spent cold was good for it; it lowered the glycemic index)
6) Serve, adding the mushroom sauce to the spaghetti:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- The Magic of Mushrooms: “The Longevity Vitamin” (That’s Not A Vitamin)
- The Many Health Benefits of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- If You’re Not Taking Chia, You’re Missing Out
Take care!
Share This Post
-
Insomnia? High blood pressure? Try these!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Your Questions, Our Answers!
Q: Recipes for insomnia and high blood pressure and good foods to eat for these conditions?
A: Insomnia can be caused by many things, and consequently can often require a very multi-vector approach to fixing it. But, we’ll start by answering the question you asked (and probably address the rest of dealing with insomnia in another day’s edition!):
- First, you want food that’s easy to digest. Broadly speaking, this means plant-based. If not plant-based, fish (unless you have an allergy, obviously) is generally good and certainly better than white meat, which is better than red meat. In the category of dairy, it depends so much on what it is, that we’re not going to try to break it down here. If in doubt, skip it.
- You also don’t want blood sugar spikes, so it’s good to lay off the added sugar and white flour (or white flour derivatives, like white pasta), especially in your last meal of the day.
- Magnesium supports healthy sleep. A fine option would be our shchi recipe, but using collard greens rather than cabbage. Cabbage is a wonderful food, but collard greens are much higher in magnesium. Remember to add plenty of mushrooms (unless you don’t like them), as they’re typically high in magnesium too.
As for blood pressure, last month we gave tips (and a book recommendation) for heart health. The book, Dr. Monique Tello’s “Healthy Habits for Your Heart: 100 Simple, Effective Ways to Lower Your Blood Pressure and Maintain Your Heart’s Health”, also has recipes!
Here’s one from the “mains” section:
Secret Ingredient Baltimore-Style Salmon Patties with Not-Oily Aioli
❝This is a family favorite, and no one knows that it features puréed pumpkin! Most salmon cake recipes all for eggs and bread crumbs as binders, but puréed pumpkin and grated carrot work just as well, lend a beautiful color, and add plenty of fiber and plant nutrients. Canned salmon is way cheaper than fresh and has just as much omega-3 PUFAs and calcium. Serve this alongside a salad (the Summer Corn, Tomato, Spinach, and Basil Salad would go perfectly) for a well-rounded meal.❞
Serves 4 (1 large patty each)
Secret Ingredient Baltimore-Style Salmon Patties:
- 1 (15-oz) can pink salmon, no salt added
- ½ cup puréed pumpkin
- ½ cup grated carrot (I use a handheld box grater)
- 2 tablespoons minced chives (Don’t have chives? Minced green onions or any onions will do)
- 2 teaspoons Old Bay Seasoning
- 1 tablespoon olive oil
- ½ large lemon, sliced, for serving
Not-Oily Aioli:
- ½ cup plain low-fat Greek yogurt
- Juice and zest from ½ large lemon
- 1 clove garlic, crushed and minced fine
- 2 tablespoons chopped fresh dill
- For the patties: mix all the ingredients for the salmon patties together in a medium bowl
- Form patties with your hands and set on a plate or tray (you should have 4 burger-sized patties)
- Heat oil in a large skillet over medium heat.
- Set patties in a skillet and brown for 4 minutes, then carefully flip.
- Brown the other side, then serve hot.
- For the Aioli: mix all the ingredients for the aioli together in a small bowl.
- Plop a dollop alongside or on top of each salmon patty and serve with a spice of lemon.
Per serving: Calories: 367 | Fat: 13.6g | Saturated Fat: 4.4g | Protein: 46g | Sodium: 519mg | Carbohydrates: 13.2g | Fiber: 1.3g | Sugars: 9g | Calcium: 505mg | Iron: 1mg | Potassium 696mg
Notes from the 10almond team:
- If you want to make it plant-based, substitute cooked red lentils (no salt added) for the tinned salmon, and plant-based yogurt for the Greek yogurt
- We recommend adding more garlic. Seriously, who uses 1 clove of garlic for anything, let alone divided between four portions?
- The salads mentioned are given as recipes elsewhere in the same book. We strongly recommend getting her book, if you’re interested in heart health!
Do you have a question you’d like to see answered here? Hit reply or use the feedback widget at the bottom; we’d love to hear from you!
Share This Post
-
Gut Health 2.0
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Gene Expression & Gut Health
This is Dr. Tim Spector. After training in medicine and becoming a consultant rheumatologist, he’s turned his attention to medical research, and is these days a specialist in twin studies, genetics, epigenetics, microbiome, and diet.
What does he want us to know?
For one thing: epigenetics are for more than just getting your grandparents’ trauma.
More usefully: there are things we can do to improve epigenetic factors in our body
DNA is often seen as the script by which our body does whatever it’s going to do, but it’s only part of the story. Thinking of DNA as some kind of “magical immutable law of reality” overlooks (to labor the metaphor) script revisions, notes made in the margins, directorial choices, and ad-lib improvizations, as well as the quality of the audience’s hearing and comprehension.
Hence the premise of one of Dr. Spector’s older books, “Identically Different: Why We Can Change Our Genes”
(*in fact, it was his first, from all the way back in 2013, when he’d only been a doctor for 34 years)
Gene expression will trump genes every time, and gene expression is something that can often be changed without getting in there with CRISPR / a big pair of scissors and some craft glue.
How this happens on the micro level is beyond the scope of today’s article; part of it has to do with enzymes that get involved in the DNA transcription process, and those enzymes in turn are despatched or not depending on hormonal messaging—in the broadest sense of “hormonal”; all the body’s hormonal chemical messengers, not just the ones people think of as hormones.
However, hormonal messaging (of many kinds) is strongly influenced by something we can control relatively easily with a little good (science-based) knowledge: the gut.
The gut, the SAD, and the easy
In broad strokes: we know what is good for the gut. We’ve written about it before at 10almonds:
Making Friends With Your Gut (You Can Thank Us Later)
This is very much in contrast with what in scientific literature is often abbreviated “SAD”, the Standard American Diet, which is very bad for the gut.
However, Dr. Spector (while fully encouraging everyone to enjoy an evidence-based gut-healthy diet) wanted to do one better than just a sweeping one-size-fits-all advice, so he set up a big study with 15,000 identical twins; you can read about it here: TwinsUK
The information that came out of that was about a lot more than just gene expression and gut health, but it did provide the foundation for Dr. Spector’s next project, ZOE.
ZOE crowdsources huge amounts of data including individual metabolic responses to standardized meals in order to predict personalized food responses based on individual biology and unique microbiome profile.
In other words, it takes the guesswork out of a) knowing what your genes mean for your food responses b) tailoring your food choices with your genetic expression in mind, and c) ultimately creating a positive feedback loop to much better health on all levels.
Now, this is not an ad for ZOE, but if you so wish, you can…
- Get the free ZOE gut health guide (this is good, but generic, gut health information)
- Take the ZOE home gut health test (quiz followed by offers of lab tests)
- Browse the ZOE Health Academy, its education wing
Want to know more?
Dr. Spector has a bunch of books out, including some that we’ve reviewed previously:
- Spoon-Fed: Why Almost Everything We’ve Been Told About Food Is Wrong
- The Diet Myth: The Real Science Behind What We Eat
- Food for Life: The New Science of Eating Well
You can also check out our own previous main feature, which wasn’t about Dr. Spector’s work but was very adjacent:
The Brain-Gut Highway: A Two-Way Street
Enjoy!
Share This Post
Related Posts
-
The Brain Health Book – by Dr. John Randolph
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a clinical neuropsychologist and brain health consultant, brings his professional knowledge and understanding to bear on the questions of what works, what doesn’t, and why?
In practical terms, the focus is mostly on maintaining/improving attention, memory, and executive functions. To that end, he covers what kinds of exercises to do (physical and mental!), and examines what strategies make the most difference—including the usual lifestyle considerations of course, but also more specifically than that, what to prioritize over what when it comes to daily choices.
The style is easy pop-science, with an emphasis on being directly useful to the reader, rather than giving an overabundance of citations for everything as we go along. He does, however, explain the necessary science as we go, making the book educational without being academic.
Bottom line: if you’d like to maintain/improve your brain, this book can certainly help with that, and as a bonus (unless you are already an expert) you’ll learn plenty about the brain as you go.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
7 things you can do if you think you sweat too much
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sweating is our body’s way of cooling down, a bit like an internal air conditioner.
When our core temperature rises (because it’s hot outside, or you’re exercising), sweat glands all over our skin release a watery fluid. As that fluid evaporates, it takes heat with it, keeping us from overheating.
But sweating can vary from person to person. Some people might just get a little dewy under the arms, others feel like they could fill a swimming pool (maybe not that dramatic, but you get the idea).
So what’s a normal amount of sweat? And what’s too much?
ERIK Miheyeu/Shutterstock Why do some people sweat more than others?
How much you sweat depends on a number of factors including:
- your age (young kids generally sweat less than adults)
- your sex (men tend to sweat more than women)
- how active you are.
The average person sweats at the rate of 300 millilitres per hour (at 30°C and about 40% humidity). But as you can’t go around measuring the volume of your own sweat (or weighing it), doctors use another measure to gauge the impact of sweating.
They ask whether sweating interferes with your daily life. Maybe you stop wearing certain clothes because of the sweat stains, or feel embarrassed so don’t go to social events or work.
If so, this is a medical condition called hyperhidrosis, which affects millions of people worldwide.
People with this condition most commonly report problematic armpit sweating, as you’d expect. But sweaty hands, feet, scalp and groin can also be an issue.
Hyperhidrosis can be a symptom of another medical condition, such as an overactive thyroid, fever or menopause.
But hyperhidrosis can have no obvious cause, and the reasons behind this so-called primary hyperhidrosis are a bit of a mystery. People have normal numbers of sweat glands but researchers think they simply over-produce sweat after triggers such as stress, heat, exercise, tobacco, alcohol and hot spices. There may also be a genetic link.
OK, I sweat a lot. What can I do?
1. Antiperspirants
Antiperspirants, particularly ones with aluminium, are your first line of defence and are formulated to reduce sweating. Deodorants only stop body odour.
Aluminum chloride hexahydrate, aluminium chloride or the weaker aluminum zirconium tetrachlorohydrex glycinate react with proteins in the sweat glands, forming a plug. This plug temporarily blocks the sweat ducts, reducing the amount of sweat reaching the skin’s surface.
These products can contain up to 25% aluminium. The higher the percentage the better these products work, but the more they irritate the skin.
Make sure you’re buying antiperspirant and not deodorant. Okrasiuk/Shutterstock 2. Beat the heat
This might seem obvious, but staying cool can make a big difference. That’s because you have less heat to lose, so the body makes less sweat.
Avoid super-hot, long showers (you will have more heat to loose), wear loose-fitting clothes made from breathable fabrics such as cotton (this allows any sweat you do produce to evaporate more readily), and carry a little hand fan to help your sweat evaporate.
When exercising try ice bandanas (ice wrapped in a scarf or cloth, then applied to the body) or wet towels. You can wear these around the neck, head, or wrists to reduce your body temperature.
Try also to modify the time or place you exercise; try to find cool shade or air-conditioned areas when possible.
If you have tried these first two steps and your sweating is still affecting your life, talk to your doctor. They can help you figure out the best way to manage it.
3. Medication
Some medications can help regulate your sweating. Unfortunately some can also give you side effects such as a dry mouth, blurred vision, stomach pain or constipation. So talk to your doctor about what’s best for you.
Your GP may also refer you to a dermatologist – a doctor like myself who specialises in skin conditions – who might recommend different treatments, including some of the following.
4. Botulinum toxin injections
Botulinum toxin injections are not just used for cosmetic reasons. They have many applications in medicine, including blocking the nerves that control the sweat glands. They do this for many months.
A dermatologist usually gives the injections. But they’re only subsidised by Medicare in Australia for the armpits and if you have primary hyperhidrosis that hasn’t been controlled by the strongest antiperspirants. These injections are given up to three times a year. It is not subsidised for other conditions, such as an overactive thyroid or for other areas such as the face or hands.
If you don’t qualify, you can have these injections privately, but it will cost you hundreds of dollars per treatment, which can last up to six months.
Injections are available on Medicare in some cases. Satyrenko/Shutterstock 5. Iontophoresis
This involves using a device that passes a weak electrical current through water to the skin to reducing sweating in the hands, feet or armpits. Scientists aren’t sure exactly how it works.
But this is the only way to control sweating of the hands and feet that does not require drugs, surgery or botulinum toxin injections.
This treatment is not subsidised by Medicare and not all dermatologists provide it. However, you can buy and use your own device, which tends to be cheaper than accessing it privately. You can ask your dermatologist if this is the right option for you.
6. Surgery
There is a procedure to cut certain nerves to the hands that stop them sweating. This is highly effective but can cause sweating to occur elsewhere.
There are also other surgical options, which you can discuss with your doctor.
7. Microwave therapy
This is a newer treatment that zaps your sweat glands to destroy them so they can’t work any more. It’s not super common yet, and it is quite painful. It’s available privately in a few centres.
Michael Freeman, Associate Professor of Dermatology, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Kettlebell Swings Are Not What Most People Think They Are (They’re Better)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Commonly assumed to be mostly a shoulders-and-arms exercise, they’re actually mostly about the hips and core:
From the hips
Correctly executed kettlebell swings primarily strengthens muscles from the hamstrings and glutes the to abs and back; in other words, muscles whose strength is essential for power, posture, and injury prevention.
The core in particular is not to be underestimated, with deep stabilizing muscles supporting posture, balance, and movement. Strengthening these areas can also help reduce lower back pain.
How to do it correctly: start with your feet shoulder-width apart (this is important, if you like having knees) and grip the kettlebell with both hands. Hinge at your hips, lowering the kettlebell between your legs while keeping your back flat and core engaged. Then, drive your hips forward explosively to swing the kettlebell up to shoulder height before allowing it to return down with control. The most common mistake is using the arms to lift the kettlebell, but the real power should come from the hips to maximize benefits and prevent injury.
Example workout: 30 seconds of kettlebell swings followed by 30 seconds of rest, repeated for 10 sets. This 10-minute routine provides a full-body workout that builds strength and endurance. As you progress, you can increase the weight, duration, number of sets, etc.
Timeline of changes: within a few weeks of regular kettlebell swings, you should notice stronger glutes, better endurance, and improved posture. After a month, you may experience reduced lower back pain (if you had lower back pain) and more power in your everyday movements. By two to three months, visible muscle definition and fat loss are likely to become noticeable, along with increased overall strength.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Body Sculpting with Kettlebells for Women – by Lorna Kleidman
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: