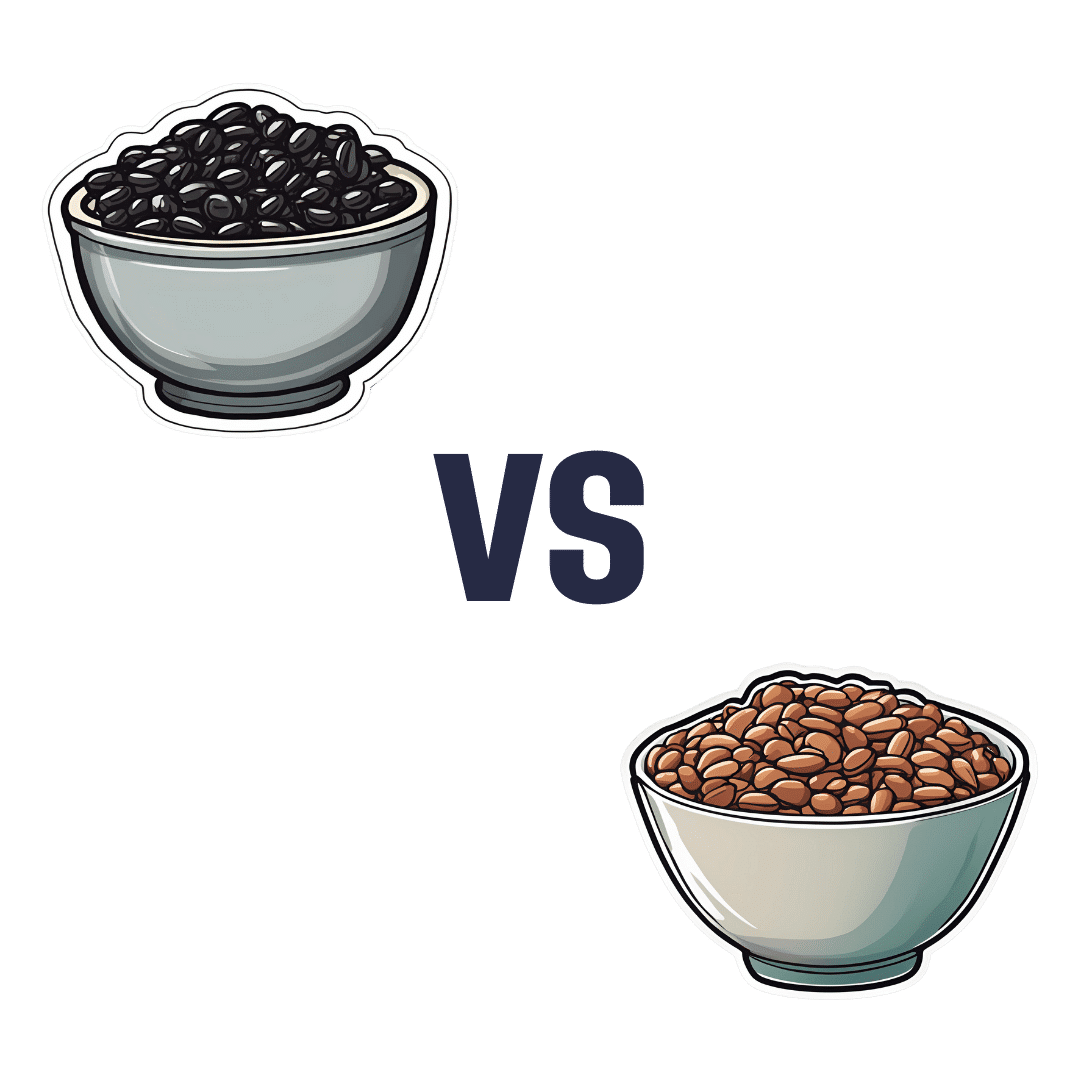
Black Beans vs Pinto Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing black beans to pinto beans, we picked the pinto beans.
Why?
Both of these beans have won all their previous comparisons, so it’s no surprise that this one was very close. Despite their different appearance, taste, and texture, their nutritional profiles are almost identical:
In terms of macros, pinto beans have a tiny bit more protein, carbs, and fiber. So, a nominal win for pinto beans, but again, the difference is very slight.
When it comes to vitamins, black beans have more of vitamins A, B1, B3, and B5, while pinto beans have more of vitamins B2, B6, B9, C, E, K and choline. Superficially, again this is nominally a win for pinto beans, but in most cases the differences are so slight as to be potentially the product of decimal place rounding.
In the category of minerals, black beans have more calcium, copper, iron, and phosphorus, while pinto beans have more magnesium, manganese, selenium, and zinc. That’s a 4:4 tie, but the only one with a meaningful margin of difference is selenium (of which pinto beans have 4x more), so we’re calling this one a very modest win for pinto beans.
All in all, adding these up makes for a “if we really are pressed to choose” win for pinto beans, but honestly, enjoy either in accordance with your preference (this writer prefers black beans!), or better yet, both.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
It’s Not Hysteria – by Dr. Karen Tan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, who this book is aimed at: in case it wasn’t clear, this book assumes you have, or at least have had, a uterus. If that’s not you, then well, it’ll still be an interesting read but it won’t be about your reproductive health.
Secondly, about that “reproductive health”: it’s mostly not actually about reproductive health literally, but rather, the health of one’s reproductive organs and the things that they affect—which is a lot more than the ability to reproduce!
Dr. Tang takes us on a (respectably in-depth) tour of the relevant anatomy, before moving on to physiology, before continuing to pathology (i.e. things that can go wrong, and often do), and finally various treatment options, including elective procedures, and the pros and cons thereof.
She also talks the reader through talking about things with gynecologists and other healthcare providers, and making sure concerns are not dismissed out-of-hand (something that happens a lot, of course).
The style throughout is quite detailed prose, but without being difficult at all to read, and (assuming one is interested in the topic) it’s very engaging.
Bottom line: if you would like to know more about uteri and everything that is (or commonly/unfortunately) can be attached to them, the effects they have on the rest of the body and health, and what can be done about things not being quite right, then this is a good book for that.
Click here to check out It’s Not Hysteria, and understand more of what’s going on down there!
Share This Post
-
Infections, Heart Failure, & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Some health news to round off the week:
The Infection That Leads To Heart Failure
It’s long been held that, for example, flossing reduces heart disease risk, with the hypothesis being that if plaque bacteria enter the blood stream, well, that’s an even worse place for plaque bacteria to be. Now, with much more data, attention has turned to
- actual infections, and
- actual heart failure
Way to up the ante! And, it holds true regardless of what kind of infection. So, you might think that a UTI, for example, is surely “downstream” and should not affect the heart, but it does. Because of this, researchers currently believe that it is not the infection itself, so much as the body’s inflammation response to infection, that leads to the heart failure. Which is reasonable, because, for example, atherosclerosis is made mostly not of cholesterol itself, but rather mostly of dead immune cells that got stuck in the cholesterol.
Moreover, it’s not so much about the acute inflammatory response (which is almost always a good thing, circumstantially), but rather that after cases where an infection managed to take hold, the immune system can then often stay on high alert for many years alter. Long COVID is an obvious recent example of this, but it’s hardly a new phenomenon; see for example post-polio syndrome, and consider how many more such post-infection maladies are likely to exist that never got a name because they flew under the radar or got diagnosed as fibromyalgia or something (fibromyalgia is a common diagnosis doctors give when they acknowledge something’s wrong, and it causes pain and exhaustion, but they don’t know what, and it appears to be stable—so while it can be helpful to put a name to the collection of symptoms, it’s a non-diagnosis diagnosis on the doctors’ part. It’s saying “I diagnose you with hurty tiredness”).
The take-away from all this? Avoid infections, for your heart’s sake, and if you do get an infection, take it seriously even if it’s minor. The safe amount of infection is “no infection”.
Read in full: Study uncovers new link between infections and heart failure
Cold Water Immersion: Hot Or Not?
The evidence is clear for some benefits; for others, not so much:
- It’s great (if you’re already in fair health, and definitely not if you have a heart condition) to improve circulation and stress response
- There may be some benefits to immune function, but however reasonable the hypothesis, actual evidence is thin on the ground
- The oft-hyped mood benefits are a) marginal b) short-lived, with benefits fading after 3 months of regular cold baths/showers/etc
Read in full: The big chill: Is cold-water immersion good for our health?
Related: Ice Baths: To Dip Or Not To Dip?
The Unspoken Trials Of Going To The Gym (While Being A Woman)
Public health decision-makers often think that getting people to go to the gym more is a matter of public information, or perhaps branding. Some who have their thinking heads on might even realize that there may be economic factors for many. But for women, there’s an additional factor—or rather, an additionally prominent factor. The study we’ll link started with this observation (please read it in the voice of your favorite nature documentary narrator):
❝Despite an increase in gym memberships, women are less active than men and little is known about the barriers women face when navigating gym spaces.❞
What then, of these shy, elusive creatures that make up a mere 51% of the world’s population?
A medium-sized (n=279) study of women, of whom 84% being current gym-goers, reported often feeling “judged for their appearance or performance, as well as having to fight for space in the gym and to be taken seriously, while navigating harassment and unsolicited comments from men”
Even gym attire becomes an issue:
❝Aligning with previous literature, women often chose attire based on comfort and functionality. However, their choices were also influenced by comparisons with others or fear of judgement for wearing non-branded attire or looking too put together. Many women also chose gym attire to hide perceived problem areas or avoid appearance concerns, including visible sweat stains.❞
…which main seem silly; you’re at the gym, of course you’re going to sweat, but if you’re the only one with visible sweat stains, then there can be social consequences (bad ones).
Similarly, there’s a “damned if you do; damned if you don’t” when it comes to working out while fat—on the one hand, society conflates fatness with laziness; on the other, it can be extra intimidating to be the only fat person in a gym full of people who look like they’re going to audition for a superhero movie.
❝In the gym, just like in other areas of life, women often feel stuck between being seen as ‘too much’ and ‘not enough’, dealing with judgement about how they look, how they perform, and even how much space they take up. Even though the pressure to be super thin is decreasing, the growing focus on being muscular and athletic is creating new challenges. It is pushing unrealistic standards that can negatively affect women’s body image and overall well-being.❞
Writer’s note: I live a few minutes walk from my nearest gym, and I work out at home instead. This way, if I want to do yoga in my pajamas, I can. If I want to use my treadmill naked and watch my T+A bounce in the mirror, I can. If I want to lift weights in the dress I happened to be wearing, I can. Alas that I can’t swim at home!
Read in full: Women face multiple barriers while exercising in gyms
Related: Body Image Dissatisfaction/Appreciation Across The Ages
Take care!
Share This Post
-
Broad Beans vs Sweetcorn – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing broad beans to sweetcorn, we picked the broad beans.
Why?
Firstly, you may be wondering: “aren’t broad beans fava beans?”, and yes, yes they are, but by convention, broad beans are the young green beans, while fava beans are the mature beans of the plant. Similar situation to the relationship between edamame and soybeans. And, in both cases, you’re more likely to put the young green beans in a salad, thus making the broad beans the more reasonable vegetable to compare to the sweetcorn. On which note…
In terms of macros, the broad beans have more protein and fiber, while the sweetcorn has more carbs. We call that a win for the beans.
Looking at the vitamins, the broad beans have (barely) more vitamin B6, while the sweetcorn has more of vitamins A, B1, B2, B5, B9, E, and choline. An easy win for the corn this time.
In the category of minerals, the situation is reversed: broad beans have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while sweetcorn is not higher in any minerals. So, a clear win for the beans.
Adding up the sections gives a 2:1 win for the beans over the corn, but by all means enjoy either or both—together is great, and diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Share This Post
Related Posts
-
Our Top 5 Spices: How Much Is Enough For Benefits?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A spoonful of pepper makes the… Hang on, no, that’s not right…
We know that spices are the spice of life, and many have great health-giving qualities. But…
- How much is the right amount?
- What’s the minimum to get health benefits?
- What’s the maximum to avoid toxicity?
That last one always seems like a scary question, but please bear in mind: everything is toxic at a certain dose. Oxygen, water, you-name-it.
On the other hand, many things have a toxicity so low that one could not physically consume it sufficiently faster than the body eliminates it, to get a toxic build-up.
Consider, for example, the €50 banknote that was nearly withdrawn from circulation because one of the dyes used in it was found to be toxic. However, the note remained in circulation after scientists patiently explained that a person would have to eat many thousands of them to get a lethal dose.
So, let’s address these questions in reverse order:
What’s the maximum to avoid toxicity?
In the case of the spices we’ll look at today, the human body generally* has high tolerance for them if eaten at levels that we find comfortable eating.
*IMPORTANT NOTE: If you have (or may have) a medical condition that may be triggered by spices, go easier on them (or if appropriate, abstain completely) after you learn about that.
Check with your own physician if unsure, because not only are we not doctors, we’re specifically not your doctors, and cannot offer personalized health advice.
We’re going to be talking in averages and generalizations here. Caveat consumator.
For most people, unless you are taking the spice in such quantities that you are folding space and seeing the future, or eating them as the main constituents of your meal rather than an embellishment, you should be fine. Please don’t enter a chilli-eating contest and sue us.
What is the minimum to get health benefits and how much should we eat?
The science of physiology generally involves continuous rather than discrete data, so there’s not so much a hard threshold, as a point at which the benefits become significant. The usefulness of most nutrients we consume, be they macro- or micro-, will tend to have a bell curve.
In other words, a tiny amount won’t do much, the right amount will have a good result, and usefulness will tail off after that point. To that end, we’re going to look at the “sweet spot” of peaking on the graph.
Also note: the clinical dose is the dose of the compound, not the amount of the food that one will need to eat to get that dose. For example, food x containing compound y will not usually contain that compound at 100% rate and nothing else. We mention this so that you’re not surprised when we say “the recommended dose is 5mg of compound, so take a teaspoon of this spice”, for example.
Further note: we only have so much room here, so we’re going to list only the top benefits, and not delve into the science of them. You can see the related main features for more details, though!
The “big 5” health-giving spices, with their relevant active compound:
- Black pepper (piperine)
- Hot pepper* (capsaicin)
- Garlic (allicin)
- Ginger (gingerol)
- Turmeric (curcumin**)
*Cayenne pepper is very high in capsaicin; chilli peppers are also great
**not the same thing as cumin, which is a completely different plant. Cumin does have some health benefits of its own, but not in the same league as the spices above, and there’s only so much we have room to cover today.
Black pepper
- Benefits: antioxidant, anti-cancer, boosts bioavailability of other nutrients, aids digestion
- Dosage: 5–20mg for benefits
- Suggestion: ½ teaspoon of black pepper is sufficient for benefits. However, this writer’s kitchen dictum in this case is “if you can’t see the black pepper in/on the food, add more”—but that’s more about taste!
- Related main feature: Black Pepper’s Anti-Cancer Arsenal (And More)
Hot Pepper
- Benefits: anti-inflammatory, metabolism accelerator
- Dosage: 6mg gives benefits, 500mg is a common dose in capsules
- Suggestion: if not making a spicy dish, consider using a teaspoon of cayenne as part of the seasoning for rice or potatoes
- Related main feature: Capsaicin For Weight Loss And Against Inflammation
Garlic
- Benefits: heart health, blood sugar balancing, anti-cancer
- Dosage: 4–8µg for benefits
- Suggestion: 1–2 cloves daily is generally good. However, cooking reduces allicin content (and so does oxidation after cutting/crushing), so you may want to adjust accordingly if doing those things.
- Related main feature: The Many Health Benefits Of Garlic
Ginger
- Benefits: anti-inflammatory, antioxidant, anti-nausea
- Dosage: 3–4g for benefits
- Suggestion: 1 teaspoon grated raw ginger or ½ a teaspoon powdered ginger, can be used in baking or as part of the seasoning for a stir-fry
- Related main feature: Ginger Does A Lot More Than You Think
Turmeric
- Benefits: anti-inflammatory, anti-cancer
- Dosage: 500–2000mg for benefits
- Suggestion: ¼ teaspoon per day is sufficient for benefits; ½ teaspoon dropped into the water when cooking rice will infuse the rice with turmeric (which is very water-soluble), turn the rice a pretty golden color, and not affect the flavor. Throw in some black pepper as it increases the bioavailability of curcumin up to 2000%
- Related main feature: Why Curcumin (Turmeric) Is Worth Its Weight In Gold
Closing notes
The above five spices are very healthful for most people. Personal physiology can and will vary, so if in doubt, a) check with your doctor b) start at lowest doses and establish your tolerance (or lack thereof).
Enjoy, and stay well!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Mediterranean Diet: What Is It Good For?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More to the point: what isn’t it good for?
- It’s been found to reduce all-cause mortality, which is about the best thing one can say of any diet.
- It’s especially good for heart health and against cancer.
- It’s particularly recommended for the prevention or management of diabetes.
- It’s also been found, societally, to reduce general healthcare costs—basically, people get sick less and so have fewer healthcare costs.
What brought it to the attention of the world’s scientific community?
Back in the 1950s, physiologist Ancel Keys wondered why poor people in Italian villages were healthier than wealthy New Yorkers. Upon undertaking studies, he narrowed it down to the Mediterranean diet—something he’d then take on as a public health cause for the rest of his career.
Keys himself lived to the ripe old age of 100, by the way.
When we say “Mediterranean Diet”, what image comes to mind?
We’re willing to bet that tomatoes feature (great source of lycopene, by the way), but what else?
- Salads, perhaps? Vegetables, olives? Olive oil, yea or nay?
- Bread? Pasta? Prosciutto, salami? Cheese?
- Pizza but only if it’s Romana style, not Chicago?
- Pan-seared liver, with some fava beans and a nice Chianti?
In reality, the diet is based on what was historically eaten specifically by Italian peasants. If the word “peasants” conjures an image of medieval paupers in smocks and cowls, and that’s not necessarily wrong, further back historically… but the relevant part here is that they were people who lived and worked in the countryside.
They didn’t have money for meat, which was expensive, nor the industrial setting for refined grain products to be affordable. They didn’t have big monocrops either, which meant no canola oil, for example… Olives produce much more easily extractable oil per plant, so olive oil was easier to get. Nor, of course, did they have the money (or infrastructure) for much in the way of imports.
So what foods are part of “the” Mediterranean Diet?
- Fruits. These would be fruits grown locally, but no need to sweat that, dietwise. It’s hard to go wrong with fruit.
- Tomatoes yes. So many tomatoes. (Knowledge is knowing tomato is a fruit. Wisdom is not putting it in a fruit salad)
- Non-starchy vegetables (e.g. eggplant yes, potatoes no)
- Greens (spinach, kale, lettuce, all those sorts of things)
- Beans and other legumes (whatever was grown nearby)
- Whole grain products in moderation (wholegrain bread, wholewheat pasta)
- Olives and olive oil. Special category, single largest source of fat in the Mediterranean diet, but don’t overdo it.
- Dairy products in moderation (usually hard cheeses, as these keep well)
- Fish, in moderation. Typically grilled, baked, steamed even. Not fried.
- Other meats as a rarer luxury in considerable moderation. There’s more than one reason prosciutto is so thinly sliced!
Want to super-power this already super diet?
Try: A Pesco-Mediterranean Diet With Intermittent Fasting: JACC Review Topic of the Week
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Huperzine A: A Natural Nootropic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Huperzine A: A Natural Nootropic
Huperzine A is a compound, specifically a naturally occurring sesquiterpene alkaloid, that functions as an acetylcholinesterase inhibitor. If that seems like a bunch of big words, don’t worry, we’ll translate in a moment.
First, a nod to its origins: it is found in certain kinds of firmoss, especially the “toothed clubmoss”, Huperzia serrata, which grows in many Asian countries.
What’s an acetylcholinesterase inhibitor?
Let’s do this step-by-step:
- An acetylcholinesterase inhibitor is a compound that inhibits acetylcholinesterase.
- Acetylcholinesterase is an enzyme that catalyzes (speeds up) the breakdown of acetylcholine.
- Acetylcholine is a neurotransmitter; it’s an ester of acetic acid and choline.
- This is the main neurotransmitter of the parasympathetic nervous system, and is also heavily involved in cognitive functions including memory and creative thinking.
What this means: if you take an acetylcholinesterase inhibitor like huperzine A, it will inhibit acetylcholinesterase, meaning you will have more acetylcholine to work with. That’s good.
What can I expect from it?
Huperzine A has been well-studied for a while, mostly for the prevention and treatment of Alzheimer’s disease:
- New insights into huperzine A for the treatment of Alzheimer’s disease
- Huperzine A: Is it an Effective Disease-Modifying Drug for Alzheimer’s Disease?
- Huperzine A and Its Neuroprotective Molecular Signaling in Alzheimer’s Disease
However, research has suggested that huperzine A is much better as a prevention than a treatment:
❝A central event in the pathogenesis of Alzheimer’s disease (AD) is the accumulation of senile plaques composed of aggregated amyloid-β (Aβ) peptides.
Ex vivo electrophysiological experiments showed that 10 μM of Aβ1-40 significantly decreased the effect of the AChE inhibitor huperzine A on the synaptic potential parameters. ❞
~ Dr. Irina Zueva
In other words: the answer to the titular question is “Yes, yes it can”
And, to translate Dr. Zueva’s words into simple English:
- People with Alzheimer’s have amyloid-β plaque in their brains
- That plaque reduces the effectiveness of huperzine A
So, what if we take it in advance? That works much better:
❝Pre-treatment with [huperzine A] at concentrations of 50, 100, and 150 µg/mL completely inhibited the secretion of PGE2, TNF-α, IL-6, and IL-1β compared to post-treatment with [huperzine A].
This suggests that prophylactic treatment is better than post-inflammation treatment. ❞
~ Dr. Thu Kim Dang
Source: Anti-neuroinflammatory effects of alkaloid-enriched extract from Huperzia serrata
As you may know, neuroinflammation is a big part of Alzheimer’s pathology, so we want to keep that down. The above research suggests we should do that sooner rather than later.
Aside from holding off dementia, can it improve memory now, too?
There’s been a lot less research done into this (medicine is generally more concerned with preventing/treating disease, than improving the health of healthy people), but there is some:
^This is a small (n=68) old (1999) study for which the full paper has mysteriously disappeared and we only get to see the abstract. It gave favorable results, though.
The effects of huperzine A and IDRA 21 on visual recognition memory in young macaques
^This, like most non-dementia research into HupA, is an animal study. But we chose to spotlight this one because, unlike most of the studies, it did not chemically lobotomize the animals first; they were and remained healthy. That said, huperzine A improved the memory scores most for the monkeys that performed worst without it initially.
Where can I get it?
As ever, we don’t sell it, but here’s an example product on Amazon for your convenience
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: