How stigma perpetuates substance use
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In 2022, 54.6 million people 12 and older in the United States needed substance use disorder (SUD) treatment. Of those, only 24 percent received treatment, according to the most recent National Survey on Drug Use and Health.
SUD is a treatable, chronic medical condition that causes people to have difficulty controlling their use of legal or illegal substances, such as alcohol, tobacco, prescription opioids, heroin, methamphetamine, or cocaine. Using these substances may impact people’s health and ability to function in their daily life.
While help is available for people with SUD, the stigma they face—negative attitudes, stereotypes, and discrimination—often leads to shame, worsens their condition, and keeps them from seeking help.
Read on to find out more about how stigma perpetuates substance use.
Stigma can keep people from seeking treatment
Suzan M. Walters, assistant professor at New York University’s Grossman School of Medicine, has seen this firsthand in her research on stigma and health disparities.
She explains that people with SUD may be treated differently at a hospital or another health care setting because of their drug use, appearance (including track marks on their arms), or housing situation, which may discourage them from seeking care.
“And this is not just one case; this is a trend that I’m seeing with people who use drugs,” Walters tells PGN. “Someone said, ‘If I overdose, I’m not even going to the [emergency room] to get help because of this, because of the way I’m treated. Because I know I’m going to be treated differently.’”
People experience stigma not only because of their addiction, but also because of other aspects of their identities, Walters says, including “immigration or race and ethnicity. Hispanic folks, brown folks, Black folks [are] being treated differently and experiencing different outcomes.”
And despite the effective harm reduction tools and treatment options available for SUD, research has shown that stigma creates barriers to access.
Syringe services programs, for example, provide infectious disease testing, Narcan, and fentanyl test strips. These programs have been proven to save lives and reduce the spread of HIV and hepatitis C. SSPs don’t increase crime, but they’re often mistakenly “viewed by communities as potential settings of drug-related crime;” this myth persists despite decades of research proving that SSPs make communities safer.
To improve this bias, Walters says it’s helpful for people to take a step back and recognize how we use substances, like alcohol, in our own lives, while also humanizing those with addiction. She says, “There’s a lack of understanding that these are human beings and people … [who] are living lives, and many times very functional lives.”
Misconceptions lead to stigma
SUD results from changes in the brain that make it difficult for a person to stop using a substance. But research has shown that a big misconception that leads to stigma is that addiction is a choice and reflects a person’s willpower.
Michelle Maloney, executive clinical director of mental health and addiction recovery services for Rogers Behavioral Health, tells PGN that statements such as “you should be able to stop” can keep a patient from seeking treatment. This belief goes back to the 1980s and the War on Drugs, she adds.
“We think about public service announcements that occurred during that time: ‘Just say no to drugs,’” Maloney says. “People who have struggled, whether that be with nicotine, alcohol, or opioids, [know] it’s not as easy as just saying no.”
Stigma can worsen addiction
Stigma can also lead people with SUD to feel guilt and shame and blame themselves for their medical condition. These feelings, according to the National Institute on Drug Abuse, may “reinforce drug-seeking behavior.”
In a 2020 article, Dr. Nora D. Volkow, the director of NIDA, said that “when internalized, stigma and the painful isolation it produces encourage further drug taking, directly exacerbating the disease.”
Overall, research agrees that stigma harms people experiencing addiction and can make the condition worse. Experts also agree that debunking myths about the condition and using non-stigmatizing language (like saying someone is a person with a substance use disorder, not an addict) can go a long way toward reducing stigma.
Resources to mitigate stigma:
- CDC: Stigma Reduction
- National Harm Reduction Coalition: Respect To Connect: Undoing Stigma
- NIDA:
- Shatterproof: Addiction language guide (Disclosure: The Public Good Projects, PGN’s parent company, is a Shatterproof partner)
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ozempic vs Five Natural Supplements
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Semaglutide (GLP-1 agonist) drugs Ozempic and Wegovy really do work for losing weight, provided one then remains on these expensive drugs for life. Dr. Jin Sung recommends a supplements-based approach, instead.
Natural Alternatives
Dr. Sung recommends:
- Berberine, which increases production and secretion of GLP-1.
- Probiotics, which increase GLP-1 secretion. In particular he recommends Akkermansia municiphila which secretes P9, and this protein stimulates GLP-1 production and secretion.
- Psyllium, a soluble dietary fiber which will increase short-chain fatty acids which then help with increasing GLP-1.
- Curcumin, which enhances L-cell numbers, in turn promoting and increasing GLP-1 secretion. Also, curcumin may prolong gastric emptying, and increase insulin sensitivity.
- Ginseng, of which the bioactive compound stimulates secretion of GLP-1, and also has anti-diabetic effects.
Dr. Sung explains more about each of these in his video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to know more?
You might enjoy our previous main feature looking at some of the pros and cons:
Take care!
Share This Post
-
How can I stop overthinking everything? A clinical psychologist offers solutions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As a clinical psychologist, I often have clients say they are having trouble with thoughts “on a loop” in their head, which they find difficult to manage.
While rumination and overthinking are often considered the same thing, they are slightly different (though linked). Rumination is having thoughts on repeat in our minds. This can lead to overthinking – analysing those thoughts without finding solutions or solving the problem.
It’s like a vinyl record playing the same part of the song over and over. With a record, this is usually because of a scratch. Why we overthink is a little more complicated.
We’re on the lookout for threats
Our brains are hardwired to look for threats, to make a plan to address those threats and keep us safe. Those perceived threats may be based on past experiences, or may be the “what ifs” we imagine could happen in the future.
Our “what ifs” are usually negative outcomes. These are what we call “hot thoughts” – they bring up a lot of emotion (particularly sadness, worry or anger), which means we can easily get stuck on those thoughts and keep going over them.
However, because they are about things that have either already happened or might happen in the future (but are not happening now), we cannot fix the problem, so we keep going over the same thoughts.
Who overthinks?
Most people find themselves in situations at one time or another when they overthink.
Some people are more likely to ruminate. People who have had prior challenges or experienced trauma may have come to expect threats and look for them more than people who have not had adversities.
Deep thinkers, people who are prone to anxiety or low mood, and those who are sensitive or feel emotions deeply are also more likely to ruminate and overthink.
We all overthink from time to time, but some people are more prone to rumination.
BĀBI/UnsplashAlso, when we are stressed, our emotions tend to be stronger and last longer, and our thoughts can be less accurate, which means we can get stuck on thoughts more than we would usually.
Being run down or physically unwell can also mean our thoughts are harder to tackle and manage.
Acknowledge your feelings
When thoughts go on repeat, it is helpful to use both emotion-focused and problem-focused strategies.
Being emotion-focused means figuring out how we feel about something and addressing those feelings. For example, we might feel regret, anger or sadness about something that has happened, or worry about something that might happen.
Acknowledging those emotions, using self-care techniques and accessing social support to talk about and manage your feelings will be helpful.
The second part is being problem-focused. Looking at what you would do differently (if the thoughts are about something from your past) and making a plan for dealing with future possibilities your thoughts are raising.
But it is difficult to plan for all eventualities, so this strategy has limited usefulness.
What is more helpful is to make a plan for one or two of the more likely possibilities and accept there may be things that happen you haven’t thought of.
Think about why these thoughts are showing up
Our feelings and experiences are information; it is important to ask what this information is telling you and why these thoughts are showing up now.
For example, university has just started again. Parents of high school leavers might be lying awake at night (which is when rumination and overthinking is common) worrying about their young person.
Think of what the information is telling you.
TheVisualsYouNeed/ShutterstockKnowing how you would respond to some more likely possibilities (such as they will need money, they might be lonely or homesick) might be helpful.
But overthinking is also a sign of a new stage in both your lives, and needing to accept less control over your child’s choices and lives, while wanting the best for them. Recognising this means you can also talk about those feelings with others.
Let the thoughts go
A useful way to manage rumination or overthinking is “change, accept, and let go”.
Challenge and change aspects of your thoughts where you can. For example, the chance that your young person will run out of money and have no food and starve (overthinking tends to lead to your brain coming up with catastrophic outcomes!) is not likely.
You could plan to check in with your child regularly about how they are coping financially and encourage them to access budgeting support from university services.
Your thoughts are just ideas. They are not necessarily true or accurate, but when we overthink and have them on repeat, they can start to feel true because they become familiar. Coming up with a more realistic thought can help stop the loop of the unhelpful thought.
Accepting your emotions and finding ways to manage those (good self-care, social support, communication with those close to you) will also be helpful. As will accepting that life inevitably involves a lack of complete control over outcomes and possibilities life may throw at us. What we do have control over is our reactions and behaviours.
Remember, you have a 100% success rate of getting through challenges up until this point. You might have wanted to do things differently (and can plan to do that) but nevertheless, you coped and got through.
So, the last part is letting go of the need to know exactly how things will turn out, and believing in your ability (and sometimes others’) to cope.
What else can you do?
A stressed out and tired brain will be more likely to overthink, leading to more stress and creating a cycle that can affect your wellbeing.
So it’s important to manage your stress levels by eating and sleeping well, moving your body, doing things you enjoy, seeing people you care about, and doing things that fuel your soul and spirit.
Find ways to manage your stress levels.
antoniodiaz/ShutterstockDistraction – with pleasurable activities and people who bring you joy – can also get your thoughts off repeat.
If you do find overthinking is affecting your life, and your levels of anxiety are rising or your mood is dropping (your sleep, appetite and enjoyment of life and people is being negatively affected), it might be time to talk to someone and get some strategies to manage.
When things become too difficult to manage yourself (or with the help of those close to you), a therapist can provide tools that have been proven to be helpful. Some helpful tools to manage worry and your thoughts can also be found here.
When you find yourself overthinking, think about why you are having “hot thoughts”, acknowledge your feelings and do some future-focused problem solving. But also accept life can be unpredictable and focus on having faith in your ability to cope.
Kirsty Ross, Associate Professor and Senior Clinical Psychologist, Massey University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Accidental falls in the older adult population: What academic research shows
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Accidental falls are among the leading causes of injury and death among adults 65 years and older worldwide. As the aging population grows, researchers expect to see an increase in the number of fall injuries and related health spending.
Falls aren’t unique to older adults. Nealy 684,000 people die from falls each year globally. Another 37.3 million people each year require medical attention after a fall, according to the World Health Organization. But adults 65 and older account for the greatest number of falls.
In the United States, more than 1 in 4 older adults fall each year, according to the National Institute on Aging. One in 10 report a fall injury. And the risk of falling increases with age.
In 2022, health care spending for nonfatal falls among older adults was $80 billion, according to a 2024 study published in the journal Injury Prevention.
Meanwhile, the fall death rate in this population increased by 41% between 2012 and 2021, according to the latest CDC data.
“Unfortunately, fall-related deaths are increasing and we’re not sure why that is,” says Dr. Jennifer L. Vincenzo, an associate professor at the University of Arkansas for Medical Sciences in the department of physical therapy and the Center for Implementation Research. “So, we’re trying to work more on prevention.”
Vincenzo advises journalists to write about how accidental falls can be prevented. Remind your audiences that accidental falls are not an inevitable consequence of aging, and that while we do decline in many areas with age, there are things we can do to minimize the risk of falls, she says. And expand your coverage beyond the national Falls Prevention Awareness Week, which is always during the first week of fall — Sept. 23 to 27 this year.
Below, we explore falls among older people from different angles, including injury costs, prevention strategies and various disparities. We have paired each angle with data and research studies to inform your reporting.
Falls in older adults
In 2020, 14 million older adults in the U.S. reported falling during the previous year. In 2021, more than 38,700 older adults died due to unintentional falls, according to the CDC.
A fall could be immediately fatal for an older adult, but many times it’s the complications from a fall that lead to death.
The majority of hip fractures in older adults are caused by falls, Vincenzo says, and “it could be that people aren’t able to recover [from the injury], losing function, maybe getting pneumonia because they’re not moving around, or getting pressure injuries,” she says.
In addition, “sometimes people restrict their movement and activities after a fall, which they think is protective, but leads to further functional declines and increases in fall risk,” she adds.
Factors that can cause a fall include:
- Poor eyesight, reflexes and hearing. “If you cannot hear as well, anytime you’re doing something in your environment and there’s a noise, it will be really hard for you to focus on hearing what that noise is and what it means and also moving at the same time,” Vincenzo says.
- Loss of strength, balance, and mobility with age, which can lessen one’s ability to prevent a fall when slipping or tripping.
- Fear of falling, which usually indicates decreased balance.
- Conditions such as diabetes, heart disease, or problems with nerves or feet that can affect balance.
- Conditions like incontinence that cause rushed movement to the bathroom.
- Cognitive impairment or certain types of dementia.
- Unsafe footwear such as backless shoes or high heels.
- Medications or medication interactions that can cause dizziness or confusion.
- Safety hazards in the home or outdoors, such as poor lighting, steps and slippery surfaces.
Related Research
Nonfatal and Fatal Falls Among Adults Aged ≥65 Years — United States, 2020–2021
Ramakrishna Kakara, Gwen Bergen, Elizabeth Burns and Mark Stevens. Morbidity and Mortality Weekly Report, September 2023.Summary: Researchers analyzed data from the 2020 Behavioral Risk Factor Surveillance System — a landline and mobile phone survey conducted each year in all 50 U.S. states and the District of Columbia — and data from the 2021 National Vital Statistics System to identify patterns of injury and death due to falls in the U.S. by sex and state for adults 65 years and older. Among the findings:
- The percentage of women who reported falling was 28.9%, compared with 26.1% of men.
- Death rates from falls were higher among white and American Indian or Alaska Native older adults than among older adults from other racial and ethnic groups.
- In 2020, the percentage of older adults who reported falling during the past year ranged from 19.9% in Illinois to 38.0% in Alaska. The national estimate for 18 states was 27.6%.
- In 2021, the unintentional fall-related death rate among older adults ranged from 30.7 per 100,000 older adults in Alabama to 176.5 in Wisconsin. The national estimate for 26 states was 78.
“Although common, falls among older adults are preventable,” the authors write. “Health care providers can talk with patients about their fall risk and how falls can be prevented.”
Trends in Nonfatal Falls and Fall-Related Injuries Among Adults Aged ≥65 Years — United States, 2012-2018
Briana Moreland, Ramakrishna Kakara and Ankita Henry. Morbidity and Mortality Weekly Report, July 2020.Summary: Researchers compared data from the 2018 Behavioral Risk Factor Surveillance System. Among the findings:
- The percentage of older adults reporting a fall increased from 2012 to 2016, then slightly decreased from 2016 to 2018.
- Even with this decrease in 2018, older adults reported 35.6 million falls. Among those falls, 8.4 million resulted in an injury that limited regular activities for at least one day or resulted in a medical visit.
“Despite no significant changes in the rate of fall-related injuries from 2012 to 2018, the number of fall-related injuries and health care costs can be expected to increase as the proportion of older adults in the United States grows,” the authors write.
Understanding Modifiable and Unmodifiable Older Adult Fall Risk Factors to Create Effective Prevention Strategies
Gwen Bergen, et al. American Journal of Lifestyle Medicine, October 2019.Summary: Researchers used data from the 2016 U.S. Behavioral Risk Factor Surveillance System to better understand the association between falls and fall injuries in older adults and factors such as health, state and demographic characteristics. Among the findings:
- Depression had the strongest association with falls and fall injuries. About 40% of older adults who reported depression also reported at least one fall; 15% reported at least one fall injury.
- Falls and depression have several factors in common, including cognitive impairment, slow walking speed, poor balance, slow reaction time, weakness, low energy and low levels of activity.
- Other factors associated with an increased risk of falling include diabetes, vision problems and arthritis.
“The multiple characteristics associated with falls suggest that a comprehensive approach to reducing fall risk, which includes screening and assessing older adult patients to determine their unique, modifiable risk factors and then prescribing tailored care plans that include evidence-based interventions, is needed,” the authors write.
Health care use and cost
In addition to being the leading cause of injury, falls are the leading cause of hospitalization in older adults. Each year, about 3 million older adults visit the emergency department due to falls. More than 1 million get hospitalized.
In 2021, falls led to more than 38,000 deaths in adults 65 and older, according to the CDC.
The annual financial medical toll of falls among adults 65 years and older is expected to be more than $101 billion by 2030, according to the National Council on Aging, an organization advocating for older Americans.
Related research
Healthcare Spending for Non-Fatal Falls Among Older Adults, USA
Yara K. Haddad, et al. Injury Prevention, July 2024.Summary: In 2015, health care spending related to falls among older adults was roughly $50 billion. This study aims to update the estimate, using the 2017, 2019 and 2021 Medicare Current Beneficiary Survey, the most comprehensive and complete survey available on the Medicare population. Among the findings:
- In 2020, health care spending for non-fatal falls among older adults was $80 billion.
- Medicare paid $53.3 billion of the $80 billion, followed by $23.2 billion paid by private insurance or patients and $3.5 billion by Medicaid.
“The burden of falls on healthcare systems and healthcare spending will continue to rise if the risk of falls among the aging population is not properly addressed,” the authors write. “Many older adult falls can be prevented by addressing modifiable fall risk factors, including health and functional characteristics.”
Cost of Emergency Department and Inpatient Visits for Fall Injuries in Older Adults Lisa Reider, et al. Injury, February 2024.
Summary: The researchers analyzed data from the 2016-2018 National Inpatient Sample and National Emergency Department Sample, which are large, publicly available patient databases in the U.S. that include all insurance payers such as Medicare and private insurance. Among the findings:
- During 2016-2018, more than 920,000 older adults were admitted to the hospital and 2.3 million visited the emergency department due to falls. The combined annual cost was $19.2 billion.
- More than half of hospital admissions were due to bone fractures. About 14% of these admissions were due to multiple fractures and cost $2.5 billion.
“The $20 billion in annual acute treatment costs attributed to fall injury indicate an urgent need to implement evidence-based fall prevention interventions and underscores the importance of newly launched [emergency department]-based fall prevention efforts and investments in geriatric emergency departments,” the authors write.
Hip Fracture-Related Emergency Department Visits, Hospitalizations and Deaths by Mechanism of Injury Among Adults Aged 65 and Older, United States 2019
Briana L. Moreland, Jaswinder K. Legha, Karen E. Thomas and Elizabeth R. Burns. Journal of Aging and Health, June 2024.Summary: The researchers calculated hip fracture-related U.S. emergency department visits, hospitalizations and deaths among older adults, using data from the Healthcare Cost and Utilization Project and the National Vital Statistics System. Among the findings:
- In 2019, there were 318,797 emergency department visits, 290,130 hospitalizations and 7,731 deaths related to hip fractures among older adults.
- Nearly 88% of emergency department visits and hospitalizations and 83% of deaths related to hip fractures were caused by falls.
- These rates were highest among those living in rural areas and among adults 85 and older. More specifically, among adults 85 and older, the rate of hip fracture-related emergency department visits was nine times higher than among adults between 65 and 74 years old.
“Falls are common among older adults, but many are preventable,” the authors write. “Primary care providers can prevent falls among their older patients by screening for fall risk annually or after a fall, assessing modifiable risk factors such as strength and balance issues, and offering evidence-based interventions to reduce older adults’ risk of falls.”
Fall prevention
Several factors, including exercising, managing medication, checking vision and making homes safer can help prevent falls among older adults.
“Exercise is one of the best interventions we know of to prevent falls,” Vincenzo says. But “walking in and of itself will not help people to prevent falls and may even increase their risk of falling if they are at high risk of falls.”
The National Council on Aging also has a list of evidence-based fall prevention programs, including activities and exercises that are shown to be effective.
The National Institute on Aging has a room-by-room guide on preventing falls at home. Some examples include installing grab bars near toilets and on the inside and outside of the tub and shower, sitting down while preparing food to prevent fatigue, and keeping electrical cords near walls and away from walking paths.
There are also national and international initiatives to help prevent falls.
Stopping Elderly Accidents, Deaths and Injuries, or STEADI, is an initiative by the CDC’s Injury Center to help health care providers who treat older adults. It helps providers screen patients for fall risk, assess their fall risk factors and reduce their risk by using strategies that research has shown to be effective. STEADI’s guidelines are in line with the American and British Geriatric Societies’ Clinical Practice Guidelines for fall prevention.
“We’re making some iterations right now to STEADI that will come out in the next couple of years based on the World Falls Guidelines, as well as based on clinical providers’ feedback on how to make [STEADI] more feasible,” Vincenzo says.
The World Falls Guidelines is an international initiative to prevent falls in older adults. The guidelines are the result of the work of 14 international experts who came together in 2019 to consider whether new guidelines on fall prevention were needed. The task force then brought together 96 experts from 39 countries across five continents to create the guidelines.
The CDC’s STEADI initiative has a screening questionnaire for consumers to check their risk of falls, as does the National Council on Aging.
On the policy side, U.S. Rep. Carol Miller, R-W.V., and Melanie Stansbury, D-N.M., introduced the Stopping Addiction and Falls for the Elderly (SAFE) Act in March 2024. The bill would allow occupational and physical therapists to assess fall risks in older adults as part of the Medicare Annual Wellness Benefit. The bill was sent to the House Subcommittee on Health in the same month.
Meanwhile, older adults’ attitudes toward falls and fall prevention are also pivotal. For many, coming to terms with being at risk of falls and making changes such as using a cane, installing railings at home or changing medications isn’t easy for all older adults, studies show.
“Fall is a four-letter F-word in a way to older adults,” says Vincenzo, who started her career as a physical therapist. “It makes them feel ‘old.’ So, it’s a challenge on multiple fronts: U.S. health care infrastructure, clinical and community resources and facilitating health behavior change.”
Related research
Environmental Interventions for Preventing Falls in Older People Living in the Community
Lindy Clemson, et al. Cochrane Database of Systematic Reviews, March 2023.Summary: This review includes 22 studies from 10 countries involving a total of 8,463 older adults who live in the community, which includes their own home, a retirement facility or an assisted living facility, but not a hospital or nursing home. Among the findings:
- Removing fall hazards at home reduced the number of falls by 38% among older adults at a high risk of having a fall, including those who have had a fall in the past year, have been hospitalized or need support with daily activities. Examples of fall hazards at home include a stairway without railings, a slippery pathway or poor lighting.
- It’s unclear whether checking prescriptions for eyeglasses, wearing special footwear or installing bed alarm systems reduces the rate of falls.
- It’s also not clear whether educating older adults about fall risks reduces their fall risk.
The Influence of Older Adults’ Beliefs and Attitudes on Adopting Fall Prevention Behaviors
Judy A. Stevens, David A. Sleet and Laurence Z. Rubenstein. American Journal of Lifestyle Medicine. January 2017.Summary: Persuading older adults to adopt interventions that reduce their fall risk is challenging. Their attitudes and beliefs about falls play a large role in how well they accept and adopt fall prevention strategies, the authors write. Among the common attitudes and beliefs:
- Many older adults believe that falls “just happen,” are a normal result of aging or are simply due to bad luck.
- Many don’t acknowledge or recognize their fall risk.
- For many, falls are considered to be relevant only for frail or very old people.
- Many believe that their home environment or daily activities can be a risk for fall, but do not consider biological factors such as dizziness or muscle weakness.
- For many, fall prevention simply consists of “being careful” or holding on to things when moving about the house.
“To reduce falls, health care practitioners have to help patients understand and acknowledge their fall risk while emphasizing the positive benefits of fall prevention,” the authors write. “They should offer patients individualized fall prevention interventions as well as provide ongoing support to help patients adopt and maintain fall prevention strategies and behaviors to reduce their fall risk. Implementing prevention programs such as CDC’s STEADI can help providers discuss the importance of falls and fall prevention with their older patients.”
Reframing Fall Prevention and Risk Management as a Chronic Condition Through the Lens of the Expanded Chronic Care Model: Will Integrating Clinical Care and Public Health Improve Outcomes?
Jennifer L. Vincenzo, Gwen Bergen, Colleen M. Casey and Elizabeth Eckstrom. The Gerontologist, June 2024.Summary: The authors recommend approaching fall prevention from the lens of chronic disease management programs because falls and fall risk are chronic issues for many older adults.
“Policymakers, health systems, and community partners can consider aligning fall risk management with the [Expanded Chronic Care Model], as has been done for diabetes,” the authors write. “This can help translate high-quality research on the effectiveness of fall prevention interventions into daily practice for older adults to alter the trajectory of older adult falls and fall-related injuries.”
Disparities
Older adults face several barriers to reducing their fall risk. Accessing health care services and paying for services such as physical therapy is not feasible for everyone. Some may lack transportation resources to go to and from medical appointments. Social isolation can increase the risk of death from falls. In addition, physicians may not have the time to fit in a fall risk screening while treating older patients for other health concerns.
Moreover, implementing fall risk screening, assessment and intervention in the current U.S. health care structure remains a challenge, Vincenzo says.
Related research
Mortality Due to Falls by County, Age Group, Race, and Ethnicity in the USA, 2000-19: A Systematic Analysis of Health Disparities
Parkes Kendrick, et al. The Lancet Public Health, August 2024.Summary: Researchers analyzed death registration data from the U.S. National Vital Statistics System and population data from the U.S. National Center for Health Statistics to estimate annual fall-related mortality. The data spanned from 2000 to 2019 and includes all age groups. Among the findings:
- The disparities between racial and ethnic populations varied widely by age group. Deaths from falls among younger adults were highest for the American Indian/Alaska Native population, while among older adults it was highest for the white population.
- For older adults, deaths from falls were particularly high in the white population within clusters of counties across states including Florida, Minnesota and Wisconsin.
- One factor that could contribute to higher death rates among white older adults is social isolation, the authors write. “Studies suggest that older Black and Latino adults are more likely to have close social support compared with older white adults, while AIAN and Asian individuals might be more likely to live in multigenerational households,” they write.
“Among older adults, current prevention techniques might need to be restructured to reduce frailty by implementing early prevention and emphasizing particularly successful interventions. Improving social isolation and evaluating the effectiveness of prevention programs among minoritized populations are also key,” the authors write.
Demographic Comparisons of Self-Reported Fall Risk Factors Among Older Adults Attending Outpatient Rehabilitation
Mariana Wingood, et al. Clinical Interventions in Aging, February 2024.Summary: Researchers analyzed the electronic health record data of 108,751 older adults attending outpatient rehabilitation within a large U.S. health care system across seven states, between 2018 and 2022. Among the findings:
- More than 44% of the older adults were at risk of falls; nearly 35% had a history of falls.
- The most common risk factors for falls were diminished strength, gait and balance.
- Compared to white older adults, Native American/Alaska Natives had the highest prevalence of fall history (43.8%) and Hispanics had the highest prevalence of falls with injury (56.1%).
“Findings indicate that rehabilitation providers should perform screenings for these impairments, including incontinence and medication among females, loss of feeling in the feet among males, and all Stay Independent Questionnaire-related fall risk factors among Native American/Alaska Natives, Hispanics, and Blacks,” the authors write.
Resources and articles
- National Institute on Aging
- National Council on Aging
- Gerontological Society of America
- Home Health Agencies Failed To Report Over Half of Falls With Major Injury and Hospitalization Among Their Medicare Patients, a 2023 report from the U.S Department of Health and Human Services’ Office of Inspector General.
- 6 tips for improving new coverage of older people, a tip sheet from The Journalist’s Resource.
- Crosswalk and pedestrian safety: What you need to know from recent research, from The Journalist’s Resource.
- Aging-in-place technology challenges and trends, a resource from the Association of Health Care Journalists.
- Successful aging at home: what reporters should know, a resource from the Association of Health Care Journalists.
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Saunas: Health Benefits (& Caveats)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Heat Is On
In Tuesday’s newsletter, we asked you your (health-related) opinion on saunas, and got the above-depicted, below-described, set of responses:
- About 53% said it is “a healthful activity with many benefits”
- About 25% said it is “best avoided; I feel like I’m dying in there”
- About 12% said “it feels good and therefore can’t be all bad”
So what does the science say?
The heat of saunas carries a health risk: True or False?
False, generally speaking, for any practical purposes. Of course, anything in life comes with a health risk, but statistically speaking, your shower at home is a lot more dangerous than a sauna (risk of slipping with no help at hand).
It took a bit of effort to find a paper on the health risks of saunas, because all the papers on PubMed etc coming up for those keywords were initially papers with “reduces the risk of…”, i.e. ways in which the sauna is healthy.
However, we did find one:
❝Contraindications to sauna bathing include unstable angina pectoris, recent myocardial infarction, and severe aortic stenosis.
Sauna bathing is safe, however, for most people with coronary heart disease with stable angina pectoris or old myocardial infarction.
Very few acute myocardial infarctions and sudden deaths occur in saunas, but alcohol consumption during sauna bathing increases the risk of hypotension, arrhythmia, and sudden death, and should be avoided. ❞
~ Dr. Matti Hannuksela & Dr. Samer Ellahham
Source: Benefits and risks of sauna bathing
So, very safe for most people, safe even for most people with heart disease, but there are exceptions so check with your own doctor of course.
And drinking alcohol anywhere is bad for the health, but in a sauna it’s a truly terrible idea. As an aside, please don’t drink alcohol in the shower, either (risk of slipping with no help at hand, and this time, broken glass too).
On the topic of it being safe for most people’s hearts, see also:
Beneficial effects of sauna bathing for heart failure patients
As an additional note, those who have a particular sensitivity to the heat, may (again please check with your own doctor, as your case may vary) actually benefit from moderate sauna use, to reduce the cardiovascular strain that your body experiences during heatwaves (remember, you can get out of a sauna more easily than you can get out of a heatwave, so for many people it’s a lot easier to do moderation and improve thermoregulatory responses):
Sauna usage can bring many health benefits: True or False?
True! Again, at least for most people. As well as the above-discussed items, here’s one for mortality rates in healthy Finnish men:
Not only that, also…
❝The Finnish saunas have the most consistent and robust evidence regarding health benefits and they have been shown to decrease the risk of health outcomes such as hypertension, cardiovascular disease, thromboembolism, dementia, and respiratory conditions; may improve the severity of musculoskeletal disorders, COVID-19, headache and flu, while also improving mental well-being, sleep, and longevity.
Finnish saunas may also augment the beneficial effects of other protective lifestyle factors such as physical activity.
The beneficial effects of passive heat therapies may be linked to their anti-inflammatory, cytoprotective and anti-oxidant properties and synergistic effects on neuroendocrine, circulatory, cardiovascular and immune function.
Passive heat therapies, notably Finnish saunas, are emerging as potentially powerful and holistic strategies to promoting health and extending the healthspan in all populations. ❞
~ Dr. Jari Laukkanen & Dr. Setor Kunutsor
(the repeated clarification of “Finnish sauna” is not a matter of fervent nationalism, by the way, but rather a matter of disambiguating it from Swedish sauna, which has some differences, most notably a lack of steam)
That reminds us: in Scandinavia, it is usual to use a sauna naked, and in Finland in particular, it is a common social activity amongst friends, coworkers, etc. In the US, many people are not so comfortable with nudity, and indeed, many places that provide saunas, may require the wearing of swimwear. But…
Just one problem: if you’re wearing swimwear because you’ve just been swimming in a pool, you now have chlorinated water soaked into your swimwear, which in the sauna, will become steam + chlorine gas. That’s not so good for your health (and is one reason, beyond tradition and simple normalization, for why swimwear is usually not permitted in Finnish saunas).
Want to read more?
You might like our previous main feature,
Turning Up The Heat Against Diabetes & Alzheimer’s ← you guessed it, sauna may be beneficial against these too
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Metformin For Weight-Loss & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Metformin Without Diabetes?
Metformin is a diabetes drug; it works by:
- decreasing glucose absorption from the gut
- decreasing glucose production in the liver
- increasing glucose sensitivity
It doesn’t change how much insulin is secreted, and is unlikely to cause hypoglycemia, making it relatively safe as diabetes drugs go.
It’s a biguanide drug, and/but so far as science knows (so far), its mechanism of action is unique (i.e. no other drug works the same way that metformin does).
Today we’ll examine its off-label uses and see what the science says!
A note on terms: “off-label” = when a drug is prescribed to treat something other than the main purpose(s) for which the drug was approved.
Other examples include modafinil against depression, and beta-blockers against anxiety.
Why take it if not diabetic?
There are many reasons people take it, including just general health and life extension:
However, its use was originally expanded (still “off-label”, but widely prescribed) past “just for diabetes” when it showed efficacy in treating pre-diabetes. Here for example is a longitudinal study that found metformin use performed similarly to lifestyle interventions (e.g. diet, exercise, etc). In their words:
❝ Lifestyle intervention or metformin significantly reduced diabetes development over 15 years. There were no overall differences in the aggregate microvascular outcome between treatment groups❞
But, it seems it does more, as this more recent review found:
❝Long-term weight loss was also seen in both [metformin and intensive lifestyle intervention] groups, with better maintenance under metformin.
Subgroup analyses from the DPP/DPPOS have shed important light on the actions of metformin, including a greater effect in women with prior gestational diabetes, and a reduction in coronary artery calcium in men that might suggest a cardioprotective effect.
Long-term diabetes prevention with metformin is feasible and is supported in influential guidelines for selected groups of subjects.❞
Source: Metformin for diabetes prevention: update of the evidence base
We were wondering about that cardioprotective effect, so…
Cardioprotective effect
In short, another review (published a few months after the above one) confirmed the previous findings, and also added:
❝Patients with BMI > 35 showed an association between metformin use and lower incidence of CVD, including African Americans older than age 65. The data suggest that morbidly obese patients with prediabetes may benefit from the use of metformin as recommended by the ADA.❞
We wondered about the weight loss implications of this, and…
For weight loss
The short version is, it works:
- Effectiveness of metformin on weight loss in non-diabetic individuals with obesity
- Metformin for weight reduction in non-diabetic patients: a systematic review and meta-analysis
- Metformin induces weight loss associated with gut microbiota alteration in non-diabetic obese women
…and many many more where those came from. As a point of interest, it has also been compared and contrasted to GLP-1 agonists.
Compared/contrasted with GLP-1 agonists
It’s not quite as effective for weight loss, and/but it’s a lot cheaper, is tablets rather than injections, has fewer side effects (for most people), and doesn’t result in dramatic yoyo-ing if there’s an interruption to taking it:
Or if you prefer a reader-friendly pop-science version:
Ozempic vs Metformin: Comparing The Two Diabetes Medications
Is it safe?
For most people yes, but there are a stack of contraindications, so it’s best to speak with your doctor. However, particular things to be aware of include:
- Usually contraindicated if you have kidney problems of any kind
- Usually contraindicated if you have liver problems of any kind
- May be contraindicated if you have issues with B12 levels
See also: Metformin: Is it a drug for all reasons and diseases?
Where can I get it?
As it’s a prescription-controlled drug, we can’t give you a handy Amazon link for this one.
However, many physicians are willing to prescribe it for off-label use (i.e., for reasons other than diabetes), so speak with yours (telehealth options may also be available).
If you do plan to speak with your doctor and you’re not sure they’ll be agreeable, you might want to get this paper and print it to take it with you:
Off-label indications of Metformin – Review of Literature
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Better Sex = Longer Life (Here’s How)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
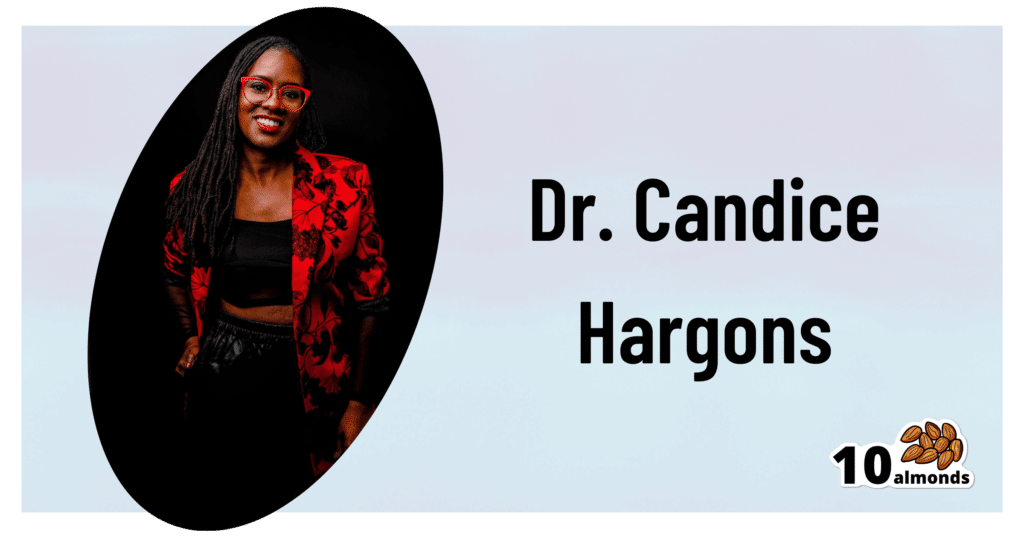
This is Dr. Candice Hargons. She’s a professor of psychology, and has served on the Kentucky Psychological Association Board, the Society of Counseling Psychology Executive Board, and the American Psychological Association (APA)’s Council of Representatives. She also served on the APA Board of Directors, after receiving the APA’s Presidential Citation award for her research and leadership.
She leads the Study of Mental And Sexual Health Equity in Relationships (SMASHER Lab), with a predominant focus on promoting good sex, sexual wellness, and liberation among couples and communities.
In her own words:
❝Sex is one of the most common and normal human behaviors, and yet it remains relatively taboo as a topic. Many people worry about being judged, either for being perceived as too sexual or not sexual enough, and a major focus of my work is to normalize talking and learning about sex to improve sexual functioning across the adult lifespan.❞
~ Dr. Candice Hargons
So, let’s do that!
What does good sex do for health?
We’ve written previously about the health aspects of orgasms specifically:
“Early To Bed…” (Mythbusting Orgasms) ← including resources pertaining to anorgasmia, the inability to orgasm
…but orgasms are not the be-all-and-end-all of sex; see for example:
A Urologist Explains Edging: What, Why, & Is It Safe? ← when the journey is genuinely more of a focus than the destination
And certainly, good sex is simply a very good way to relax and de-stress, which is important, given how important stress management is to general health in very many ways (affecting things ranging from inflammation to heart health and more).
Plus, while the level of athleticism deployed may vary, sex is a physical activity, and physical activity is, as a rule, good.
There’s more to it than that though! It also can help us bind closely to our loved ones, in a positive way, which—critically—has a very positive impact on healthy longevity:
Only One Kind Of Relationship Promotes Longevity This Much! ← this is about the seriousness of the relationship, not the sex, but for most people, a strong and fulfilling relationship will include having good sex.
The scientific relationship between sex and longevity also got a whole chapter in this excellent book that we reviewed all so recently:
Age Proof: The New Science of Living a Longer and Healthier Life – by Dr. Rose Anne Kenny
What makes it “good”?
Dr. Hargons considers (and her opinion is backed by extensive research in the SMASHER Lab, if you’ll pardon the mental image that that might conjure) that first and foremost… It has to feel good to all parties involved.
In contrast, oftentimes, one partner’s pleasure is prioritized over another’s, and that becomes a problem.*
*assuming that’s not part of an established kink dynamic with enthusiastic affirmative consent, such as if the partner whose pleasure is being deprioritized is enthusiastically requesting to be denied orgasms, for example. Yes, that’s a real kink and even a popular one, but it’s not what’s happening in most sexually uneven relationships.
This kind of unplanned disparity often goes undiscussed by the couple in question—especially in heterosexual couples if the man is getting what he wants/needs and the woman isn’t, because there’s a rather lop-sided societal expectation in that regard. And even a loving, well-intentioned man can simply not know how to do better and be afraid to ask. And for that matter, it’s also entirely possible for his partner to not know either.
Dr. Hargons lists the four main keys as:
- Communication
- Intimacy
- Passion
- Pleasure
And communication indeed comes first, so to speak. For example, she advises:
❝Begin by identifying what you like and don’t like sexually. An easy way to do this is to create a “Yes, No, Maybe So” list. You can use paper or a Notes app on your phone.
Create three columns: one for Yes, No, and Maybe So sections. In the Yes section, write all the things you enjoy and want to keep doing sexually, as well as things you have not tried yet that you want to try. In the No section, write all the things you don’t enjoy and do not want to do anymore. It can also include things you haven’t tried that you’re uninterested in trying. Finally, in your Maybe So list, write all the things you’re curious about and/or are only willing to try in specific settings or circumstances.
You can share this list with your partner, but even if you are not ready to do that, you will already have enhanced your sexual self-awareness and be better positioned to talk with your sexual partner about what you want.❞
This represents an important shift from “whatever” to taking an active role in your sex life at your own pace.
And from there, it’s just a matter of exploring, together, and learning as you go. Could anything be more exciting than that?
“What if I’m single?”
We talked about this a little previously, more relationally than sexually specifically, though:
Now, a single person can of course still have an active sex life if you so choose, in which case, the above advice still applies, just, it’ll be conversations with your partner-of-the-moment rather than with a life partner. And that’s important too! Just because something is casual, doesn’t mean it need not be entered into mindfully and with a sense of what you want out of it, and communicating that effectively (while encouraging the same from others, and of course actually listening to, and caring about, what they say too).
And if you are, perchance, single and decided on a life of celibacy now, you can and (if you are sexual at all) should still figure out what you like and don’t like sexually, because even if it’s going to be you-on-you action, it will be good for you to love yourself enough to do it right.
Seriously, treat yourself at least as well as you would any other lover.
On which note, corded wand-style vibrators like the famous “Magic Wand” kind are much more powerful than the battery kind, and you will feel the difference, in a good way.
And if you really want to invest in your sexual wellness and you like the idea, saddle-style vibrators like this one will rock your socks off in ways handheld vibrators couldn’t dream of.
Want to know more?
You might want to check out Dr. Hargons’ book:
Good Sex: Stories, Science, and Strategies for Sexual Liberation – by Dr. Candice Hargons ← this covers so many important areas, more than we have room to here. Just check out the table of contents, and you’ll see what we mean.
…which we haven’t reviewed yet, but here are some excellent related books that we have:
- Come Together: The Science (and Art) of Creating Lasting Sexual Connections – by Dr. Emily Nagoski
- Better Sex Through Mindfulness: How Women Can Cultivate Desire – by Dr. Lori Brotto
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: