Why Fibromyalgia Is Not An Acceptable Diagnosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Efrat Lamandre makes the case that fibromyalgia is less of a useful diagnosis and more of a rubber stamp, much like the role historically often fulfilled by “heart failure” as an official cause of death (because certainly, that heart sure did stop beating). It’s a way of answering the question without answering the question.
…and what to look for instead
Fibromyalgia is characterized by chronic pain, tenderness, sleep disturbances, fatigue, and other symptoms. It’s often considered an “invisible” illness, because it’s the kind that’s easy to dismiss if you’re not the one carrying it. A broken leg, one can point at and see it’s broken; a respiratory infection, one can see its effects and even test for presence of the pathogen and/or its antigens. But fibromyalgia? “It hurts and I’m tired” doesn’t quite cut it.
Much like “heart failure” as a cause of death when nothing else is implicated, fibromyalgia is a diagnosis that gets applied when known causes of chronic pain have been ruled out.
Dr. Lamandre advocates for functional medicine and seeking the underlying causes of the symptoms, rather than the industry standard approach, which is to just manage the symptoms themselves with medications (of course, managing the symptoms with medications has its place; there is no need to suffer needlessly if pain relief can be used; it’s just not a sufficient response).
She notes that potential triggers for fibromyalgia include microbiome imbalances, food sensitivities, thyroid issues, nutrient deficiencies, adrenal fatigue, mitochondrial dysfunction, mold toxicity, Lyme disease, and more. Is this really just one illness? Maybe, but quite possibly not.
In short… If you are given a diagnosis of fibromyalgia, she advises that you insist doctors keep on looking, because that’s not an answer.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Managing Chronic Pain (Realistically!)
- How To Eat To Beat Chronic Fatigue ← yes, including how to do so when you are chronically fatigued. In other words, this isn’t just dietary advice, but rather practical advice too
- When Painkillers Aren’t Helping, These Things Might
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Reduce Caffeine’s Impact on Kidneys
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Avid coffee drinker so very interested in the results Also question Is there something that you could take or eat that would prevent the caffeine from stimulating the kidneys? I tried to drink decaf from morning to night not a good result! Thanks❞
That is a good question! The simple answer is “no” (but keep reading, because all is not lost)
There’s no way (that we yet know of) to proof the kidneys against the stimulating effect of caffeine. This is especially relevant because part of caffeine’s stimulating effect is noradrenergic, and that “ren” in the middle there? It’s about the kidneys. This is just because the adrenal gland is situated next to them (actually, it’s pretty much sitting on top of them), hence the name, but it does mean that the kidneys are about the hardest thing in the body to have not effected by caffeine.
However! The effects of caffeine in general can be softened a little with l-theanine (found in tea, or it can be taken as a supplement). It doesn’t stop it from working, but it makes the curve of the effect a little gentler, and so it can reduce some unwanted side effects.
You can read more about l-theanine here:
Share This Post
-
Protein: How Much Do We Need, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mythbusting Protein!
Yesterday, we asked you for your policy on protein consumption. The distribution of responses was as follows:
- A marginal majority (about 55%) voted for “Protein is very important, but we can eat too much of it”
- A large minority (about 35%) voted for “We need lots of protein; the more, the better!”
- A handful (about 4%) voted for “We should go as light on protein as possible”
- A handful (6%) voted for “If we don’t eat protein, our body will create it from other foods”
So, what does the science say?
If we don’t eat protein, our body will create it from other foods: True or False?
Contingently True on an absurd technicality, but for all practical purposes False.
Our body requires 20 amino acids (the building blocks of protein), 9 of which it can’t synthesize and absolutely must get from food. Normally, we get those amino acids from protein in our diet, and we can also supplement them by buying amino acid supplements.
Specifically, we require (per kg of bodyweight) a daily average of:
- Histidine: 10 mg
- Isoleucine: 20 mg
- Leucine: 39 mg
- Lysine: 30 mg
- Methionine: 10.4 mg
- Phenylalanine*: 25 mg
- Threonine: 15 mg
- Tryptophan: 4 mg
- Valine: 26 mg
*combined with the non-essential amino acid tyrosine
Source: Protein and Amino Acid Requirements In Human Nutrition: WHO Technical Report
However, to get the requisite amino acid amounts, without consuming actual protein, would require gargantuan amounts of supplementation (bearing in mind bioavailability will never be 100%, so you’ll always need to take more than it seems), using supplements that will have been made by breaking down proteins anyway.
So unless you live in a laboratory and have access to endless amounts of all of the required amino acids (you can’t miss even one; you will die), and are willing to do that for the sake of proving a point, then you do really need to eat protein.
Your body cannot, for example, simply break down sugar and use it to make the protein you need.
On another technical note… Do bear in mind that many foods that we don’t necessarily think of as being sources of protein, are sources of protein.
Grains and grain products, for example, all contain protein; we just don’t think of them as that because their macronutritional profile is heavily weighted towards carbohydrates.
For that matter, even celery contains protein. How much, you may ask? Almost none! But if something has DNA, it has protein. Which means all plants and animals (at least in their unrefined forms).
So again, to even try to live without protein would very much require living in a laboratory.
We can eat too much protein: True or False?
True. First on an easy technicality; anything in excess is toxic. Even water, or oxygen. But also, in practical terms, there is such a thing as too much protein. The bar is quite high, though:
❝Based on short-term nitrogen balance studies, the Recommended Dietary Allowance of protein for a healthy adult with minimal physical activity is currently 0.8 g protein per kg bodyweight per day❞
❝To meet the functional needs such as promoting skeletal-muscle protein accretion and physical strength, dietary intake of 1.0, 1.3, and 1.6 g protein per kg bodyweight per day is recommended for individuals with minimal, moderate, and intense physical activity, respectively❞
❝Long-term consumption of protein at 2 g per kg bodyweight per day is safe for healthy adults, and the tolerable upper limit is 3.5 g per kg bodyweight per day for well-adapted subjects❞
❝Chronic high protein intake (>2 g per kg bodyweight per day for adults) may result in digestive, renal, and vascular abnormalities and should be avoided❞
Source: Dietary protein intake and human health
To put this into perspective, if you weigh about 160lbs (about 72kg), this would mean eating more than 144g protein per day, which grabbing a calculator means about 560g of lean beef, or 20oz, or 1¼lb.
If you’re eating quarter-pounder burgers though, that’s not usually so lean, so you’d need to eat more than nine quarter-pounder burgers per day to get too much protein.
High protein intake damages the kidneys: True or False?
True if you have kidney damage already; False if you are healthy. See for example:
- Effects of dietary protein restriction on the progression of advanced renal disease in the modification of diet in renal disease study
- A high protein diet has no harmful effects: a one-year crossover study in healthy male athletes
High protein intake increases cancer risk: True or False?
True or False depending on the source of the protein, so functionally false:
- Eating protein from red meat sources has been associated with higher risk for many cancers
- Eating protein from other sources has been associated with lower risk for many cancers
Source: Red Meat Consumption and Mortality Results From 2 Prospective Cohort Studies
High protein intake increase risk of heart disease: True or False?
True or False depending on the source of the protein, so, functionally false:
- Eating protein from red meat sources has been associated with higher risk of heart disease
- Eating protein from other sources has been associated with lower risk of heart disease
Source: Major Dietary Protein Sources and Risk of Coronary Heart Disease in Women
In summary…
Getting a good amount of good quality protein is important to health.
One can get too much, but one would have to go to extremes to do so.
The source of protein matters:
- Red meat is associated with many health risks, but that’s not necessarily the protein’s fault.
- Getting plenty of protein from (ideally: unprocessed) sources such as poultry, fish, and/or plants, is critical to good health.
- Consuming “whole proteins” (that contain all 9 amino acids that we can’t synthesize) are best.
Learn more: Complete proteins vs. incomplete proteins (explanation and examples)
Share This Post
-
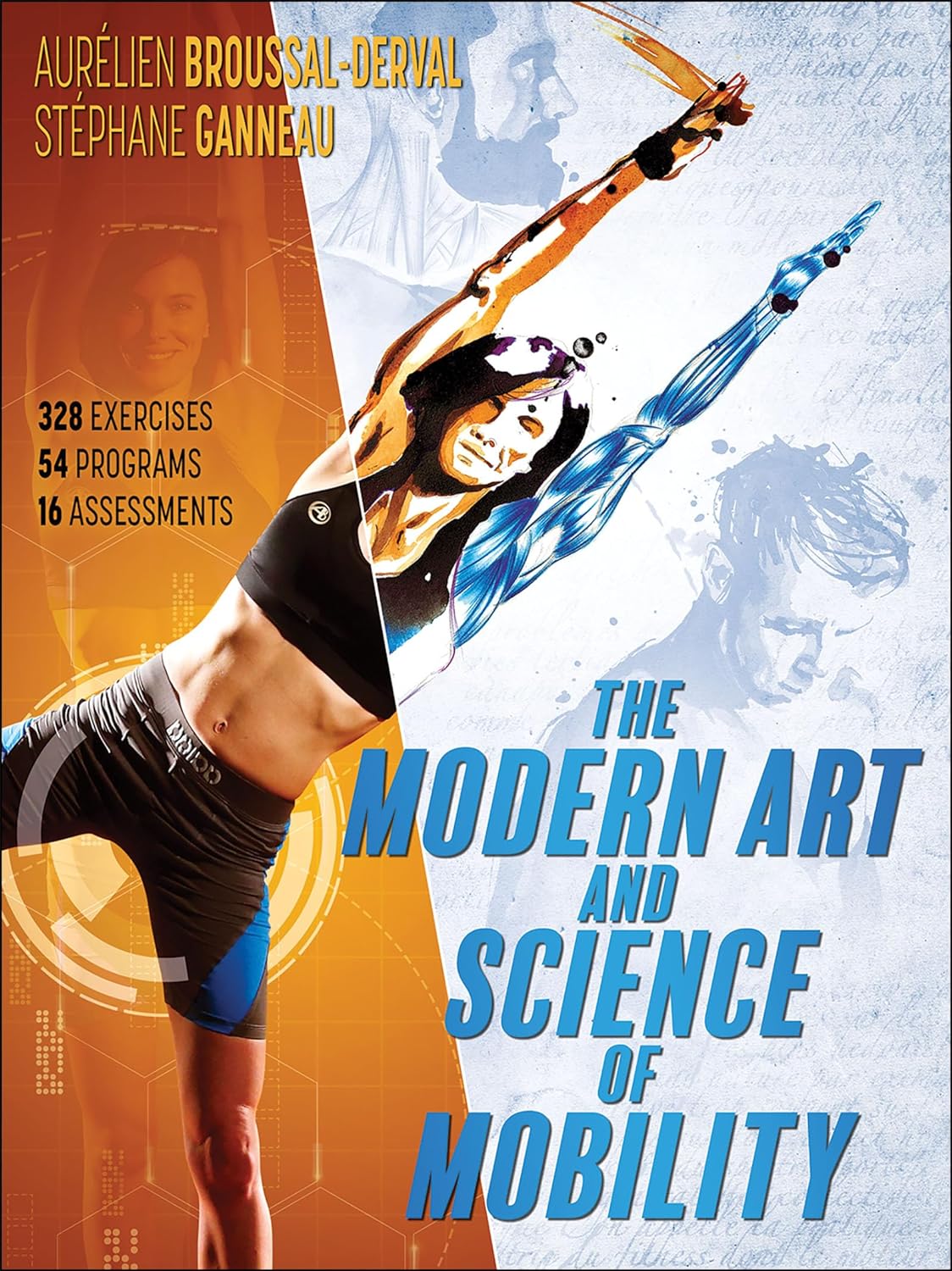
The Modern Art and Science of Mobility – by Aurélien Broussal-Derval
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed mobility books before, so what makes this one stand out?
We’ll be honest: the illustrations are lovely.
The science, the information, the exercises, the routines, the programs… All these things are excellent too, but these can be found in many a book.
What can’t usually be found is very beautiful (yet no less clear) watercolor paintings and charcoal sketches as anatomical illustrations.
There are photos too (also of high quality), but the artistry of the paintings and sketches is what makes the reader want to spend time perusing the books.
At least, that’s what this reviewer found! Because it’s all very well having access to a lot of information (and indeed, I read so much), but making it enjoyable increases the chances of rereading it much more often.
As for the rest of the content, the book’s information is divided in categories:
- Pain (what causes it, what it means, and how to manage it)
- Breathing (yes, a whole section devoted to this, and it is aligned heavily to posture also, as well as psychological state and the effect of stress on tension, inflammation, and more)
- Movement (this is mostly about kinds of movement and ranges of movement)
- Mobility (this is about aggregating movements as a fully mobile human)
So, each builds on from the previous because any pain needs addressing before anything else, breathing (and with it, posture) comes next, then we learn about movement, then we bring it all together for mobility.
Bottom line: this is a beautiful and comprehensive book that will make learning a joy
Click here to check out The Modern Art and Science of Mobility, and learn and thrive!
Share This Post
Related Posts
-
How Tight Are Your Hips? Test (And Fix!) With This
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Upon surveying over half a million people; hips were the most common area for stiffness and lack of mobility. So, what to do about it?
This test don’t lie
With 17 muscles contributing to hip function (“hip flexors” being the name for this group of 17 muscles, not specific muscle), it’s important to figure out which ones are tight, and if indeed it really is the hip flexors at all, or if it could be, as it often is, actually the tensor fasciae latae (TFL) muscle of the thigh. If it turns out to be both, well, that’s unfortunate but the good news is, now you’ll know and can start fixing from all the necessary angles.
Diagnostic test for tight hip flexors (Thomas Test):
- Use a sturdy, elevated surface (e.g. table or counter—not a bed or couch, unless there is perchance room to swing your legs without them touching the floor).
- Sit at the edge, lie back, and pull both knees to your chest.
- Return one leg back down until the thigh is perpendicular to the table.
- Let the other leg dangle off the edge to assess flexibility.
Observations from the test:
- Thigh contact: is the back of your thigh touching the table?
- Knee angle: is your knee bent at roughly 80° or straighter?
- Thigh rotation: does the thigh roll outward?
Interpreting results:
- If your thigh contacts the surface and the knee is bent at around 80°, hip mobility is good.
- If your thigh doesn’t touch or knee is too straight, hip flexor tightness is present.
- If your thigh rolls outwards from your midline, that indicates tightness in the TFL muscle of the thigh.
Three best hip flexor stretches:
- Kneeling lunge stretch:
- Hips above the knee, tuck tailbone, engage glutes, press hips forward, reach arm up with a slight side bend.
- Seated hip lift stretch:
- Sit with feet hip-width apart, hands behind shoulders, lift hips, step one foot back, tuck tailbone, point knee away.
- Sofa stretch:
- Kneel with one shin against a couch/wall, other foot forward in lunge, tuck tailbone, press hips forward, lift torso.
It’s recommended to how each stretch for 30 seconds on each side.
For more on all of the above, and visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Surgery won’t fix my chronic back pain, so what will?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This week’s ABC Four Corners episode Pain Factory highlighted that our health system is failing Australians with chronic pain. Patients are receiving costly, ineffective and risky care instead of effective, low-risk treatments for chronic pain.
The challenge is considering how we might reimagine health-care delivery so the effective and safe treatments for chronic pain are available to millions of Australians who suffer from chronic pain.
One in five Australians aged 45 and over have chronic pain (pain lasting three or more months). This costs an estimated A$139 billion a year, including $12 billion in direct health-care costs.
The most common complaint among people with chronic pain is low back pain. So what treatments do – and don’t – work?
Opioids and invasive procedures
Treatments offered to people with chronic pain include strong pain medicines such as opioids and invasive procedures such as spinal cord stimulators or spinal fusion surgery. Unfortunately, these treatments have little if any benefit and are associated with a risk of significant harm.
Spinal fusion surgery and spinal cord stimulators are also extremely costly procedures, costing tens of thousands of dollars each to the health system as well as incurring costs to the individual.
Addressing the contributors to pain
Recommendations from the latest Australian and World Health Organization clinical guidelines for low back pain focus on alternatives to drug and surgical treatments such as:
- education
- advice
- structured exercise programs
- physical, psychological or multidisciplinary interventions that address the physical or psychological contributors to ongoing pain.
Pain education is central. Monkey Business Images/Shutterstock Two recent Australian trials support these recommendations and have found that interventions that address each person’s physical and psychological contributors to pain produce large and sustained improvements in pain and function in people with chronic low back pain.
The interventions have minimal side effects and are cost-effective.
In the RESOLVE trial, the intervention consists of pain education and graded sensory and movement “retraining” aimed to help people understand that it’s safe to move.
In the RESTORE trial, the intervention (cognitive functional therapy) involves assisting the person to understand the range of physical and psychological contributing factors related to their condition. It guides patients to relearn how to move and to build confidence in their back, without over-protecting it.
Why isn’t everyone with chronic pain getting this care?
While these trials provide new hope for people with chronic low back pain, and effective alternatives to spinal surgery and opioids, a barrier for implementation is the out-of-pocket costs. The interventions take up to 12 sessions, lasting up to 26 weeks. One physiotherapy session can cost $90–$150.
In contrast, Medicare provides rebates for just five allied health visits (such as physiotherapists or exercise physiologists) for eligible patients per year, to be used for all chronic conditions.
Private health insurers also limit access to reimbursement for these services by typically only covering a proportion of the cost and providing a cap on annual benefits. So even those with private health insurance would usually have substantial out-of-pocket costs.
Access to trained clinicians is another barrier. This problem is particularly evident in regional and rural Australia, where access to allied health services, pain specialists and multidisciplinary pain clinics is limited.
Higher costs and lack of access are associated with the increased use of available and subsidised treatments, such as pain medicines, even if they are ineffective and harmful. The rate of opioid use, for example, is higher in regional Australia and in areas of socioeconomic disadvantage than metropolitan centres and affluent areas.
So what can we do about it?
We need to reform Australia’s health system, private and public, to improve access to effective treatments for chronic pain, while removing access to ineffective, costly and high-risk treatments.
Better training of the clinical workforce, and using technology such as telehealth and artificial intelligence to train clinicians or deliver treatment may also improve access to effective treatments. A recent Australian trial, for example, found telehealth delivered via video conferencing was as effective as in-person physiotherapy consultations for improving pain and function in people with chronic knee pain.
Advocacy and improving the public’s understanding of effective treatments for chronic pain may also be helpful. Our hope is that coordinated efforts will promote the uptake of effective treatments and improve the care of patients with chronic pain.
Christine Lin, Professor, University of Sydney; Christopher Maher, Professor, Sydney School of Public Health, University of Sydney; Fiona Blyth, Professor, University of Sydney; James Mcauley, Professor of Psychology, UNSW Sydney, and Mark Hancock, Professor of Physiotherapy, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Breathe; Don’t Vent (At Least In The Moment)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Zen And The Art Of Breaking Things
We’ve talked before about identifying emotions and the importance of being able to express them:
Answering The Most Difficult Question: How Are You?
However, there can be a difference between “expressing how we feel” and “being possessed by how we feel and bulldozing everything in our path”
…which is, of course, primarily a problem in the case of anger—and by extension, emotions that are often contemporaneous with anger, such as jealousy, shame, fear, etc.
How much feeling is too much?
While this is in large part a subjective matter, clinically speaking the key question is generally: is it adversely affecting daily life to the point of being a problem?
For example, if you have to spend half an hour every day actively managing a certain emotion, that’s probably indicative of something unusual, but “unusual” is not inherently bad. If you’re managing it safely and in a way that doesn’t negatively affect the rest of your life, then that is generally considered fine, unless you feel otherwise about it.
A good example of this is complicated grief and/or prolonged grief.
But what about when it comes to anger? How much is ok?
When it comes to those around you, any amount of anger can seem like too much. Anger often makes us short-tempered even with people who are not the object of our anger, and it rarely brings out the best in us.
We can express our feelings in non-aggressive ways, for example:
and
Seriously Useful Communication Skills!
Sometimes, there’s another way though…
Breathe; don’t vent
That’s a great headline, but we can’t take the credit for it, because it came from:
Breathe, don’t vent: turning down the heat is key to managing anger
…in which it was found that, by all available metrics, the popular wisdom of “getting it off your chest” doesn’t necessarily stand up to scrutiny, at least in the short term:
❝The work was inspired in part by the rising popularity of rage rooms that promote smashing things (such as glass, plates and electronics) to work through angry feelings.
I wanted to debunk the whole theory of expressing anger as a way of coping with it,” she said. “We wanted to show that reducing arousal, and actually the physiological aspect of it, is really important.❞
And indeed, he and his team did find that various arousal-increasing activities (such as hitting a punchbag, breaking things, doing vigorous exercise) did not help as much as arousal-decreasing activities, such as mindfulness-based relaxation techniques.
If you’d like to read the full paper, then so would we, but we couldn’t get full access to this one yet. However, the abstract includes representative statistics, so that’s worth a once-over:
Caveat!
Did you notice the small gap between their results and their conclusion?
In a lab or similar short-term observational setting, their recommendation is clearly correct.
However, if the source of your anger is something chronic and persistent, it could well be that calming down without addressing the actual cause is just “kicking the can down the road”, and will still have to actually be dealt with eventually.
So, while “here be science”, it’s not a mandate for necessarily suffering in silence. It’s more about being mindful about how we go about tackling our anger.
As for a primer on mindfulness, feel free to check out:
No-Frills, Evidence-Based Mindfulness
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: