Revealed: The Soviet Secret Recipe For Success That The CIA Admits Put The US To Shame
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Today’s edition of 10almonds brings you a blast from the past with a modern twist: an ancient Russian peasant food that became a Soviet staple, and today, is almost unknown in the West.
Before we get to that, let’s take a sneaky look at this declassified CIA memorandum from near the end of the Cold War:
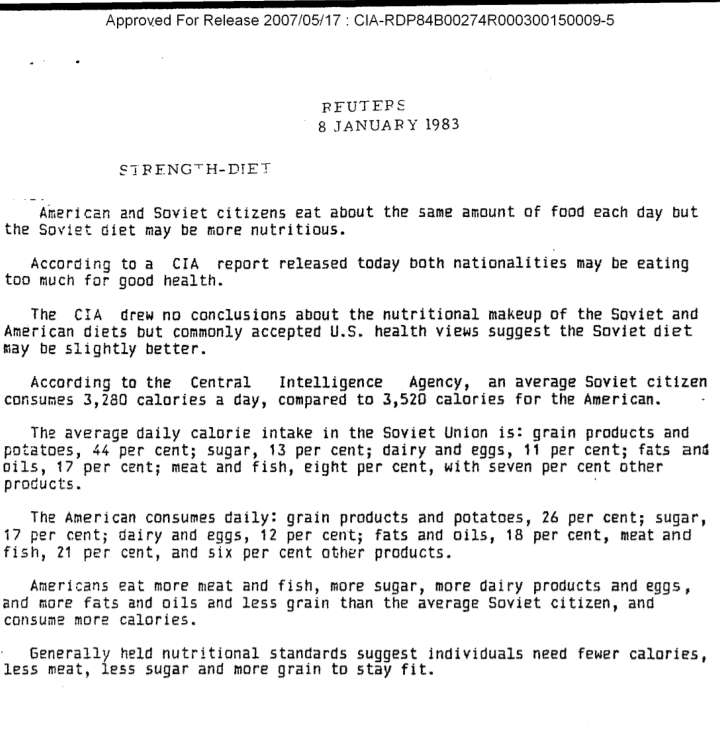
(Click here to see a bigger version)
The take-away here is:
- Americans were eating 2–3 times more meat than Soviets
- Soviets were eating nearly double the amount of grain products and potatoes
…and both of these statistics meant that nutritionally speaking, the Soviets were doing better.
Americans also consumed more sugar and fats, which again, wasn’t the best dietary option.
But was the American diet tastier? Depends on whom you ask.
Which brings us to a literal recipe we’re going to be sharing with you today:
It’s not well-known in the West, but in Russia, it’s a famous national comfort food, a bastion of health and nutrition, and it rose to popularity because it was not only cheap and nutritious, but also, you could eat it for days without getting sick of it. And it could be easily frozen for reheating later without losing any of its appeal—it’d still be just as good.
In Russia there are sayings about it:
Щи да каша — пища наша (Shchi da kasha — pishcha nasha)
“Shchi and buckwheat are what we eat”
Top tip: buckwheat makes an excellent (and naturally sweet) alternative to porridge oats if prepared the same way!
Где щи, там и нас ищи (Gdye shchi, tam i nas ishchi)
“Where there’s shchi, us you’ll see”
Голь голью, а луковка во щах есть (Gol’ gol’yu, a lukovka vo shchakh yest’)
“I’m stark naked, but there’s shchi with onions”
There’s a very strong sentiment in Russia that really, all you need is shchi (shchi, shchi… shchi is all you need )
But what, you may ask, is shchi?
Our culinary cultural ambassador Nastja is here to offer her tried-and-tested recipe for…

…Russian cabbage soup (yes, really—bear with us now, and you can thank us later)
There are a lot of recipes for shchi (see for yourself what the Russian version of Lifehacker recommends), and we’ll be offering our favorite…
Nastja’s Nutritious and Delicious Homemade Shchi
Hi, Nastja here! I’m going to share with you my shchi recipe that is:
- Cheap
- So tasty
- Super nutritious*
- Vegan
- Gluten Free
You will also need:
- A cabbage (I use sweetheart, but any white cabbage will do)
- 1 cup (250g) red lentils (other kinds of lentils will work too)
- ½ lb or so (250–300g) tomatoes (I use baby plum tomatoes, but any kind will do)
- ½ lb or so (250–300g) mushrooms (the edible kind)
- An onion (I use a brown onion; any kind will do)
- Salt, pepper, rosemary, thyme, parsley, cumin
- Marmite or similar yeast extract (do you hate it? Me too. Trust me, it’ll be fine, you’ll love it. Omit if you’re a coward.)
- A little oil for sautéing (I use sunflower, but canola is fine, as is soy oil. Do not use olive oil or coconut oil, because the taste is too strong and the flashpoint too low)
First, what the French call mise-en-place, the prep work:
- Chop the cabbage into small strips, ⅛–¼ inch x 1 inch is a good guideline, but you can’t really go wrong unless you go to extremes
- Chop the tomatoes. If you’re using baby plum tomatoes (or cherry tomatoes), cut them in half. If using larger tomatoes, cut them into eighths (halve them, halve the halves, then halve the quarters)
- Chop the mushrooms. If using button mushrooms, half them. If using larger mushrooms, quarter them.
- Chop the onion finely.
- Gather the following kitchenware: A big pan (stock pot or similar), a sauté pan (a big wok or frying pan will do), a small frying pan (here a wok will not do), and a saucepan (a rice cook will also do)
Now, for actual cooking:
- Cook the red lentils until soft (I use a rice cooker, but a saucepan is fine) and set aside
- Sauté the cabbage, put it in the big pot (not yet on the heat!)
- Fry the mushrooms, put them in the big pot (still not yet on the heat!)
When you’ve done this a few times and/or if you’re feeling confident, you can do the above simultaneously to save time
- Blend the lentils into the water you cooked them in, and then add to the big pot.
- Turn the heat on low, and if necessary, add more water to make it into a rich soup
- Add the seasonings to taste, except the parsley. Go easy on the cumin, be generous with the rosemary and thyme, let your heart guide you with the salt and pepper.
- When it comes to the yeast extract: add about one teaspoon and stir it into the pot. Even if you don’t like Marmite, it barely changes the flavour (makes it slightly richer) and adds a healthy dose of vitamin B12.
We did not forget the tomatoes and the onion:
- Caramelize the onion (keep an eye on the big pot) and set it aside
- Fry the tomatoes and add them to the big pot
Last but definitely not least:
- Serve!
- The caramelized onion is a garnish, so put a little on top of each bowl of shchi
- The parsley is also a garnish, just add a little
Any shchi you don’t eat today will keep in the fridge for several days, or in the freezer for much longer.
*That nutritious goodness I talked about? Check it out:
- Lentils are high in protein and iron
- Cabbage is high in vitamin C and calcium
- Mushrooms are high in magnesium
- Tomatoes are good against inflammation
- Black pepper has a host of health benefits
- Yeast extract contains vitamin B12
Let us know how it went! We love to receive emails from our subscribers!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Age-Proof Brain – by Dr. Marc Milstein
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Biological aging is not truly just one thing, but rather the amalgam of many things intersecting—and most of them are modifiable. The cells of your body neither know nor care how many times you have flown around the sun; they just respond to the stimuli they’re given.
Which is what fuels this book. The idea is to have a brain that is less-assailed by the things that would make it age, and more rejuvenated by the things that can make it biologically younger.
Dr. Milstein doesn’t neglect the rest of the body, and indeed notes the brain’s connections with the immune system, the heart, the gut, and more. But everything in this book is done with the brain in mind and its good health as the top priority outcome of all the things he advises.
On which note, yes, there is plenty of practical, implementable advice here. For a book that is consistently full of study paper citations, he does take care to make everything useful to the reader, and makes everything as easy as possible for the layperson along the way.
Bottom line: if you would like your brain to age less, this is an excellent, very evidence-based, guidebook.
Click here to check out The Age-Proof Brain, and age-proof your brain!
Share This Post
-
The Dopamine Precursor And More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What Is This Supplement “NALT”?
N-Acetyl L-Tyrosine (NALT) is a form of tyrosine, an amino acid that the body uses to build other things. What other things, you ask?
Well, like most amino acids, it can be used to make proteins. But most importantly and excitingly, the body uses it to make a collection of neurotransmitters—including dopamine and norepinephrine!
- Dopamine you’ll probably remember as “the reward chemical” or perhaps “the motivation molecule”
- Norepinephrine, also called noradrenaline, is what powers us up when we need a burst of energy.
Both of these things tend to get depleted under stressful conditions, and sometimes the body can need a bit of help replenishing them.
What does the science say?
This is Research Review Monday, after all, so let’s review some research! We’re going to dive into what we think is a very illustrative study:
A 2015 team of researchers wanted to know whether tyrosine (in the form of NALT) could be used as a cognitive enhancer to give a boost in adverse situations (times of stress, for example).
They noted:
❝The potential of using tyrosine supplementation to treat clinical disorders seems limited and its benefits are likely determined by the presence and extent of impaired neurotransmitter function and synthesis.❞
More on this later, but first, the positive that they also found:
❝In contrast, tyrosine does seem to effectively enhance cognitive performance, particularly in short-term stressful and/or cognitively demanding situations. We conclude that tyrosine is an effective enhancer of cognition, but only when neurotransmitter function is intact and dopamine and/or norepinephrine is temporarily depleted❞
That “but only”, is actually good too, by the way!
You do not want too much dopamine (that could cause addiction and/or psychosis) or too much norepinephrine (that could cause hypertension and/or heart attacks). You want just the right amount!
So it’s good that NALT says “hey, if you need some more, it’s here, if not, no worries, I’m not going to overload you with this”.
Read the study: Effect of tyrosine supplementation on clinical and healthy populations under stress or cognitive demands
About that limitation…
Remember they said that it seemed unlikely to help in treating clinical disorders with impaired neurotransmitter function and/or synthesis?
Imagine that you employ a chef in a restaurant, and they can’t keep up with the demand, and consequently some of the diners aren’t getting fed. Can you fix this by supplying the chef with more ingredients?
Well, yes, if and only if the problem is “the chef wasn’t given enough ingredients”. If the problem is that the oven (or the chef’s wrist) is broken, more ingredients aren’t going to help at all—something different is needed in those cases.
So it is with, for example, many cases of depression.
See for example: Tyrosine for depression: a double-blind trial
About blood pressure…
You may be wondering, “if NALT is a precursor of norepinephrine, a vasoconstrictor, will this increase my blood pressure adversely?”
Well, check with your doctor as your own situation may vary, but under normal circumstances, no. The effect of NALT is adaptogenic, meaning that it can help keep its relevant neurotransmitters at healthy levels—not too low or high.
See what we mean, for example in this study where it actually helped keep blood pressure down while improving cognitive performance under stress:
Effect of tyrosine on cognitive function and blood pressure under stress
Bottom line:
For most people, NALT is a safe and helpful way to help keep healthy levels of dopamine and norepinephrine during times of stress, giving cognitive benefits along the way.
Share This Post
-
Comfortable with Uncertainty – by Pema Chödrön
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is exactly what the subtitle claims it to be: 108 teachings on cultivating fearlessness and compassion. They are short extracts, entire of themselves, taken from Chödrön’s wider work and arranged to offer her insights and advices on this one topic, in one place.
It is worth noting, by the way, that the author is a Buddhist nun, and as such, the principles and practices are Buddhist in origin. If that’s a problem for you, then this book will not be for you. It does not, however, require that the reader be Buddhist to benefit, simply that one has a will to be calm in the face of chaos, and yet not indifferent—rather, to take on the challenges of life with a whole heart.
And about that compassion? This is about alleviating suffering; your own, and the suffering in the world as a whole, increasingly uncertain as this world is. And being brave enough to do that, in a world that is not always gentle.
The style is idiosyncratic, and you will likely love it or hate it. If you love it, then you will find this book at once both soothing and empowering; if not, you will put the book down and pick up a book on CBT or something instead.
Bottom line: this book absolutely does deliver on its title/subtitle promises—provided you, dear reader, internalize it and practise it.
Click here to check out Comfortable with Uncertainty, and get comfortable with uncertainty!
Share This Post
Related Posts
-
Mythbusting The Mask Debate
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mythbusting The Mask Debate
We asked you for your mask policy this respiratory virus season, and got the above-depicted, below-described, set of responses:
- A little under half of you said you will be masking when practical in indoor public places
- A little over a fifth of you said you will mask only if you have respiratory virus symptoms
- A little under a fifth of you said that you will not mask, because you don’t think it helps
- A much smaller minority of you (7%) said you will go with whatever people around you are doing
- An equally small minority of you said that you will not mask, because you’re not concerned about infections
So, what does the science say?
Wearing a mask reduces the transmission of respiratory viruses: True or False?
True…with limitations. The limitations include:
- The type of mask
- A homemade polyester single-sheet is not the same as an N95 respirator, for instance
- How well it is fitted
- It needs to be a physical barrier, so a loose-fitting “going through the motions” fit won’t help
- The condition of the mask
- And if applicable, the replaceable filter in the mask
- What exactly it has to stop
- What kind of virus, what kind of viral load, what kind of environment, is someone coughing/sneezing, etc
More details on these things can be found in the link at the end of today’s main feature, as it’s more than we could fit here!
Note: We’re talking about respiratory viruses in general in this main feature, but most extant up-to-date research is on COVID, so that’s going to appear quite a lot. Remember though, even COVID is not one beast, but many different variants, each with their own properties.
Nevertheless, the scientific consensus is “it does help, but is not a magical amulet”:
- 2021: Effectiveness of Face Masks in Reducing the Spread of COVID-19: A Model-Based Analysis
- 2022: Why Masks are Important during COVID‐19 Pandemic
- 2023: The mitigating effect of masks on the spread of COVID-19
Wearing a mask is actually unhygienic: True or False?
False, assuming your mask is clean when you put it on.
This (the fear of breathing more of one’s own germs in a cyclic fashion) was a point raised by some of those who expressed mask-unfavorable views in response to our poll.
There have been studies testing this, and they mostly say the same thing, “if it’s clean when you put it on, great, if not, then well yes, that can be a problem”:
❝A longer mask usage significantly increased the fungal colony numbers but not the bacterial colony numbers.
Although most identified microbes were non-pathogenic in humans; Staphylococcus epidermidis, Staphylococcus aureus, and Cladosporium, we found several pathogenic microbes; Bacillus cereus, Staphylococcus saprophyticus, Aspergillus, and Microsporum.
We also found no associations of mask-attached microbes with the transportation methods or gargling.
We propose that immunocompromised people should avoid repeated use of masks to prevent microbial infection.❞
Source: Bacterial and fungal isolation from face masks under the COVID-19 pandemic
Wearing a mask can mean we don’t get enough oxygen: True or False?
False, for any masks made-for-purpose (i.e., are by default “breathable”), under normal conditions:
- COVID‐19 pandemic: do surgical masks impact respiratory nasal functions?
- Performance Comparison of Single and Double Masks: Filtration Efficiencies, Breathing Resistance and CO2 Content
However, wearing a mask while engaging in strenuous best-effort cardiovascular exercise, will reduce VO₂max. To be clear, you will still have more than enough oxygen to function; it’s not considered a health hazard. However, it will reduce peak athletic performance:
…so if you are worrying about whether the mask will impede you breathing, ask yourself: am I engaging in an activity that requires my peak athletic performance?
Also: don’t let it get soaked with water, because…
Writer’s anecdote as an additional caveat: in the earliest days of the COVID pandemic, I had a simple cloth mask on, the one-piece polyester kind that we later learned quite useless. The fit wasn’t perfect either, but one day I was caught in heavy rain (I had left it on while going from one store to another while shopping), and suddenly, it fitted perfectly, as being soaked through caused it to cling beautifully to my face.
However, I was now effectively being waterboarded. I will say, it was not pleasant, but also I did not die. I did buy a new mask in the next store, though.
tl;dr = an exception to “no it won’t impede your breathing” is that a mask may indeed impede your breathing if it is made of cloth and literally soaked with water; that is how waterboarding works!
Want up-to-date information?
Most of the studies we cited today were from 2022 or 2023, but you can get up-to-date information and guidance from the World Health Organization, who really do not have any agenda besides actual world health, here:
Coronavirus disease (COVID-19): Masks | Frequently Asked Questions
At the time of writing this newsletter, the above information was last updated yesterday.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
5 Ways To Beat Cancer (And Other Diseases)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Systematic Approach To Healthy Eating
This is Dr. William Li. He’s a physician, cancer researcher, and educator. He also founded the Angiogenesis Foundation back in 1994.
We recently reviewed one of his books, “Eat To Beat Disease”.
He has another book that we haven’t reviewed at time of writing, “Eat To Beat Your Diet“, which you might like to check out.
What does he want us to know?
He wants us to know how to eat to beat cancer and other diseases, by means of five specific angles:
Angiogenesis
This is about replacing blood vessels, which of course happens all the time, but it becomes a problem when it is feeding a cancer in the process.
Here, based on Dr. Li’s work, is what can be done about it:
A List of Anti-Angiogenic Foods for a Cancer-Fighting Diet
Regeneration
Generally speaking, we want to replace healthy cells early, because if we wait until they get damaged, then that damage will be copied forwards. As well as intermittent fasting, there are other things we can do to promote this—even, Dr. Li’s research shows, for stem cells:
Doctor’s Tip: Regeneration (stem cells)—one of your body’s five defense systems
Microbiome health
Healthy gut, healthy rest of the body. We’ve written about this before:
Making Friends With Your Gut (You Can Thank Us Later)
DNA protection
DNA gets unravelled and damaged with age, the telomere caps get shorter, and mistakes get copied forward. So there more we can protect our DNA, the longer we can live healthily. There are many ways to do this, but Dr. Li was one of the first to bring to light the DNA-protecting benefits of kiwi fruit:
Immunity
Paradoxically, what’s good for your immune system (making it stronger) also helps to protect against autoimmune diseases (for most people, for the most part).
In short: it’s good to have an immune system that’s powerful not just in its counterattacks, but also in its discerning nature. There are dietary and other lifestyle approaches to both, and they’re mostly the same things:
Beyond Supplements: The Real Immune-Boosters!
and thus see also:
Want to know more?
You might enjoy his blog or podcast, and here’s his TED talk:
Want to watch it, but not right now? Bookmark it for later
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
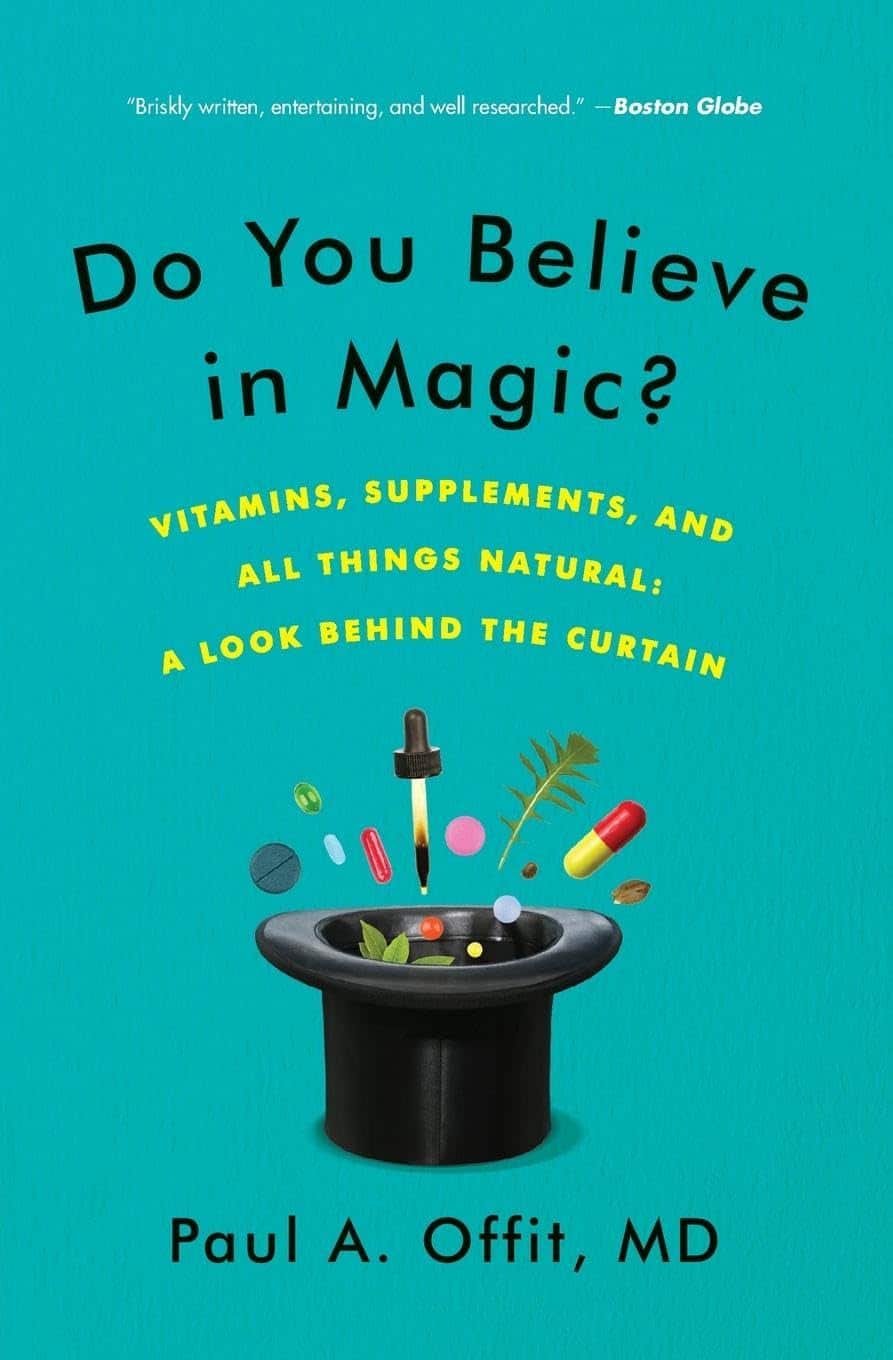
Do You Believe In Magic? – by Dr. Paul Offit
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Here at 10almonds, we like to examine and present the science wherever it leads, so this book was an interesting read.
Dr. Offit, himself a much-decorated vaccine research scientist, and longtime enemy of the anti-vax crowd, takes aim at alternative therapies in general, looking at what does work (and how), and what doesn’t (and what harm it can cause).
The style of the book is largely polemic in tone, but there’s lots of well-qualified information and stats in here too. And certainly, if there are alternative therapies you’ve left unquestioned, this book will probably prompt questions, at the very least.
And science, of course, is about asking questions, and shouldn’t be afraid of such! Open-minded skepticism is a key starting point, while being unafraid to actually reach a conclusion of “this is probably [not] so”, when and if that’s where the evidence brings us. Then, question again when and if new evidence comes along.
To that end, Dr. Offit does an enthusiastic job of looking for answers, and presenting what he finds.
If the book has downsides, they are primarily twofold:
- He is a little quick to dismiss the benefits of a good healthy diet, supplemented or otherwise.
- His keenness here seems to step from a desire to ensure people don’t skip life-saving medical treatments in the hope that their diet will cure their cancer (or liver disease, or be it what it may), but in doing so, he throws out a lot of actually good science.
- He—strangely—lumps menopausal HRT in with alternative therapies, and does the exact same kind of anti-science scaremongering that he rails against in the rest of the book.
- In his defence, this book was published ten years ago, and he may have been influenced by a stack of headlines at the time, and a popular celebrity endorsement of HRT, which likely put him off it.
Bottom line: there’s something here to annoy everyone—which makes for stimulating reading.
Click here to check out Do You Believe In Magic, and expand your knowledge!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- He is a little quick to dismiss the benefits of a good healthy diet, supplemented or otherwise.