Gut Health 2.0
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Gene Expression & Gut Health

This is Dr. Tim Spector. After training in medicine and becoming a consultant rheumatologist, he’s turned his attention to medical research, and is these days a specialist in twin studies, genetics, epigenetics, microbiome, and diet.
What does he want us to know?
For one thing: epigenetics are for more than just getting your grandparents’ trauma.
More usefully: there are things we can do to improve epigenetic factors in our body
DNA is often seen as the script by which our body does whatever it’s going to do, but it’s only part of the story. Thinking of DNA as some kind of “magical immutable law of reality” overlooks (to labor the metaphor) script revisions, notes made in the margins, directorial choices, and ad-lib improvizations, as well as the quality of the audience’s hearing and comprehension.
Hence the premise of one of Dr. Spector’s older books, “Identically Different: Why We Can Change Our Genes”
(*in fact, it was his first, from all the way back in 2013, when he’d only been a doctor for 34 years)
Gene expression will trump genes every time, and gene expression is something that can often be changed without getting in there with CRISPR / a big pair of scissors and some craft glue.
How this happens on the micro level is beyond the scope of today’s article; part of it has to do with enzymes that get involved in the DNA transcription process, and those enzymes in turn are despatched or not depending on hormonal messaging—in the broadest sense of “hormonal”; all the body’s hormonal chemical messengers, not just the ones people think of as hormones.
However, hormonal messaging (of many kinds) is strongly influenced by something we can control relatively easily with a little good (science-based) knowledge: the gut.
The gut, the SAD, and the easy
In broad strokes: we know what is good for the gut. We’ve written about it before at 10almonds:
Making Friends With Your Gut (You Can Thank Us Later)
This is very much in contrast with what in scientific literature is often abbreviated “SAD”, the Standard American Diet, which is very bad for the gut.
However, Dr. Spector (while fully encouraging everyone to enjoy an evidence-based gut-healthy diet) wanted to do one better than just a sweeping one-size-fits-all advice, so he set up a big study with 15,000 identical twins; you can read about it here: TwinsUK
The information that came out of that was about a lot more than just gene expression and gut health, but it did provide the foundation for Dr. Spector’s next project, ZOE.
ZOE crowdsources huge amounts of data including individual metabolic responses to standardized meals in order to predict personalized food responses based on individual biology and unique microbiome profile.
In other words, it takes the guesswork out of a) knowing what your genes mean for your food responses b) tailoring your food choices with your genetic expression in mind, and c) ultimately creating a positive feedback loop to much better health on all levels.
Now, this is not an ad for ZOE, but if you so wish, you can…
- Get the free ZOE gut health guide (this is good, but generic, gut health information)
- Take the ZOE home gut health test (quiz followed by offers of lab tests)
- Browse the ZOE Health Academy, its education wing
Want to know more?
Dr. Spector has a bunch of books out, including some that we’ve reviewed previously:
- Spoon-Fed: Why Almost Everything We’ve Been Told About Food Is Wrong
- The Diet Myth: The Real Science Behind What We Eat
- Food for Life: The New Science of Eating Well
You can also check out our own previous main feature, which wasn’t about Dr. Spector’s work but was very adjacent:
The Brain-Gut Highway: A Two-Way Street
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Are You Flourishing? (There’s a Scale)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What does it mean, to flourish? And how can you do it more?
In 2009, psychologists Diener et al developed the “Flourishing Scale”, or as it was more prosaically called originally, “Subjective Wellness Scale”. The name was changed later, as it was noted that it went beyond what was typically considered mere “wellness”.
This scale was so useful, that colleagues scrambled to see if they could improve on it, such as with PERMA (2012), which looked at:
- Positive emotion
- Engagement
- positive Relationships
- Meaning
- Accomplishment/Achievement
While popular (despite the tenuous acronym, it is a very good list of things to foster in your life), this was studied and measured scientifically and found to not be an improvement on the Flourishing Scale / SWS, so we’re going to stick to the original version for now.
We couldn’t find an interactive online quiz for the scale though (apart from this NY Times one, which is paywalled for NYT subscribers, so enjoy if you’re a NYT subscriber!), so here’s the source material, still hosted on the website of the (now deceased, as of a couple of years ago) author:
Flourishing Scale (FS) ← it’s an eight-question, ranked choice scale
How did you score? And…
What are the keys to flourishing more?
According to Jeffrey Davis M.A., of Tracking Wonder, there are five key attributes that we must develop and/or maintain:
The ability to direct and re-direct your attention
This isn’t just a task-related thing.This is about your mind itself. For example, the ability to recognize what your emotions are telling you, thank them for the message, and then set them aside. Or the ability to cut through negative thought spirals! How often have you worried about future events that didn’t transpire, or twisted yourself in knots over a past event that you can’t change?
Action: check out our previous article “The Off-Button For Your Brain” ← this is a technique for switching off racing thoughts, and it’s really good
Want more? We also did this:
The tendency to shape your time with intention and for impact
Time is an incredibly precious asset. How you use it is a very personal choice. You don’t have to maximize productivity (though you can if you want), but for example there’s a difference between:
- Deciding to spend an hour watching a TV show you really enjoy
- Wondering what’s on TV, browsing aimlessly, watching listlessly, just a distraction
In the former case, you are enjoying your time. Literally: you are experiencing joy during your time.
In the latter case, to borrow from Jim Steinman, “you were only killing time and it’ll kill you right back”!
Action: do a time audit for a week, and see where your time really goes, rather than where you expect or hope for it to go. Use this information to plan your next week more intentionally. Repeat as and when it seems like it might be useful!
The practice of constant improvement
Fun fact: you are good enough already. And you can also improve. You don’t have to, but improving in the areas that are meaningful to you can really add up over time. This could be becoming excellent at something for which already have a passion… It could also be brushing up something that you feel might be holding you back.
Action: do a quick SWOT* self-assessment. Then plan your next step from there!
*Strengths, Weaknesses, Opportunities, Threats. What are yours?
The ability to communicate and listen to others
A lot of this is about feedback. Giving and receiving feedback are often amongst the hardest things we do in the category of communication… Especially if the feedback is negative. How to decide what to disregard as baseless criticism, and what to take on board (and try not to take it personally), or the other way around, how to present negative feedback in a way that won’t trigger defensiveness.
Action: check out our previous article “Save Time With Better Communication” for some tips that really make relationships (of any kind) so much easier.
The commitment to positive experiences
Many things in life are not fun. Often, we know in advance that they will not be fun. The key here is the ability to make the most of a bad situation, and seek out better situations by your actions. Not like a lost person in a desert seeks water, but like a chess player who employs a general strategy to make tactical advantages more likely to appear.
Action: think about something you have to do but don’t want to. How could it be made more fun? Or failing that, how could it be made at least more comfortable?
See also: Working Smarter < Working Brighter!
Want to read more?
Check out: What Is Flourishing in Positive Psychology? (+8 Tips & PDF)
Share This Post
-
Are GMOs Good Or Bad For Us?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Unzipping Our Food’s Genes
In yesterday’s newsletter, we asked you for your (health-related) views on GMOs.
But what does the science say?
First, a note on terms
Technically, we (humans) have been (g)enetically (m)odifying (o)rganisms for thousands of years.
If you eat a banana, you are enjoying the product of many generations of artificial selection, to change its genes to produce a fruit that is soft, sweet, high in nutrients, and digestible without cooking. The original banana plant would be barely recognizable to many people now (and also, barely edible). We’ve done similarly with countless other food products.
So in this article, we’re going to be talking exclusively about modern genetic modification of organisms, using exciting new (ish, new as in “in the last century”) techniques to modify the genes directly, in a copy-paste fashion.
For more details on the different kinds of genetic modification of organisms, and how they’re each done (including the modern kinds), check out this great article from Sciencing, who explain it in more words than we have room for here:
Sciencing | How Are GMOs Made?
(the above also offers tl;dr section summaries, which are great too)
GMOS are outright dangerous (cancer risks, unknown risks, etc): True or False?
False, so far as we know, in any direct* fashion. Obviously “unknown risks” is quite a factor, since those are, well, unknown. But GMOs on the market undergo a lot of safety testing, and have invariably passed happily.
*However! Glyphosate (the herbicide), on the other hand, has a terrible safety profile and is internationally banned in very many countries for this reason.
Why is this important? Because…
- in the US (and two out of ten Canadian provinces), glyphosate is not banned
- In the US (and we may hypothesize, those two Canadian provinces) one of the major uses of genetic modification of foodstuffs is to make it resistant to glyphosate
- Consequently, GMO foodstuffs grown in those places have generally been liberally doused in glyphosate
So… It’s not that the genetic modification itself makes the food dangerous and potentially carcinogenic (it doesn’t), but it is that the genetic modification makes it possible to use a lot more glyphosate without losing crops to glyphosate’s highly destructive properties.
Which results in the end-consumer eating glyphosate. Which is not good. For example:
❝Following the landmark case against Monsanto, which saw them being found liable for a former groundskeeper, 46 year old Dewayne Johnson’s cancer, 32 countries have to date banned the use of Glyphosate, the key ingredient in Monsanto’s Roundup weed killer. The court awarded Johnson R4.2 billion in damages finding Monsanto “acted with malice or oppression”.❞
Source: see below!
You can read more about where glyphosate is and isn’t banned, here:
33 countries ban the use of Glyphosate—the key ingredient in Roundup
For the science of this (and especially the GMO → glyphosate use → cancer pipeline), see:
Use of Genetically Modified Organism (GMO)-Containing Food Products in Children
GMOs are extra healthy because of the modifications (they were designed for that, right?): True or False?
True or False depending on who made them and why! As we’ve seen above, not all companies seem to have the best interests of consumer health in mind.
However, they can be! Here are a couple of great examples:
❝Recently, two genome-edited crops targeted for nutritional improvement, high GABA tomatoes and high oleic acid soybeans, have been released to the market.
Nutritional improvement in cultivated crops has been a major target of conventional genetic modification technologies as well as classical breeding methods❞
Source: Drs. Nagamine & Ezura
Read in full: Genome Editing for Improving Crop Nutrition
(note, they draw a distinction of meaning between genome editing and genetic modification, according to which of two techniques is used, but for the purposes of our article today, this is under the same umbrella)
Want to know more?
If you’d like to read more about this than we have room for here, here’s a great review in the Journal of Food Science & Nutrition:
Should we still worry about the safety of GMO foods? Why and why not? A review
Take care!
Share This Post
-
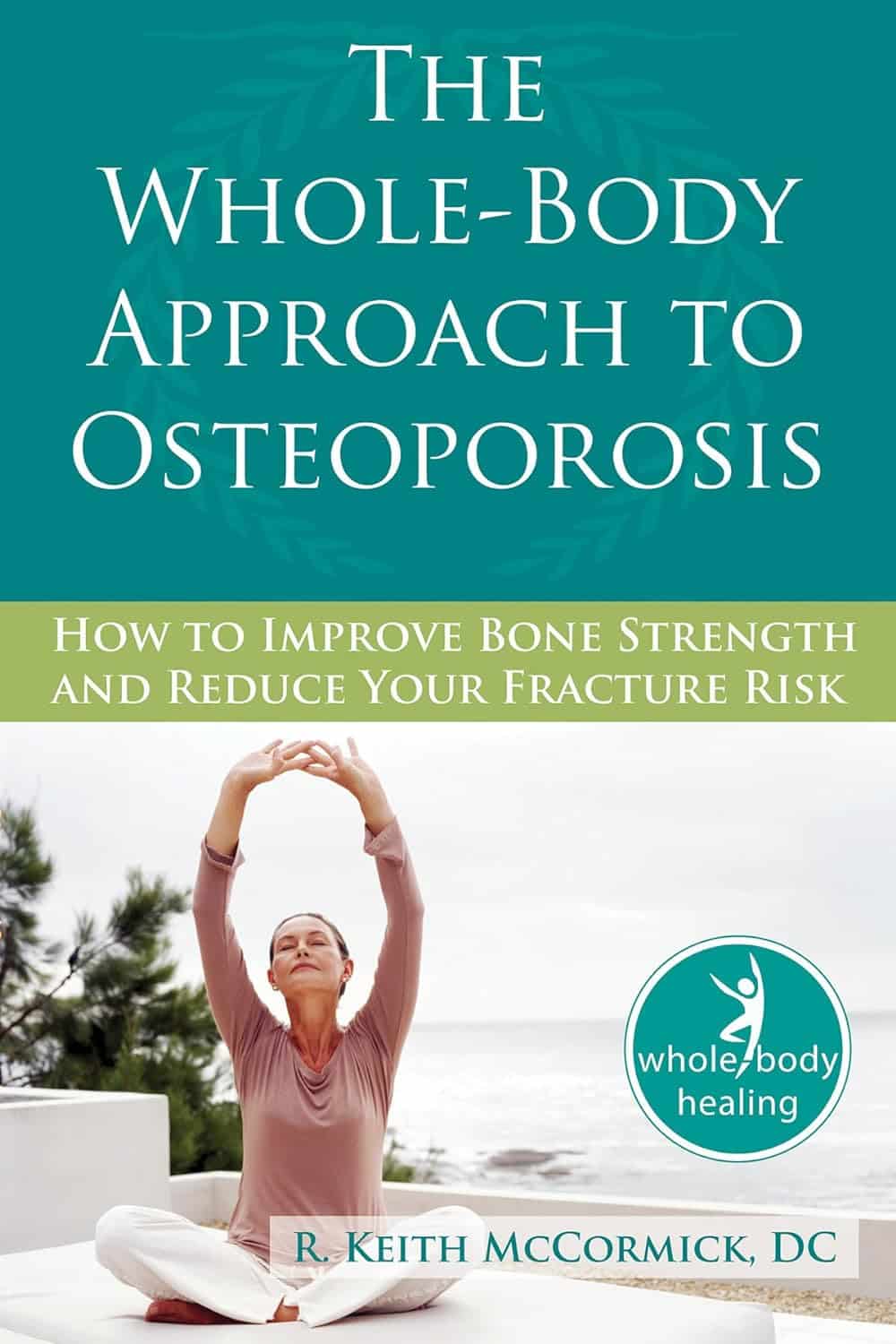
The Whole-Body Approach to Osteoporosis – by Keith McCormick
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You probably already know to get enough calcium and vitamin D, and do some resistance training. What does this book offer beyond that advice?
It’s pretty comprehensive, as it turns out. It covers the above, plus the wide range of medications available, what supplements help or harm or just don’t have enough evidence either way yet, things like that.
Amongst the most important offerings are the signs and symptoms that can help monitor your bone health (things you can do at home! Like examinations of your fingernails, hair, skin, tongue, and so forth, that will reveal information about your internal biochemical make-up), as well as what lab tests to ask for. Which is important, as osteoporosis is one of those things whereby we often don’t learn something is wrong until it’s too late.
The author is a chiropractor, which doesn’t always have a reputation as the most robustly science-based of physical therapy options, but he…
- doesn’t talk about chiropractic
- did confer with a flock of experts (osteopaths, nutritionists, etc) to inform/check his work
- does refer consistently to good science, and explains it well
- includes 16 pages of academic references, and yes, they are very reputable publications
Bottom line: this one really does give what the subtitle promises: a whole body approach to avoiding (or reversing) osteoporosis.
Click here to check out The Whole Body Approach To Osteoporosis; sooner is better than later!
Share This Post
Related Posts
-
Cavolo Nero & Sweet Potato Hash
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
🎶 Sweet potato hash? It’s a seasonal smash… Catches on in a flash… Let’s do the hash 🎶
You will need
- 6 oz cavolo nero, tough stems removed, chopped
- 1 large sweet potato, diced
- 1 large red onion, finely chopped
- 1 parsnip, grated
- 1 small red pepper, chopped
- 4 oz baby portobello mushrooms, chopped
- ½ cup fresh or thawed peas
- ¼ bulb garlic, thinly sliced
- 1 tbsp nutritional yeast
- 2 tsp black pepper, coarse ground
- 1 tsp dried rosemary
- 1 tsp dried thyme (dried for convenience; fresh is also fine if you have it)
- 1 tsp red chili flakes (dried for convenience; fresh is also fine if you have it)
- 1 tsp ground turmeric
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 425℉ / 220℃.
2) Toss the diced sweet potato in 1 tbsp olive oil, as well as the nutritional yeast, ground turmeric, black pepper, and MSG/salt, ensuring an even distribution. Roast in the oven on a lined baking tray, for 30 minutes, turning at least once to get all sides of the potato. When it is done, remove from the oven and set aside.
3) Heat a little oil in a sauté pan or large skillet (either is fine; we’re not adding liquids today), and fry the onion, parsnip, and pepper until softened, which should take about 5 minutes (this is one reason why we grated the parsnip; the other is for the variation in texture).
4) Add the garlic, mushrooms, herbs, and chili flakes, and cook for a further 1 minute, while stirring.
5) Add the cavolo nero and peas, stir until the cavolo nero begins to wilt, and then…
6) Add the roasted sweet potato; cook for about 5 more minutes, pressing down with the spatula here and there to mash the ingredients together.
7) Turn the hash over when it begins to brown on the bottom, to lightly brown the other side too.
8) Serve hot.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Brain Food? The Eyes Have It!
- Which Bell Peppers To Pick?
- Ergothioneine: “The Longevity Vitamin” (That’s Not A Vitamin)
- Our Top 5 Spices: How Much Is Enough For Benefits?
- What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Seven Principles for Making Marriage Work – by Dr. John Gottman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of relationship advice can seem a little wishy-washy. Hardline clinical work, on the other hand, can seem removed from the complex reality of married life. Dr. Gottman, meanwhile, strikes a perfect balance.
He looks at huge datasets, and he listens to very many couples. He famously isolated four relational factors that predict divorce with 91% accuracy, his “Four Horsemen”:
- Criticism
- Contempt
- Defensiveness
- Stonewalling
He also, as the title of this book promises (and we get a chapter-by-chapter deep-dive on each of them) looks at “Seven principles for making marriage work”. They’re not one-word items, so including them here would take up the rest of our space, and this is a book review not a book summary. However…
Dr. Gottman’s seven principles are, much like his more famous “four horsemen”, deeply rooted in science, while also firmly grounded in the reality of individual couples. Essentially, by listening to very many couples talk about their relationships, and seeing how things panned out with each of them in the long-term, he was able to see what things kept on coming up each time in the couples that worked out. What did they do differently?
And, that’s the real meat of the book. Science yes, but lots of real-world case studies and examples, from couples that worked and couples that didn’t.
In so doing, he provides a roadmap for couples who are serious about making their marriage the best it can be.
Bottom line: this is a must-have book for couples in general, no matter how good or bad the relationship.
- For some it’ll be a matter of realising “You know what; this isn’t going to work”
- For others, it’ll be a matter of “Ah, relief, this is how we can resolve that!”
- For still yet others, it’ll be a matter of “We’re doing these things right; let’s keep them forefront in our minds and never get complacent!”
- And for everyone who is in a relationship or thinking of getting into one, it’s a top-tier manual.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Reishi Mushrooms: Which Benefits Do They Really Have?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Reishi Mushrooms
Another Monday Research Review, another mushroom! If we keep this up, we’ll have to rename it “Mushroom Monday”.
But, there’s so much room for things to say, and these are fun guys to write about, as we check the science for any spore’ious claims…
Why do people take reishi?
Popular health claims for the reishi mushroom include:
- Immune health
- Cardiovascular health
- Protection against cancer
- Antioxidant qualities
- Reduced fatigue and anxiety
And does the science agree?
Let’s take a look, claim by claim:
Immune health
A lot of research for this has been in vitro (ie, with cell cultures in labs), but promising, for example:
Immunomodulating Effect of Ganoderma lucidum (Lingzhi) and Possible Mechanism
(that is the botanical name for reishi, and the Chinese name for it, by the way)
That’s not to say there are no human studies though; here it was found to boost T-cell production in stressed athletes:
Cardiovascular health
Here we found a stack of evidence for statistically insignificant improvements in assorted measures of cardiovascular health, and some studies where reishi did not outperform placebo.
Because the studies were really not that compelling, instead of taking up room (and your time) with them, we’re going to move onto more compelling, exciting science, such as…
Protection against cancer
There’s a lot of high quality research for this, and a lot of good results. The body of evidence here is so large that even back as far as 2005, the question was no longer “does it work” or even “how does it work”, but rather “we need more clinical studies to find the best doses”. Researchers even added:
❝At present, lingzhi is a health food supplement to support cancer patients, yet the evidence supporting the potential of direct in vivo anticancer effects should not be underestimated.❞
Check it out:
Anticancer effects of Ganoderma lucidum: a review of scientific evidence
Just so you know we’re not kidding about the weight of evidence, let’s drop a few extra sources:
- Ganoderma lucidum: a rational pharmacological approach to surmount cancer
- Ganoderma lucidum as an anti-cancer agent
- Extract from Ganoderma lucidum suppresses cervical cancer cell malignancy
- Ganoderma lucidum spore oil induces apoptosis of breast cancer cells
- Ganoderma lucidum enhances carboplatin chemotherapy effect
- Ganoderma lucidum inhibits prostate cancer cell migration
- Ganoderma lucidum fruiting body extracts inhibit colorectal cancer
- Inhibitory activity of medicinal mushroom Ganoderma lucidum on colorectal cancer
- Ganoderma lucidum (reishi mushroom) for cancer treatment
By the way, we shortened most of those titles for brevity, but almost all of the continued with “by” followed by a one-liner of how it does it.
So it’s not a “mysterious action” thing, it’s a “this is a very potent medicine and we know how it works” thing.
Antioxidant qualities
Here we literally only found studies to say no change was found, one that found a slight increase of antioxidant levels in urine. It’s worth noting that levels of a given thing (or its metabolites, in the case of some things) in urine are often quite unhelpful regards knowing what’s going on in the body, because we get to measure only what the body lost, not what it gained/kept.
So again, let’s press on:
Reduced fatigue and anxiety
Most of the studies for this that we could find pertained to health-related quality of life for cancer patients specifically, so (while they universally give glowing reports of reishi’s benefits to health and happiness of cancer patients), that’s a confounding factor when it comes to isolating its effects on reduction of fatigue and anxiety in people without cancer.
Here’s one that looked at it in the case of reduction of fatigue, anxiety, and other factors, in patients without cancer (but with neurathenia), in which they found it was “significantly superior to placebo with respect to the clinical improvement of symptoms”.
Summary:
- Reishi mushroom’s anti-cancer properties are very, very clear
- There is also good science to back immune health claims
- It also has been found to significantly reduce fatigue and anxiety in unwell patients (we’d love to see more studies on its benefits in otherwise healthy people, though)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: