Celery vs Radish – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to radish, we picked the celery.
Why?
It was very close! And yes, surprising, we know. Generally speaking, the more colorful/pigmented an edible plant is, the healthier it is. Celery is just one of those weird exceptions (as is cauliflower, by the way).
Macros-wise, these two are pretty much the same—95% water, with just enough other stuff to hold them together. The proportions of “other stuff” are also pretty much equal.
In the category of vitamins, celery has more vitamin K while radish has more vitamin C; the other vitamins are pretty close to equal. We’ll call this one a minor win for celery, as vitamin K is found in fewer foods than vitamin C.
When it comes to minerals, celery has more calcium, manganese, phosphorus, and potassium, while radish has more copper, iron, selenium, and zinc. We’ll call this a minor win for radish, as the margins are a little wider for its minerals.
So, that makes the score 1–1 so far.
Both plants have an assortment of polyphenols, of which, when we add up the averages, celery comes out on top by some way. Celery also comes out on top when we do a head-to-head of the top flavonoid of each; celery has 5.15mg/100g of apigenin to radish’s 0.63mg/100g kaempferol.
Which means, both are great healthy foods, but celery wins the day.
Want to learn more?
You might like to read:
Celery vs Cucumber – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Rebalancing Dopamine (Without “Dopamine Fasting”)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Rebalancing Dopamine (Without “Dopamine Fasting”)
Credit Steve Fisch This is Dr. Anna Lembke. She’s a professor of psychiatry at Stanford, and chief of the Stanford Addiction Medicine Dual Diagnosis Clinic—as well as running her own clinical practice, and serving on the board of an array of state and national addiction-focused organizations.
Today we’re going to look at her work on dopamine management…
Getting off the hedonic treadmill
For any unfamiliar with the term, the “hedonic treadmill” is what happens when we seek pleasure, enjoy the pleasure, the pleasure becomes normalized, and now we need to seek a stronger pleasure to get above our new baseline.
In other words, much like running on a reciprocal treadmill that just gets faster the faster we run.
What Dr. Lembke wants us to know here: pleasure invariably leads to pain
This is not because of some sort of extrinsic moral mandate, nor even in the Buddhist sense. Rather, it is biology.
Pleasure and pain are processed by the same part of the brain, and if we up one, the other will be upped accordingly, to try to keep a balance.
Consequently, if we recklessly seek “highs”, we’re going to hit “lows” soon enough. Whether that’s by drugs, sex, or just dopaminergic habits like social media overuse.
Dr. Lembke’s own poison of choice was trashy romance novels, by the way. But she soon found she needed more, and more, and the same level wasn’t “doing it” for her anymore.
So, should we just give up our pleasures, and do a “dopamine fast”?
Not so fast!
It depends on what they are. Dopamine fasting, per se, does not work. We wrote about this previously:
Short On Dopamine? Science Has The Answer
However, when it comes to our dopaminergic habits, a short period (say, a couple of weeks) of absence of that particular thing can help us re-find our balance, and also, find insight.
Lest that latter sound wishy-washy: this is about realizing how bad an overuse of some dopaminergic activity had become, the better to appreciate it responsibly, going forwards.
So in other words, if your poison is, as in Dr. Lembke’s case, trashy romance novels, you would abstain from them for a couple of weeks, while continuing to enjoy the other pleasures in life uninterrupted.
Substances that create a dependency are a special case
There’s often a popular differentiation between physical addictions (e.g. alcohol) and behavioral addictions (e.g. video games). And that’s fair; physiologically speaking, those may both involve dopamine responses, but are otherwise quite different.
However, there are some substances that are physical addictions that do not create a physical dependence (e.g. sugar), and there are substances that create a physical dependence without being addictive (e.g. many antidepressants)
See also: Addiction and physical dependence are not the same thing
In the case of anything that has created a physical dependence, Dr. Lembke does not recommend trying to go “cold turkey” on that without medical advice and supervision.
Going on the counterattack
Remember what we said about pleasure and pain being processed in the same part of the brain, and each rising to meet the other?
While this mean that seeking pleasure will bring us pain, the inverse is also true.
Don’t worry, she’s not advising us to take up masochism (unless that’s your thing!). But there are very safe healthy ways that we can tip the scales towards pain, ultimately leading to greater happiness.
Cold showers are an example she cites as particularly meritorious.
As a quick aside, we wrote about the other health benefits of these, too:
A Cold Shower A Day Keeps The Doctor Away?
Further reading
Want to know more? You might like her book:
Dopamine Nation: Finding Balance in the Age of Indulgence
Enjoy!
Share This Post
-
Gut-Healthy Sunset Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So-called for its gut-healthy ingredients, and its flavor profile being from the Maghreb (“Sunset”) region, the western half of the N. African coast.
You will need
- 1 can chickpeas (do not drain)
- 1 cup low-sodium vegetable stock
- 1 small onion, finely chopped
- 1 carrot, finely chopped
- 2 tbsp sauerkraut, drained and chopped (yes, it is already chopped, but we want it chopped smaller so it can disperse evenly in the soup)
- 2 tbsp tomato paste
- 1 tbsp harissa paste (adjust per your heat preference)
- 1 tbsp ras el-hanout
- ¼ bulb garlic, crushed
- Juice of ½ lemon
- ¼ tsp MSG or ½ tsp low-sodium salt
- Extra virgin olive oil
- Optional: herb garnish; we recommend cilantro or flat-leaf parsley
Method
(we suggest you read everything at least once before doing anything)
1) Heat a little oil in a sauté pan or similar (something suitable for combination cooking, as we’ll be frying first and then adding liquids), and fry the onion and carrot until the onion is soft and translucent; about 5 minutes.
2) Stir in the garlic, tomato paste, harissa paste, and ras el-hanout, and fry for a further 1 minute.
3) Add the remaining ingredients* except the lemon juice. Bring to the boil and then simmer for 5 minutes.
*So yes, this includes adding the “chickpea water” also called “aquafaba”; it adds flavor and also gut-healthy fiber in the form of oligosaccharides and resistant starches, which your gut microbiota can use to make short-chain fatty acids, which improve immune function and benefit the health in more ways than we can reasonably mention as a by-the-way in a recipe.
4) Stir in the lemon juice, and serve, adding a herb garnish if you wish.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Our Top 5 Spices: How Much Is Enough For Benefits? ← today’s recipe scored 5/5 of these, plus quite a few more! Remember that ras el-hanout is a spice blend, so if you’re thinking “wait, where’s the…?” then it’s in the ras el-hanout 😉
- Making Friends With Your Gut (You Can Thank Us Later)
- Lycopene’s Benefits For The Gut, Heart, Brain, & More ← not to be underestimated!
Take care!
Share This Post
-
What’s the difference between physical and chemical sunscreens? And which one should you choose?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sun exposure can accelerate ageing, cause skin burns, erythema (a skin reaction), skin cancer, melasmas (or sun spots) and other forms of hyperpigmentation – all triggered by solar ultraviolet radiation.
Approximately 80% of skin cancer cases in people engaged in outdoor activities are preventable by decreasing sun exposure. This can be done in lots of ways including wearing protective clothing or sunscreens.
But not all sunscreens work in the same way. You might have heard of “physical” and “chemical” sunscreens. What’s the difference and which one is right for you?
How sunscreens are classified
Sunscreens are grouped by their use of active inorganic and organic ultraviolet (UV) filters. Chemical sunscreens use organic filters such as cinnamates (chemically related to cinnamon oil) and benzophenones. Physical sunscreens (sometimes called mineral sunscreens) use inorganic filters such as titanium and zinc oxide.
These filters prevent the effects of UV radiation on the skin.
Organic UV filters are known as chemical filters because the molecules in them change to stop UV radiation reaching the skin. Inorganic UV filters are known as physical filters, because they work through physical means, such as blocking, scattering and reflection of UV radiation to prevent skin damage.
Nano versus micro
The effectiveness of the filters in physical sunscreen depends on factors including the size of the particle, how it’s mixed into the cream or lotion, the amount used and the refraction index (the speed light travels through a substance) of each filter.
When the particle size in physical sunscreens is large, it causes the light to be scattered and reflected more. That means physical sunscreens can be more obvious on the skin, which can reduce their cosmetic appeal.
Nanoparticulate forms of physical sunscreens (with tiny particles smaller than 100 nanometers) can improve the cosmetic appearance of creams on the skin and UV protection, because the particles in this size range absorb more radiation than they reflect. These are sometimes labelled as “invisible” zinc or mineral formulations and are considered safe.
So how do chemical sunscreens work?
Chemical UV filters work by absorbing high-energy UV rays. This leads to the filter molecules interacting with sunlight and changing chemically.
When molecules return to their ground (or lower energy) state, they release energy as heat, distributed all over the skin. This may lead to uncomfortable reactions for people with skin sensitivity.
Generally, UV filters are meant to stay on the epidermis (the first skin layer) surface to protect it from UV radiation. When they enter into the dermis (the connective tissue layer) and bloodstream, this can lead to skin sensitivity and increase the risk of toxicity. The safety profile of chemical UV filters may depend on whether their small molecular size allows them to penetrate the skin.
Chemical sunscreens, compared to physical ones, cause more adverse reactions in the skin because of chemical changes in their molecules. In addition, some chemical filters, such as dibenzoylmethane tend to break down after UV exposure. These degraded products can no longer protect the skin against UV and, if they penetrate the skin, can cause cell damage.
Due to their stability – that is, how well they retain product integrity and effectiveness when exposed to sunlight – physical sunscreens may be more suitable for children and people with skin allergies.
Although sunscreen filter ingredients can rarely cause true allergic dermatitis, patients with photodermatoses (where the skin reacts to light) and eczema have higher risk and should take care and seek advice.
What to look for
The best way to check if you’ll have a reaction to a physical or chemical sunscreen is to patch test it on a small area of skin.
And the best sunscreen to choose is one that provides broad-spectrum protection, is water and sweat-resistant, has a high sun protection factor (SPF), is easy to apply and has a low allergy risk.
Health authorities recommend sunscreen to prevent sun damage and cancer. Chemical sunscreens have the potential to penetrate the skin and may cause irritation for some people. Physical sunscreens are considered safe and effective and nanoparticulate formulations can increase their appeal and ease of use.
Yousuf Mohammed, Dermatology researcher, The University of Queensland and Khanh Phan, Postdoctoral research associate, Frazer Institute, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
The Wim Hof Method – by Wim Hof
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In Wednesday’s main feature, we wrote about the Wim Hof Method, and/but only scratched the surface. Such is the downside of being a super-condensed newsletter! However, it does give us the opportunity to feature the book:
The Wim Hof Method is definitely loudly trumpeted as “up there” with Atomic Habits or How Not To Die in the category of “life-changing” books. Why?
Firstly, it’s a very motivational book. Hof is a big proponent of the notion “if you think you can or you think you can’t, you’re right” idea, practises what he preaches, and makes clear he’s not special.
Secondly, it’s backed up with science. While it’s not a science-heavy book and that’s not the main focus, there are references to studies. Where physiological explanations are given for how certain things work, those explanations are sound. There’s no pseudoscience here, which is especially important for a book of this genre!
What does the book have that our article didn’t? A good few things:
- More about Hof’s own background and where it’s taken him. This is generally not a reason people buy books (unless they are biographies), but it’s interesting nonetheless.
- A lot more advice, data, and information about Cold Therapy and how it can (and, he argues convincingly, should) be built into your life.
- A lot about breathing exercises that we just didn’t cover at all in our article, but is actually an important part of the Wim Hof Method.
- More about stepping through the psychological barriers that can hold us back.
Bottom line: this book offers benefits that stretch into many areas of life, from some simple habits that can be built.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Bare-Bones Truth About Osteoporosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
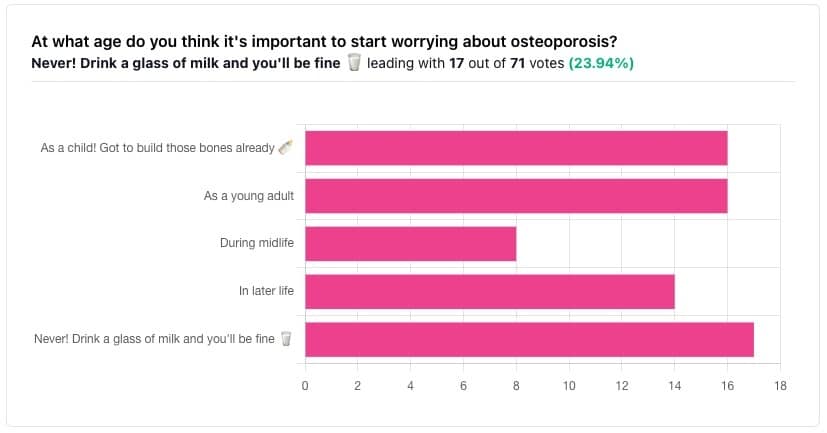
In yesterday’s issue of 10almonds, we asked you “at what age do you think it’s important to start worrying about osteoporosis?”, and here’s the spread of answers you gave us:
The Bare-bones Truth About Osteoporosis
In yesterday’s issue of 10almonds, we asked you “at what age do you think it’s important to start worrying about osteoporosis?”, and here’s the spread of answers you gave us:
At first glance it may seem shocking that a majority of respondents to a poll in a health-focused newsletter think it’ll never be an issue worth worrying about, but in fact this is partly a statistical quirk, because the vote of the strongest “early prevention” crowd was divided between “as a child” and “as a young adult”.
This poll also gave you the option to add a comment with your vote. Many subscribers chose to do so, explaining your choices… But, interestingly, not one single person who voted for “never” had any additional thoughts to add.
We loved reading your replies, by the way, and wish we had room to include them here, because they were very interesting and thought-provoking.
Let’s get to the myths and facts:
Top myth: “you will never need to worry about it; drink a glass of milk and you’ll be fine!”
The body is constantly repairing itself. Its ability to do that declines with age. Until about 35 on average, we can replace bone mineral as quickly as it is lost. After that, we lose it by up to 1% per year, and that rate climbs after 50, and climbs even more steeply for those who go through (untreated) menopause.
Losing 1% per year might not seem like a lot, but if you want to live to 100, there are some unfortunate implications!
About that menopause, by the way… Because declining estrogen levels late in life contribute significantly to osteoporosis, hormone replacement therapy (HRT) may be of value to many for the sake of bone health, never mind the more obvious and commonly-sought benefits.
On the topic of that glass of milk…
- Milk is a great source of calcium, which is useless to the body if you don’t also have good levels of vitamin D and magnesium.
- People’s vitamin D levels tend to directly correlate to the level of sun where they live, if supplementation isn’t undertaken.
- Plant-based milks are usually fortified with vitamin D (and calcium), by the way.
- Most people are deficient in magnesium, because green leafy things don’t form as big a part of most people’s diets as they should.
See also: An update on magnesium and bone health
Next most common myth: “bone health is all about calcium”
We spoke a little above about the importance of vitamin D and magnesium for being able to properly use that. But potassium is also critical:
Read more: The effects of potassium on bone health
While we’re on the topic…
People think of collagen as being for skin health. And it is important for that, but collagen’s benefits (and the negative effects of its absence) go much deeper, to include bone health. We’ve written about this before, so rather than take more space today, we’ll just drop the link:
We Are Such Stuff As Fish Are Made Of
Want to really maximize your bone health?
You might want to check out this well-sourced LiveStrong article:
Bone Health: Best and Worst Foods
(Teaser: leafy greens are in 2nd place, topped by sardines at #1—where do you think milk ranks?)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eggplant vs Zucchini – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing eggplant to zucchini, we picked the zucchini.
Why?
In terms of macros, eggplant has more carbs and fiber while zucchini has more protein; we’ll generally prioritize fiber, so call this a subjective win for eggplant in this category, though an argument could be made for a tie.
In the category of vitamins, eggplant has more of vitamins B3, B5, and E, while zucchini has more of vitamins A, B1, B2, B6, B9, C, K, and choline, scoring a win for zucchini here.
Looking at minerals, eggplant has more copper, manganese, and selenium, while zucchini has more calcium, iron, magnesium, phosphorus, potassium and zinc, meaning another win for zucchini in this round.
In terms of polyphenols, eggplant has a greater variety of polyphenols, while zucchini has greater total mass of polyphenols, so we’re calling this one a tie.
Adding up the sections makes for an overall win for zucchini, but by all means enjoy either or both (perhaps together!); diversity is good!
Want to learn more?
You might like:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: