Which Bell Peppers To Pick?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
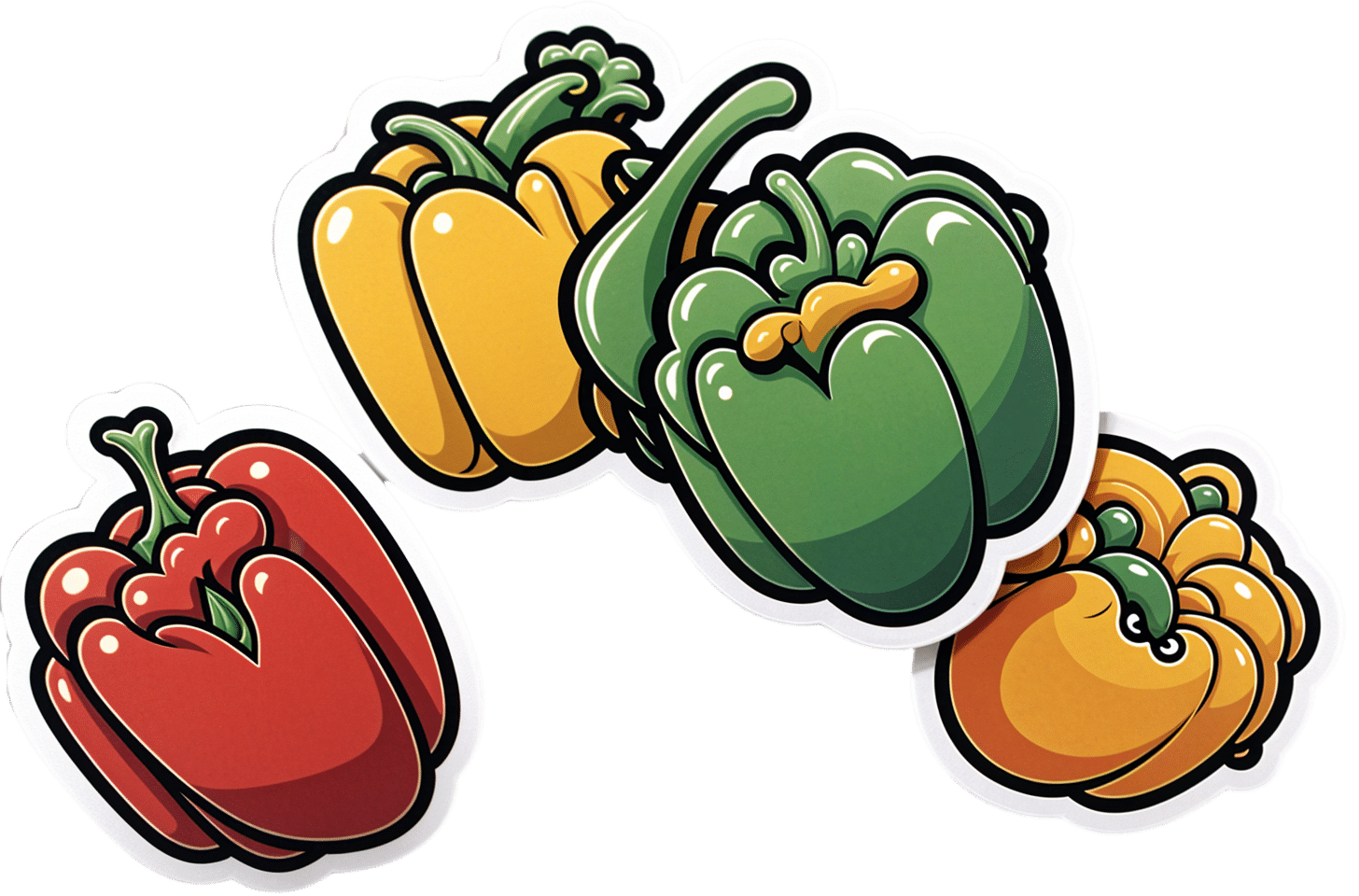
Bell Peppers: A Spectrum Of Specialties
We were going to do this as part of our ongoing “This Or That?” challenge, but as there are four main types all with many different benefits, we thought this bunch of fruits deserved a main feature.
And yes, they’re botanically fruits, even if culinarily used as vegetables—much like tomatoes, famously!
They’re all the same (but also very much not)
A thing to know is that whether bell peppers be green, yellow, orange, or red, they’re all the same plant, Capiscum anuum. All that differs is how early or late they’re harvested.
Notwithstanding the “Capiscum” genus, they don’t contain capsaicin (as is found in hot peppers). Capsaicin’s a wonderful phytochemical:
Capsaicin For Weight Loss And Against Inflammation
…but today we’re all about the bell peppers.
So, let’s see how they stack up!
💚 Green for lutein
Lutein is especially important for the eyes and [the rest of the] brain, to the point that there’s now an Alzheimer’s test that measures lutein concentration in the eye:
Green peppers have most of this important carotenoid, though the others all have some too. See also:
💛 Yellow for vitamin C
Yellow peppers are technically highest in vitamin C, but all of them contain far more than the daily dose per fruit already, so if there’s any color of pepper that’s nutritionally the most expendable, it’s yellow, since any other color pepper can take its place.
Watch out, though! Cooking destroys vitamin C, so if you want to get your Cs in, you’re going to want to do it raw.
🧡 Orange for zeaxanthin and cryptoxanthins
Similar in their benefits to lutein, these antioxidant carotenoids are found most generously in orange peppers (20x as much as in yellow, 10x as much as in red, and slightly more than in green).
❤️ Red for vitamins A & B6
Red peppers are richest by far in vitamin A, with one fruit giving the daily dose already. The others have about 10% of that, give or take.
Red peppers also have the most vitamin B6, though the others also have nearly as much.
❤️ Red for lycopene
We must do a main feature for lycopene sometime, as unlike a lot of antioxidant carotenoids, lycopene is found in comparatively very few foods (most famously it’s present in tomatoes).
Red is the only color of pepper to have lycopene.
10almonds tip: to get the most out of your lycopene, cook these ones!
Lycopene becomes 4x more bioavailable when cooked:
Lycopene in tomatoes: chemical and physical properties affected by food processing ← this paper is about tomatoes but lycopene is lycopene and this applies to the lycopene in red peppers, too
And the overall winner is…
You! Because you get to eat all four of them
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Does intermittent fasting have benefits for our brain?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Intermittent fasting has become a popular dietary approach to help people lose or manage their weight. It has also been promoted as a way to reset metabolism, control chronic disease, slow ageing and improve overall health.
Meanwhile, some research suggests intermittent fasting may offer a different way for the brain to access energy and provide protection against neurodegenerative diseases like Alzheimer’s disease.
This is not a new idea – the ancient Greeks believed fasting enhanced thinking. But what does the modern-day evidence say?
First, what is intermittent fasting?
Our diets – including calories consumed, macronutrient composition (the ratios of fats, protein and carbohydrates we eat) and when meals are consumed – are factors in our lifestyle we can change. People do this for cultural reasons, desired weight loss or potential health gains.
Intermittent fasting consists of short periods of calorie (energy) restriction where food intake is limited for 12 to 48 hours (usually 12 to 16 hours per day), followed by periods of normal food intake. The intermittent component means a re-occurrence of the pattern rather than a “one off” fast.
Food deprivation beyond 24 hours typically constitutes starvation. This is distinct from fasting due to its specific and potentially harmful biochemical alterations and nutrient deficiencies if continued for long periods.
4 ways fasting works and how it might affect the brain
The brain accounts for about 20% of the body’s energy consumption.
Here are four ways intermittent fasting can act on the body which could help explain its potential effects on the brain.
1. Ketosis
The goal of many intermittent fasting routines is to flip a “metabolic switch” to go from burning predominately carbohydrates to burning fat. This is called ketosis and typically occurs after 12–16 hours of fasting, when liver and glycogen stores are depleted. Ketones – chemicals produced by this metabolic process – become the preferred energy source for the brain.
Due to this being a slower metabolic process to produce energy and potential for lowering blood sugar levels, ketosis can cause symptoms of hunger, fatigue, nausea, low mood, irritability, constipation, headaches, and brain “fog”.
At the same time, as glucose metabolism in the brain declines with ageing, studies have shown ketones could provide an alternative energy source to preserve brain function and prevent age-related neurodegeneration disorders and cognitive decline.
Consistent with this, increasing ketones through supplementation or diet has been shown to improve cognition in adults with mild cognitive decline and those at risk of Alzheimer’s disease respectively.
2. Circadian syncing
Eating at times that don’t match our body’s natural daily rhythms can disrupt how our organs work. Studies in shift workers have suggested this might also make us more prone to chronic disease.
Time-restricted eating is when you eat your meals within a six to ten-hour window during the day when you’re most active. Time-restricted eating causes changes in expression of genes in tissue and helps the body during rest and activity.
A 2021 study of 883 adults in Italy indicated those who restricted their food intake to ten hours a day were less likely to have cognitive impairment compared to those eating without time restrictions.

Matching your eating to the active parts of your day may have brain benefits.
Shutterstock3. Mitochondria
Intermittent fasting may provide brain protection through improving mitochondrial function, metabolism and reducing oxidants.
Mitochondria’s main role is to produce energy and they are crucial to brain health. Many age-related diseases are closely related to an energy supply and demand imbalance, likely attributed to mitochondrial dysfunction during ageing.
Rodent studies suggest alternate day fasting or reducing calories by up to 40% might protect or improve brain mitochondrial function. But not all studies support this theory.
4. The gut-brain axis
The gut and the brain communicate with each other via the body’s nervous systems. The brain can influence how the gut feels (think about how you get “butterflies” in your tummy when nervous) and the gut can affect mood, cognition and mental health.
In mice, intermittent fasting has shown promise for improving brain health by increasing survival and formation of neurons (nerve cells) in the hippocampus brain region, which is involved in memory, learning and emotion.

What we eat can affect our brain, and vice versa.
ShutterstockThere’s no clear evidence on the effects of intermittent fasting on cognition in healthy adults. However one 2022 study interviewed 411 older adults and found lower meal frequency (less than three meals a day) was associated with reduced evidence of Alzheimer’s disease on brain imaging.
Some research has suggested calorie restriction may have a protective effect against Alzheimer’s disease by reducing oxidative stress and inflammation and promoting vascular health.
When we look at the effects of overall energy restriction (rather than intermittent fasting specifically) the evidence is mixed. Among people with mild cognitive impairment, one study showed cognitive improvement when participants followed a calorie restricted diet for 12 months.
Another study found a 25% calorie restriction was associated with slightly improved working memory in healthy adults. But a recent study, which looked at the impact of calorie restriction on spatial working memory, found no significant effect.
Bottom line
Studies in mice support a role for intermittent fasting in improving brain health and ageing, but few studies in humans exist, and the evidence we have is mixed.
Rapid weight loss associated with calorie restriction and intermittent fasting can lead to nutrient deficiencies, muscle loss, and decreased immune function, particularly in older adults whose nutritional needs may be higher.
Further, prolonged fasting or severe calorie restriction may pose risks such as fatigue, dizziness, and electrolyte imbalances, which could exacerbate existing health conditions.
If you’re considering intermittent fasting, it’s best to seek advice from a health professional such as a dietitian who can provide guidance on structuring fasting periods, meal timing, and nutrient intake. This ensures intermittent fasting is approached in a safe, sustainable way, tailored to individual needs and goals.

Hayley O’Neill, Assistant Professor, Faculty of Health Sciences and Medicine, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post

Infrared-Reflecting Patches For Health?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Hi! I’ve been reading about LifeWave patches, would you recommend them?❞
For reference first, this is talking about these: LifeWave.com
Short answer: no
Longer answer: their main premise seems to be that the patches (subscription prices seem to start from about $100–$300 per month) reflect infrared energy back into your body, making you more energized and healthy.
Fun fact: aluminum foil reflects infrared energy (which we feel as heat), by the way, and that is why space blankets (of the kind used in emergencies and by some athletes) are made shiny like that, often with aluminized mylar.
We cannot comment too closely on the rest of the presented science of their products, as it seems quite unlike anything we’re accustomed to reading, and we were not able to make a lot of sense of it.
They do cite research papers to back their claims, including research conducted by the company’s founder and published via an open journal.
Many others are independent studies conducted by often the same researchers as each other, mostly experts in acupuncture and acupressure.
For the papers we looked at, the sample sizes were very small, but the conclusions were very positive.
They were published in a variety of journals, of which we cannot claim any prior knowledge (i.e:, they were not the peer-reviewed journals from which we cite most of our sources).
Also, none were registered with ClinicalTrials.gov.
To be on the safe side, their disclaimer does advise:
❝LifeWave products are only intended to maintain or encourage a general state of health or healthy activity and are not intended to diagnose, treat, cure, mitigate, or prevent any disease or medical condition of the body❞
They do have a Frequently Asked Questions page, which tells about ancient Egyptian use of colored glass, as well as more modern considerations including joining, ordering, their commissions system, binary commissions and matching bonuses, and “how to rank up in LifeWave” as well as a lot of information about subscribing as a preferred customer or a brand partner, opting in to their multi-level marketing opportunities.
Here’s what “Honest Brand Reviews” had to say:
Honest Brand Reviews | LifeWave Review
Our position:
We cannot honestly claim to understand their science, and thus naturally won’t actively recommend what we can’t speak for.
An expert’s position:
Since we couldn’t understand how this would work, here’s what Dr. Paul Knoepfler has to say about their flagship product, the LifeWave X39 patch:
LifeWave X39 stem cell patch story has holes
Take care!
Share This Post

Woman Petitions Health Insurer After Company Approves — Then Rejects — Her Infusions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When KFF Health News published an article in August about the “prior authorization hell” Sally Nix said she went through to secure approval from her insurance company for the expensive monthly infusions she needs, we thought her story had a happy ending.
That’s because, after KFF Health News sent questions to Nix’s insurance company, Blue Cross Blue Shield of Illinois, it retroactively approved $36,000 worth of treatments she thought she owed. Even better, she also learned she would qualify for the infusions moving forward.
Good news all around — except it didn’t last for long. After all, this is the U.S. health care system, where even patients with good insurance aren’t guaranteed affordable care.
To recap: For more than a decade, Nix, of Statesville, North Carolina, has suffered from autoimmune diseases, chronic pain, and fatigue, as well as a condition called trigeminal neuralgia, which is marked by bouts of electric shock-like pain that’s so intense it’s commonly known as the “suicide disease.”
“It is a pain that sends me to my knees,” Nix said in October. “My entire family’s life is controlled by the betrayal of my body. We haven’t lived normally in 10 years.”
Late in 2022, Nix started receiving intravenous immunoglobulin infusions to treat her diseases. She started walking two miles a day with her service dog. She could picture herself celebrating, free from pain, at her daughter’s summer 2024 wedding.
“I was so hopeful,” she said.
But a few months after starting those infusions, she found out that her insurance company wouldn’t cover their cost anymore. That’s when she started “raising Cain about it” on Instagram and Facebook.
You probably know someone like Sally Nix — someone with a chronic or life-threatening illness whose doctor says they need a drug, procedure, or scan, and whose insurance company has replied: No.
Prior authorization was conceived decades ago to rein in health care costs by eliminating duplicative and ineffective treatment. Not only does overtreatment waste billions of dollars every year, but doctors acknowledge it also potentially harms patients.
However, critics worry that prior authorization has now become a way for health insurance companies to save money, sometimes at the expense of patients’ lives. KFF Health News has heard from hundreds of people in the past year relating their prior authorization horror stories.
When we first met Nix, she was battling her insurance company to regain authorization for her infusions. She’d been forced to pause her treatments, unable to afford $13,000 out-of-pocket for each infusion.
Finally, it seemed like months of her hard work had paid off. In July, Nix was told by staff at both her doctor’s office and her hospital that Blue Cross Blue Shield of Illinois would allow her to restart treatment. Her balance was marked “paid” and disappeared from the insurer’s online portal.
But the day after the KFF Health News story was published, Nix said, she learned the message had changed. After restarting treatment, she received a letter from the insurer saying her diagnoses didn’t actually qualify her for the infusions. It felt like health insurance whiplash.
“They’re robbing me of my life,” she said. “They’re robbing me of so much, all because of profit.”
Dave Van de Walle, a spokesperson for Blue Cross Blue Shield of Illinois, said the company would not discuss individual patients’ cases.
“Prior authorization is often a requirement for certain treatments,” Van de Walle said in a written statement, “and BCBSIL administers benefits according to medical policy and the employer’s benefit.”
But Nix is a Southern woman of the “Steel Magnolia” variety. In other words, she’s not going down without a fight.
In September, she called out her insurance company’s tactics in a http://change.org/ campaign that has garnered more than 21,000 signatures. She has also filed complaints against her insurance company with the U.S. Department of Health and Human Services, U.S. Department of Labor, Illinois Department of Insurance, and Illinois attorney general.
Even so, Nix said, she feels defeated.
Not only is she still waiting for prior authorization to restart her immunoglobulin infusions, but her insurance company recently required Nix to secure preapproval for another treatment — routine numbing injections she has received for nearly 10 years to treat the nerve pain caused by trigeminal neuralgia.
“It is reprehensible what they’re doing. But they’re not only doing it to me,” said Nix, who is now reluctantly taking prescription opioids to ease her pain. “They’re doing it to other patients. And it’s got to stop.”
Do you have an experience with prior authorization you’d like to share? Click here to tell your story.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Share This Post
Related Posts

Tasty Versatile Rice
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the nearish future, we’re going to do some incredible rice dishes, but first we need to make sure we’re all on the same page about cooking rice, so here’s a simple recipe first, to get technique down and work in some essentials. We’ll be using wholegrain basmati rice, because it has a low glycemic index, lowest likelihood of heavy metal contamination (a problem for some kinds of rice), and it’s one of the easiest rices to cook well.
You will need
- 1 cup wholegrain basmati rice (it may also be called “brown basmati rice“; this is the same)
- 1 1/2 cups vegetable stock (ideally you have made this yourself from vegetable offcuts that you saved in the freezer, then it will be healthiest and lowest in sodium; failing that, low-sodium vegetable stock cubes can be purchased at most large supermarkets. and then made up at home with hot water)
- 1 tbsp extra virgin olive oil
- 1 tbsp chia seeds
- 1 tbsp black pepper, coarse ground
- 1 tsp turmeric powder (this small quantity will not change the flavor, but it has important health benefits, and also makes the rice a pleasant golden color)
- 1 tsp garlic powder
- 1 tsp yeast extract (this gently improves the savory flavor and also adds vitamin B12)
- Optional small quantity of green herbs for garnish. Cilantro is good (unless you have the soap gene); parsley never fails.
This is the ingredients list for a super-basic rice that will go with anything rice will go with; another day we can talk more extensive mixes of herbs and spice blends for different kinds of dishes (and different health benefits!), but for now, let’s get going!
Method
(we suggest you read everything at least once before doing anything)
1) Wash the rice thoroughly. We recommend using a made-for-purpose rice-washing bowl (like this one, for example), but failing that, simply rinse it thoroughly with cold water using a bowl and a sieve. You will probably need to rinse it 4–5 times, but with practice, it will only take a few seconds per rinse, and the water will be coming up clear.
2) Warm the pan. It doesn’t matter for the moment whether you’re using an electronic rice cooker, a stovetop pressure cooker, electronic pressure cooker, or just a sturdy pan with a heavy lid available, aside from that if it’s something non-stovetop, you now want it to be on low to warm up already.
3) Separately in a saucepan, bring your stock to a simmer
4) Put the tbsp of olive oil into the pan (even if you’re confident the rice won’t stick; this isn’t entirely about that) and turn up the heat (if it’s a very simple rice cooker, most at least have a warm/cook differentiation; if so, turn it to “cook”). You don’t want the oil to get to the point of smoking, so, to test the temperature as it heats, flick a single drop of water from your fingertip (you did wash your hands first, right? We haven’t been including that step, but please do wash your hands before doing kitchen things) into the pan. If it sizzles, the pan is hot enough now for the next step.
5) Put the rice into the pan. That’s right, with no extra liquid yet; we’re going to toast it for a moment. Stir it a little, for no more than a minute; keep it moving; don’t let it burn! If you try this several times and fail, it could be that you need a better pan. Treat yourself to one when you get the opportunity; until then, skip the toasting part if necessary.
6) Add the chia seeds and spices, followed by the stock, followed by the yeast extract. Why did we do the stock before the yeast extract? It’s because hot liquid will get all the yeast extract off the teaspoon 🙂
7) Put the lid on/down (per what kind of pan or rice cooker you are using), and turn up the heat (if it is a variable heat source) until a tiny bit of steam starts making its way out. When it does, turn it down to a simmer, and let the rice cook. Don’t stir it, don’t jiggle it; trust the process. If you stir or jiggle it, the rice will cook unevenly and, paradoxically, probably stick.
8) Do keep an eye on it, because when steam stops coming out, it is done, and needs taking off the heat immediately. If using an automatic rice cooker, you can be less attentive if you like, because it will monitor this for you.
Note: if you are using a simple pan with a non-fastening lid (any other kind of rice cooking setup is better), more steam will escape than the other methods, and it’s possible that it might run out of steam (literally) before the rice is finished. If the steam stops and you find the rice isn’t done, add a splash of water as necessary (the rice doesn’t need to be submerged, it just needs to have liquid; the steam is part of the cooking process), and make a note of how much you had to add (so that next time you can just add it at the start), and put it back on the heat until it is done.
9) Having taken it off the heat, let it sit for 5 minutes (with the lid still on) before doing any fluffing-up. Then you can fluff-up and serve, adding the garnish if you want one.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Should You Go Light Or Heavy On Carbs?
- Chia: The Tiniest Seeds With The Most Value
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Why Curcumin (Turmeric) Is Worth Its Weight In Gold
- The Many Health Benefits Of Garlic
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

The Fascinating Truth About Aspartame, Cancer, & Neurotoxicity
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is Aspartame’s Reputation Well-Deserved?

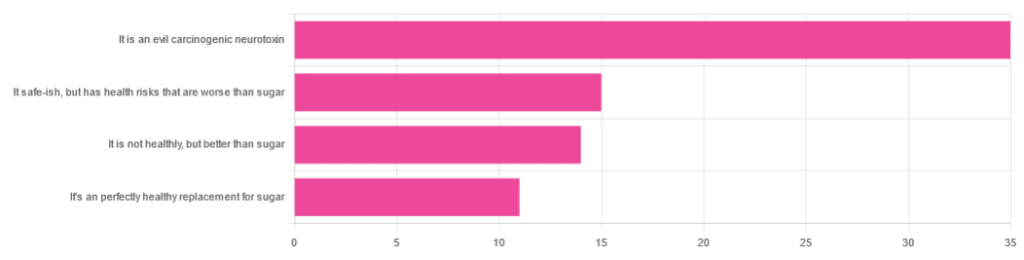
In Tuesday’s newsletter, we asked you for your health-related opinions on aspartame, and got the above-depicted, below-described, set of responses:
- About 47% said “It is an evil carcinogenic neurotoxin”
- 20% said “It is safe-ish, but has health risks that are worse than sugar”
- About 19% said “It is not healthy, but better than sugar”
- About 15% said “It’s a perfectly healthy replacement for sugar”
But what does the science say?
Aspartame is carcinogenic: True or False?
False, assuming consuming it in moderation. In excess, almost anything can cause cancer (oxygen is a fine example). But for all meaningful purposes, aspartame does not appear to be carcinogenic. For example,
❝The results of these studies showed no evidence that these sweeteners cause cancer or other harms in people.❞
~ NIH | National Cancer Institute
Source: Artificial Sweeteners and Cancer
Plenty of studies and reviews have also confirmed this; here are some examples:
- Evaluation of aspartame cancer epidemiology studies based on quality appraisal criteria
- Aspartame, low-calorie sweeteners and disease: Regulatory safety and epidemiological issues
- Aspartame: A review of genotoxicity data
Why then do so many people believe it causes cancer, despite all the evidence against it?
Well, there was a small study involving giving megadoses to rats, which did increase their cancer risk. So of course, the popular press took that and ran with it.
But those results have not been achieved outside of rats, and human studies great and small have all been overwhelmingly conclusive that moderate consumption of aspartame has no effect on cancer risk.
Aspartame is a neurotoxin: True or False?
False, again assuming moderate consumption. If you’re a rat being injected with a megadose, your experience may vary. But a human enjoying a diet soda, the aspartame isn’t the part that’s doing you harm, so far as we know.
For example, the European Food Safety Agency’s scientific review panel concluded:
❝there is still no substantive evidence that aspartame can induce such effects❞
~ Dr. Atkin et al (it was a pan-European team of 21 experts in the field)
Source: Report on the Meeting on Aspartame with National Experts
See also,
❝The data from the extensive investigations into the possibility of neurotoxic effects of aspartame, in general, do not support the hypothesis that aspartame in the human diet will affect nervous system function, learning or behavior.
The weight of existing evidence is that aspartame is safe at current levels of consumption as a nonnutritive sweetener.❞
and
❝The safety testing of aspartame has gone well beyond that required to evaluate the safety of a food additive.
When all the research on aspartame, including evaluations in both the premarketing and postmarketing periods, is examined as a whole, it is clear that aspartame is safe, and there are no unresolved questions regarding its safety under conditions of intended use.❞
Source: Regulatory Toxicology & Pharmacology | Aspartame: Review of Safety
Why then do many people believe it is a neurotoxin? This one can be traced back to a chain letter hoax from about 26 years ago; you can read it here, but please be aware it is an entirely debunked hoax:
Urban Legends | Aspartame Hoax
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

What is pathological demand avoidance – and how is it different to ‘acting out’?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Charlie” is an eight-year-old child with autism. Her parents are worried because she often responds to requests with insults, aggression and refusal. Simple demands, such as being asked to get dressed, can trigger an intense need to control the situation, fights and meltdowns.
Charlie’s parents find themselves in a constant cycle of conflict, trying to manage her and their own reactions, often unsuccessfully. Their attempts to provide structure and consequences are met with more resistance.
What’s going on? What makes Charlie’s behaviour – that some are calling “pathological demand avoidance” – different to the defiance most children show their parents or carers from time-to-time?
What is pathological demand avoidance?
British developmental psychologist Elizabeth Newson coined the term “pathological demand avoidance” (commonly shortened to PDA) in the 1980s after studying groups of children in her practice.
A 2021 systematic review noted features of PDA include resistance to everyday requests and strong emotional and behavioural reactions.
Children with PDA might show obsessive behaviour, struggle with persistence, and seek to control situations. They may struggle with attention and impulsivity, alongside motor and coordination difficulties, language delay and a tendency to retreat into role play or fantasy worlds.
PDA is also known as “extreme demand avoidance” and is often described as a subtype of autism. Some people prefer the term persistent drive for autonomy or pervasive drive for autonomy.
What does the evidence say?
Every clinician working with children and families recognises the behavioural profile described by PDA. The challenging question is why these behaviours emerge.
PDA is not currently listed in the two diagnostic manuals used in psychiatry and psychology to diagnose mental health and developmental conditions, the current Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the World Health Organization’s International Classification of Diseases (ICD-11).
Researchers have reported concerns about the science behind PDA. There are no clear theories or explanations of why or how the profile of symptoms develop, and little inclusion of children or adults with lived experience of PDA symptoms in the studies. Environmental, family or other contextual factors that may contribute to behaviour have not been systematically studied.
A major limitation of existing PDA research and case studies is a lack of consideration of overlapping symptoms with other conditions, such as autism, attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder, anxiety disorder, selective mutism and other developmental disorders. Diagnostic labels can have positive and negative consequences and so need to be thoroughly investigated before they are used in practice.
Classifying a “new” condition requires consistency across seven clinical and research aspects: epidemiological data, long-term patient follow-up, family inheritance, laboratory findings, exclusion from other conditions, response to treatment, and distinct predictors of outcome. At this stage, these domains have not been established for PDA. It is not clear whether PDA is different from other formal diagnoses or developmental differences.

When a child is stressed, demands or requests might tip them into fight, flight or freeze mode. Shutterstock Finding the why
Debates over classification don’t relieve distress for a child or those close to them. If a child is “intentionally” engaged in antisocial behaviour, the question is then “why?”
Beneath the behaviour is almost always developmental difference, genuine distress and difficulty coping. A broad and deep understanding of developmental processes is required.
Interestingly, while girls are “under-represented” in autism research, they are equally represented in studies characterising PDA. But if a child’s behaviour is only understood through a “pathologising” or diagnostic lens, there is a risk their agency may be reduced. Underlying experiences of distress, sensory overload, social confusion and feelings of isolation may be missed.
So, what can be done to help?
There are no empirical studies to date regarding PDA treatment strategies or their effectiveness. Clinical advice and case studies suggest strategies that may help include:
- reducing demands
- giving multiple options
- minimising expectations to avoid triggering avoidance
- engaging with interests to support regulation.
Early intervention in the preschool and primary years benefits children with complex developmental differences. Clinical care that involves a range of medical and allied health clinicians and considers the whole person is needed to ensure children and families get the support they need.
It is important to recognise these children often feel as frustrated and helpless as their caregivers. Both find themselves stuck in a repetitive cycle of distress, frustration and lack of progress. A personalised approach can take into account the child’s unique social, sensory and cognitive sensitivities.
In the preschool and early primary years, children have limited ability to manage their impulses or learn techniques for managing their emotions, relationships or environments. Careful watching for potential triggers and then working on timetables and routines, sleep, environments, tasks, and relationships can help.
As children move into later primary school and adolescence, they are more likely to want to influence others and be able to have more self control. As their autonomy and ability to collaborate increases, the problematic behaviours tend to reduce.
Strategies that build self-determination are crucial. They include opportunities for developing confidence, communication and more options to choose from when facing challenges. This therapeutic work with children and families takes time and needs to be revisited at different developmental stages. Support to engage in school and community activities is also needed. Each small step brings more capacity and more effective ways for a child to understand and manage themselves and their worlds.
What about Charlie?
The current scope to explain and manage PDA is limited. Future research must include the voices and views of children and adults with PDA symptoms.
Such emotional and behavioural difficulties are distressing and difficult for children and families. They need compassion and practical help.
For a child like Charlie, this could look like a series of sessions where she and her parents meet with clinicians to explore Charlie’s perspective, experiences and triggers. The family might come to understand that, in addition to autism, Charlie has complex developmental strengths and challenges, anxiety, and some difficulties with adjustment related to stress at home and school. This means Charlie experiences a fight, flight, freeze response that looks like aggression, avoidance or shutting down.
With carefully planned supports at home and school, Charlie’s options can broaden and her distress and avoidance can soften. Outside the clinic room, Charlie and her family can be supported to join an inclusive local community sporting or creative activity. Gradually she can spend more time engaged at home, school and in the community.
Nicole Rinehart, Professor, Child and Adolescent Psychology, Director, Krongold Clinic (Research), Monash University; David Moseley, Senior Research Fellow, Deputy Director (Clinical), Monash Krongold Clinic, Monash University, and Michael Gordon, Associate Professor, Psychiatry, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: