Cottage Cheese vs Ricotta – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cottage cheese to ricotta, we picked the ricotta.
Why?
Cottage cheese is a famous health food, mostly for being a low-fat, low-carb, source of protein. And yet, ricotta beats it in most respects.
Looking at the macros first, cottage cheese has more carbs, while ricotta has more protein and fat. The fat profile is pretty much the same, and in both cases it’s two thirds saturated fat, which isn’t good in either case, but cottage cheese has less overall fat which means less saturated fat in total even if the percentage is the same. Because the difference in carbs and protein is not large, while ricotta has considerably more fat, we’ll call this category a win for cottage cheese.
In terms of vitamins, cottage cheese has more of vitamins B1, B5, and B12, while ricotta has more of vitamins A, B2, B3, B9, D, E, and K, so this one’s a win for ricotta.
In the category of minerals, cottage cheese has slightly more copper, while ricotta has much more calcium, iron, magnesium, manganese, potassium, selenium, and zinc. In particular, 2.5x more calcium, and 5x more iron! An easy and clear win for ricotta here.
Taking everything into account: yes, cottage cheese has less fat (and thus, in total, less saturated fat, although the percentage is the same), but that doesn’t make up for ricotta winning in pretty much every other respect. Still, enjoy either or both (in moderation!) if you be so inclined.
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
CLA for Weight Loss?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Conjugated Linoleic Acid for Weight Loss?
You asked us to evaluate the use of CLA for weight loss, so that’s today’s main feature!
First, what is CLA?
Conjugated Linoleic Acid (CLA) is a fatty acid made by grazing animals. Humans don’t make it ourselves, and it’s not an essential nutrient.
Nevertheless, it’s a popular supplement, mostly sold as a fat-burning helper, and thus enjoyed by slimmers and bodybuilders alike.
❝CLA reduces bodyfat❞—True or False?
True! Contingently. Specifically, it will definitely clearly help in some cases. For example:
- This study found it doubled fat loss in chickens
- It significantly increased delipidation of white adipose tissue in these mice
- The mice in this study enjoyed a 43–88% reduction in (fatty) weight gain
- Over the course of a six-week weight-loss program, these mice got 70% more weight loss on CLA, compared to placebo
- In this study, pigs that took CLA on a high-calorie diet gained 50% less weight than those not taking CLA
- On a heart-unhealthy diet, these hamsters taking CLA gained much less white adipose tissue than their comrades not taking CLA
- Another study with pigs found that again, CLA supplementation resulted in much less weight gained
- These hamsters being fed a high-cholesterol diet found that those taking CLA ended up with a leaner body mass than those not taking CLA
- This study with mice found that CLA supplementation promoted fat loss and lean muscle gain
Did you notice a theme? It’s Animal Farm out there!
❝CLA reduces bodyfat in humans❞—True or False?
False—practically. Technically it appears to give non-significantly better results than placebo.
A comprehensive meta-analysis of 18 different studies (in which CLA was provided to humans in randomized, double-blinded, placebo-controlled trials and in which body composition was assessed by using a validated technique) found that, on average, human CLA-takers lost…
Drumroll please…
00.00–00.05 kg per week. That’s between 0–50g per week. That’s less than two ounces. Put it this way: if you were to quickly drink an espresso before stepping on the scale, the weight of your very tiny coffee would cover your fat loss.
The reviewers concluded:
❝CLA produces a modest loss in body fat in humans❞
Modest indeed!
See for yourself: Efficacy of conjugated linoleic acid for reducing fat mass: a meta-analysis in humans
But what about long-term? Well, as it happens (and as did show up in the non-human animal studies too, by the way) CLA works best for the first four weeks or so, and then effects taper off.
Another review of longer-term randomized clinical trials (in humans) found that over the course of a year, CLA-takers enjoyed on average a 1.33kg total weight loss benefit over placebo—so that’s the equivalent of about 25g (0.8 oz) per week. We’re talking less than a shot glass now.
They concluded:
❝The evidence from RCTs does not convincingly show that CLA intake generates any clinically relevant effects on body composition on the long term❞
A couple of other studies we’ll quickly mention before closing this section:
- CLA supplementation does not affect waist circumference in humans (at all).
- Amongst obese women doing aerobic exercise, CLA supplementation has no effect (at all) on body fat reduction compared to placebo
What does work?
You may remember this headline from our “What’s happening in the health world” section a few days ago:
Research reveals self-monitoring behaviors and tracking tools key to long-term weight loss success
On which note, we’ve mentioned before, we’ll mention again, and maybe one of these days we’ll do a main feature on it, there’s a psychology-based app/service “Noom” that’s very personalizable and helps you reach your own health goals, whatever they might be, in a manner consistent with any lifestyle considerations you might want to give it.
Curious to give it a go? Check it out at Noom.com (you can get the app there too, if you want)
Share This Post
-
Broad Beans vs Sweetcorn – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing broad beans to sweetcorn, we picked the broad beans.
Why?
Firstly, you may be wondering: “aren’t broad beans fava beans?”, and yes, yes they are, but by convention, broad beans are the young green beans, while fava beans are the mature beans of the plant. Similar situation to the relationship between edamame and soybeans. And, in both cases, you’re more likely to put the young green beans in a salad, thus making the broad beans the more reasonable vegetable to compare to the sweetcorn. On which note…
In terms of macros, the broad beans have more protein and fiber, while the sweetcorn has more carbs. We call that a win for the beans.
Looking at the vitamins, the broad beans have (barely) more vitamin B6, while the sweetcorn has more of vitamins A, B1, B2, B5, B9, E, and choline. An easy win for the corn this time.
In the category of minerals, the situation is reversed: broad beans have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while sweetcorn is not higher in any minerals. So, a clear win for the beans.
Adding up the sections gives a 2:1 win for the beans over the corn, but by all means enjoy either or both—together is great, and diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Share This Post
-
Early Bird Or Night Owl? Genes vs Environment
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Sliding Slope?
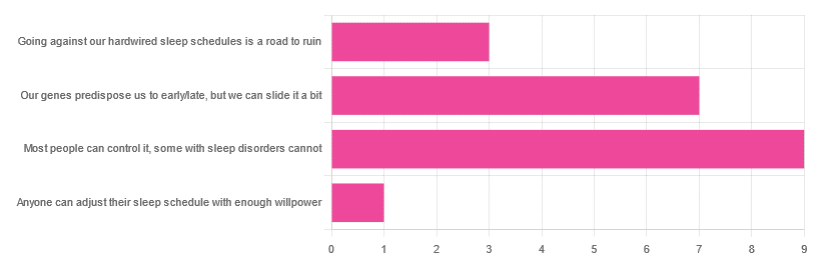
In Tuesday’s newsletter, we asked you how much control you believe we have over our sleep schedule, and got the above-depicted, below-described, set of responses:
- 45% said “most people can control it; some people with sleep disorders cannot
- 35% said “our genes predispose us to early/late, but we can slide it a bit
- 15% said: “going against our hardwired sleep schedules is a road to ruin”
- 5% said “anyone can adjust their sleep schedule with enough willpower”
You may be wondering: what’s with those single-digit numbers in the graph there? And the answer is: Tuesday’s email didn’t go out at the usual time due to a scheduling mistake (sorry!), which is probably what affected the number of responses (poll response levels vary, but are usually a lot higher than this).
Note: yes, this does mean most people who read our newsletter don’t vote. So, not to sound like a politician on the campaign trail, but… Your vote counts! We always love reading your comments when you add those, too—often they provide context that allow us to tailor what we focus on in our articles
However, those are the responses we got, so here we are!
What does the science say?
Anyone can adjust their sleep with enough willpower: True or False?
False, simply. It’s difficult for most people, but for many people with sleep disorders, it is outright impossible.
In a battle of narcolepsy vs willpower, for example, no amount of willpower will stop the brain from switching to sleep mode when it thinks it’s time to sleep:
❝Narcolepsy is the most common neurological cause of chronic sleepiness. The discovery about 20 years ago that narcolepsy is caused by selective loss of the neurons producing orexins sparked great advances in the field
[There is also] developing evidence that narcolepsy is an autoimmune disorder that may be caused by a T cell-mediated attack on the orexin neurons and explain how these new perspectives can inform better therapeutic approaches.❞
~ Dr. Carrie Mahoney et al. (lightly edited for brevity)
Source: The neurobiological basis of narcolepsy
For further reading, especially if this applies to you or a loved one:
Our genes predispose us to early/late, but we can slide it a bit: True or False?
True! First, about our genes predisposing us:
…and also:
Gene distinguishes early birds from night owls and helps predict time of death
Now, as for the “can slide it a bit”, this is really just a function of the general categories of “early bird” and “night owl” spanning periods of time that allow for a few hours’ wiggle-room at either side.
However, it is recommended to make any actual changes more gradually, with the Sleep Foundation going so far as to recommend 30 minutes, or even just 15 minutes, of change per day:
Sleep Foundation | How to Fix Your Sleep Schedule
Going against our hardwired sleep schedule is a road to ruin: True or False?
False, contextually. By this we mean: our “hardwired” sleep schedule is (for most of us), genetically predisposed but not predetermined.
Also, genetic predispositions are not necessarily always good for us; one would not argue, for example, for avoiding going against a genetic predisposition to addiction.
Some genetic predispositions are just plain bad for us, and genes can be a bit of a lottery.
That said, we do recommend getting some insider knowledge (literally), by getting personal genomics tests done, if that’s a viable option for you, so you know what’s really a genetic trait (and what to do with that information) and what’s probably caused by something else (and what to do with that information):
Genetic Testing: Health Benefits & Methods
Take care!
Share This Post
Related Posts
-
Darwin’s Bed Rest: Worthwhile Idea?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I recall that Charles Darwin (of Evolution fame) used to spend a day a month in bed in order to maintain his physical and psychological equilibrium. Do you see merit in the idea?❞
Well, it certainly sounds wonderful! Granted, it may depend on what you do in bed :p
Descartes did a lot of his work from bed (and also a surprising amount of it while hiding in an oven, but that’s another story), which was probably not so good for the health.
As for Darwin, his health was terrible in quite a lot of ways, so he may not be a great model.
However! Certainly taking a break is well-established as an important and healthful practice:
How To Rest More Efficiently (Yes, Really)
❝I don’t like to admit it but I am getting old. Recently, I had my first “fall” (ominous word!) I was walking across some wet decking and, before I knew what had happened, my feet were shooting forwards, and I crashed to the ground. Luckily I wasn’t seriously damaged. But I was wondering whether you can give us some advice about how best to fall. Maybe there are some good videos on the subject? I would like to be able to practice falling so that it doesn’t come as such a shock when it happens!❞
This writer has totally done the same! You might like our recent main feature on the topic:
…if you’ll pardon the pun
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How we treat catchment water to make it safe to drink
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most of us are fortunate that, when we turn on the tap, clean, safe and high-quality water comes out.
But a senate inquiry into the presence of PFAS or “forever chemicals” is putting the safety of our drinking water back in the spotlight.
Lidia Thorpe, the independent senator leading the inquiry, says Elders in the Aboriginal community of Wreck Bay in New South Wales are “buying bottled water out of their aged care packages” due to concerns about the health impacts of PFAS in their drinking water.
So, how is water deemed safe to drink in Australia? And why does water quality differ in some areas?
Here’s what happens between a water catchment and your tap.
Andriana Syvanych/Shutterstock Human intervention in the water cycle
There is no “new” water on Earth. The water we drink can be up to 4.5 billion years old and is continuously recycled through the hydrological cycle. This transfers water from the ground to the atmosphere through evaporation and back again (for example, through rain).
Humans interfere with this natural cycle by trapping and redirecting water from various sources to use. A lot happens before it reaches your home.
The quality of the water when you turn on the tap depends on a range of factors, including the local geology, what kind of activities happen in catchment areas, and the different treatments used to process it.
Maroondah dam in Healesville, Victoria. doublelee/Shutterstock How do we decide what’s safe?
The Australian Drinking Water Guidelines define what is considered safe, good-quality drinking water.
The guidelines set acceptable water quality values for more than 250 physical, chemical and bacterial contaminants. They take into account any potential health impact of drinking the contaminant over a lifetime as well as aesthetics – the taste and colour of the water.
The guidelines are not mandatory but provide the basis for determining if the quality of water to be supplied to consumers in all parts of Australia is safe to drink. The guidelines undergo rolling revision to ensure they represent the latest scientific evidence.
From water catchment to tap
Australians’ drinking water mainly comes from natural catchments. Sources include surface water, groundwater and seawater (via desalination).
Public access to these areas is typically limited to preserve optimal water quality.
Filtration and purification of water occurs naturally in catchments as it passes through soil, sediments, rocks and vegetation.
But catchment water is subject to further treatment via standard processes that typically focus on:
- removing particulates (for example, soil and sediment)
- filtration (to remove particles and their contaminants)
- disinfection (for example, using chlorine and chloramine to kill bacteria and viruses)
- adding fluoride to prevent tooth decay
- adjusting pH to balance the chemistry of the water and to aid filtration.
This water is delivered to our taps via a reticulated system – a network of underground reservoirs, pipes, pumps and fittings.
In areas where there is no reticulated system, drinking water can also be sourced from rainwater tanks. This means the quality of drinking water can vary.
Sources of contamination can come from roof catchments feeding rainwater tanks as well from the tap due to lead in plumbing fittings and materials.
So, does all water meet these standards?
Some rural and remote areas, especially First Nations communities, rely on poor-quality surface water and groundwater for their drinking water.
Rural and regional water can exceed recommended guidelines for salt, microbial contaminants and trace elements, such as lead, manganese and arsenic.
The federal government and other agencies are trying to address this.
There are many impacts of poor regional water quality. These include its implication in elevated rates of tooth decay in First Nations people. This occurs when access to chilled, sugary drinks is cheaper and easier than access to good quality water.
What about PFAS?
There is also renewed concern about the presence of PFAS or “forever” chemicals in drinking water.
Recent research examining the toxicity of PFAS chemicals along with their presence in some drinking water catchments in Australia and overseas has prompted a recent assessment of water source contamination.
A review by the National Health and Medical Research Council (NHMRC) proposed lowering the limits for four PFAS chemicals in drinking water: PFOA, PFOS, PFHxS and PFBS.
The review used publicly available data and found most drinking water supplies are currently below the proposed new guideline values for PFAS.
However, “hotspots” of PFAS remain where drinking water catchments or other sources (for example, groundwater) have been impacted by activities where PFAS has been used in industrial applications. And some communities have voiced concerns about an association between elevated PFAS levels in their communities and cancer clusters.
While some PFAS has been identified as carcinogenic, it’s not certain that PFAS causes cancer. The link is still being debated.
Importantly, assessment of exposure levels from all sources in the population shows PFAS levels are falling meaning any exposure risk has also reduced over time.
How about removing PFAS from water?
Most sources of drinking water are not associated with industrial contaminants like PFAS. So water sources are generally not subject to expensive treatment processes, like reverse osmosis, that can remove most waterborne pollutants, including PFAS. These treatments are energy-intensive and expensive and based on recent water quality assessments by the NHMRC will not be needed.
While contaminants are everywhere, it is the dose that makes the poison. Ultra-low concentrations of chemicals including PFAS, while not desirable, may not be harmful and total removal is not warranted.
Mark Patrick Taylor, Chief Environmental Scientist, EPA Victoria; Honorary Professor, School of Natural Sciences, Macquarie University; Antti Mikkonen, Principal Health Risk Advisor – Chemicals, EPA Victoria, and PhD graduate, School of Pharmacy and Medical Sciences, University of South Australia, and Minna Saaristo, Research Affiliate in the School of Biological Sciences, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A Statin-Free Life – by Dr. Aseem Malhotra
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Here at 10almonds, we’ve written before about the complexities of statins, and their different levels of risk/benefit for men and women, respectively. It’s a fascinating topic, and merits more than an article of the size we write here!
So, in the spirit of giving pointers of where to find a lot more information, this book is a fine choice.
Dr. Malhotra, a consultant cardiologist and professor of evidence-based medicine, talks genes and lifestyle, drugs and blood. He takes us on a tour of the very many risk factors for heart disease, and how cholesterol levels may be at best an indicator, but less likely a cause, of heart disease, especially for women. Further and even better, he discusses various more reliable indicators and potential causes, too.
Rather than be all doom and gloom, he does offer guidance on how to reduce each of one’s personal risk factors and—which is important—keep on top of the various relevant measures of heart health (including some less commonly tested ones, like the coronary calcium score).
The style is light reading andyet with a lot of reference to hard science, so it’s really the best of both worlds in that regard.
Bottom line: if you’re considering statins, or are on statins and are reconsidering that choice, then this book will (notwithstanding its own bias in its conclusion) help you make a more-informed decision.
Click here to check out A Statin-Free Life, and make the best choice for you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: