Ginger Does A Lot More Than You Think
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ginger’s benefits go deep!
You are doubtlessly already familiar with what ginger is, so let’s skip right into the science.
The most relevant active compound in the ginger root is called gingerol, and people enjoy it not just for its taste, but also a stack of health reasons, such as:
- For weight loss
- Against nausea
- Against inflammation
- For cardiovascular health
- Against neurodegeneration
Quite a collection! So, what does the science say?
For weight loss
This one’s quite straightforward. It not only helps overall weight loss, but also specifically improves waist-hip ratio, which is a much more important indicator of health than BMI.
Against nausea & pain
Ginger has proven its effectiveness in many high quality clinical trials, against general nausea, post-surgery nausea, chemotherapy-induced nausea, and pregnancy-related nausea.
Source: Ginger on Human Health: A Comprehensive Systematic Review of 109 Randomized Controlled Trials
However! While it very clearly has been shown to be beneficial in the majority of cases, there are some small studies that suggest it may not be safe to take close to the time of giving birth, or in people with a history of pregnancy loss, or unusual vaginal bleeding, or clotting disorders.
See specifically: Ginger for nausea and vomiting of pregnancy
As a side note on the topic of “trouble down there”, ginger has also been found to be as effective as Novafen (a combination drug of acetaminophen (Tylenol), caffeine, and ibuprofen), in the task of relieving menstrual pain:
See: Effect of Ginger and Novafen on menstrual pain: A cross-over trial
Against inflammation & pain
Ginger has well-established anti-inflammatory (and, incidentally, which affects many of the same systems, antioxidant) effects. Let’s take a look at that first:
Read: Effect of Ginger on Inflammatory Diseases
Attentive readers will note that this means that ginger is not merely some nebulous anti-inflammatory agent. Rather, it also specifically helps alleviate delineable inflammatory diseases, ranging from colitis to Crohn’s, arthritis to lupus.
We’ll be honest (we always are!), the benefits in this case are not necessarily life-changing, but they are a statistically significant improvement, and if you are living with one of those conditions, chances are you’ll be glad of even things described in scientific literature as “modestly efficacious”.
What does “modestly efficacious” look like? Here are the numbers from a review of 593 patients’ results in clinical trials (against placebo):
❝Following ginger intake, a statistically significant pain reduction SMD = −0.30 ([95% CI: [(−0.50, −0.09)], P = 0.005]) with a low degree of inconsistency among trials (I2 = 27%), and a statistically significant reduction in disability SMD = −0.22 ([95% CI: ([−0.39, −0.04)]; P = 0.01; I2 = 0%]) were seen, both in favor of ginger.❞
To de-mathify that:
- Ginger reduced pain by 30%
- Ginger reduced disability by 22%
Read the source: Efficacy and safety of ginger in osteoarthritis patients: a meta-analysis of randomized placebo-controlled trials
Because (in part) of the same signalling pathways, it also has benefits against cancer (and you’ll remember, it also reduces the symptoms of chemotherapy).
See for example: Ginger’s Role in Prevention and Treatment of Gastrointestinal Cancer
For cardiovascular health
In this case, its benefits are mostly twofold:
- It significantly reduces triglycerides and LDL cholesterol, while increasing HDL cholesterol
- It significantly reduces fasting blood sugar levels and HbA1c levels (both risk factors for CVD)
Against neurodegeneration
This is in large part because it reduces inflammation, which we discussed earlier.
But, not everything passes the blood-brain barrier, so it’s worth noting when something (like gingerol) does also have an effect on brain health as well as the rest of the body.
You do not want inflammation in your brain; that is Bad™ and strongly associated with Alzheimer’s and Parkinson’s.
As well as reducing neuroinflammation, ginger has other relevant mechanisms too:
❝Its bioactive compounds may improve neurological symptoms and pathological conditions by modulating cell death or cell survival signaling molecules.
The cognitive enhancing effects of ginger might be partly explained via alteration of both the monoamine and the cholinergic systems in various brain areas.
Moreover, ginger decreases the production of inflammatory related factors❞
Check it out in full, as this is quite interesting:
Role of Ginger in the Prevention of Neurodegenerative Diseases
How much to take?
In most studies, doses of 1–3 grams/day were used.
Where to get it?
Your local supermarket, as a first port-of-call. Especially given the dose you want, it may be nicer for you to have a touch of sliced ginger root in your cooking, rather than taking 2–6 capsules per day to get the same dose.
Obviously, this depends on your culinary preferences, and ginger certainly doesn’t go with everything!
If you do want it as a supplement, here is an example product on Amazon, for your convenience.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Outsmart Your Pain – by Dr. Christiane Wolf
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Wolf is a physician turned mindfulness teacher. As such, and holding an MD as well as a PhD in psychosomatic medicine, she knows her stuff.
A lot of what she teaches is mindfulness-based stress reduction (MBSR), but this book is much more specific than that. It doesn’t promise you won’t continue to experience pain—in all likelihood you will—but it does change the relationship with pain, and this greatly lessens the suffering and misery that comes with it.
For many, the most distressing thing about pain is not the sensation itself, but how crippling it can be—getting in the way of life, preventing enjoyment of other things, and making every day a constant ongoing exhausting battle… And every night, a “how much rest am I actually going to be able to get, and in what condition will I wake up, and how will I get through tomorrow?” stress-fest.
Dr. Wolf helps the reader to navigate through all these challenges and more; minimize the stress, maximize the moments of respite, and keep pain’s interference with life to a minimum. Each chapter addresses different psychological aspects of chronic pain management, and each comes with specific mindfulness meditations to explore the new ideas learned.
The style is personal and profound, while coming from a place of deep professional understanding as well as compassion.
Bottom line: if you’ve been looking for a life-ring to help you reclaim your life, this one could be it; we wholeheartedly recommend it.
Click here to check out Outsmart Your Pain, and recover the beauty and joy of life!
Share This Post
-
Goji Berries vs Cherries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing goji berries to cherries, we picked the goji berries.
Why?
Looking at the macros first, goji berries have more protein, fiber, and carbs, as well as the lower glycemic index, although cherries are great too. Still, a clear and easy win here.
In the category of vitamins, goji berries have more of vitamins A and C, while cherries have more of vitamin K; in the other vitamins these two fruits are close enough to equal that variants in what kind of cherry it is will push it slightly one way or the other. However, it’s worth noting that goji berries have 1,991% more vitamin A and 16,033% more vitamin C, while cherries have only 20% more vitamin K. So, all in all, another clear win for goji berries.
When it comes to minerals, goji berries have more calcium and iron, while cherries have more copper. Again, the margins of difference are very much in goji berries’ favor, with 1,088% more calcium and 2,025% more iron, while cherries have 35% more copper. So, again, a win for goji berries.
The polyphenol contents of cherries differ far too much to comment here, but as a general rule of thumb, goji berries have more antioxidant powers than cherries, but cherries are also excellent for this.
In short, enjoy either or both, but goji berries are the more nutritionally dense!
Want to learn more?
You might like to read:
Take care!
Share This Post
-
Why do I need to take some medicines with food?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever been instructed to take your medicine with food and wondered why? Perhaps you’ve wondered if you really need to?
There are varied reasons, and sometimes complex science and chemistry, behind why you may be advised to take a medicine with food.
To complicate matters, some similar medicines need to be taken differently. The antibiotic amoxicillin with clavulanic acid (sold as Amoxil Duo Forte), for example, is recommended to be taken with food, while amoxicillin alone (sold as Amoxil), can be taken with or without food.
Different brands of the same medicine may also have different recommendations when it comes to taking it with food.
Ron Lach/Pexels Food impacts drug absorption
Food can affect how fast and how much a drug is absorbed into the body in up to 40% of medicines taken orally.
When you have food in your stomach, the makeup of the digestive juices change. This includes things like the fluid volume, thickness, pH (which becomes less acidic with food), surface tension, movement and how much salt is in your bile. These changes can impair or enhance drug absorption.
Eating a meal also delays how fast the contents of the stomach move into the small intestine – this is known as gastric emptying. The small intestine has a large surface area and rich blood supply – and this is the primary site of drug absorption.
Eating a meal with medicine will delay its onset. Farhad/Pexels Eating a larger meal, or one with lots of fibre, delays gastric emptying more than a smaller meal. Sometimes, health professionals will advise you to take a medicine with food, to help your body absorb the drug more slowly.
But if a drug can be taken with or without food – such as paracetamol – and you want it to work faster, take it on an empty stomach.
Food can make medicines more tolerable
Have you ever taken a medicine on an empty stomach and felt nauseated soon after? Some medicines can cause stomach upsets.
Metformin, for example, is a drug that reduces blood glucose and treats type 2 diabetes and polycystic ovary syndrome. It commonly causes gastrointestinal symptoms, with one in four users affected. To combat these side effects, it is generally recommended to be taken with food.
The same advice is given for corticosteroids (such as prednisolone/prednisone) and certain antibiotics (such as doxycycline).
Taking some medicines with food makes them more tolerable and improves the chance you’ll take it for the duration it’s prescribed.
Can food make medicines safer?
Ibuprofen is one of the most widely used over-the-counter medicines, with around one in five Australians reporting use within a two-week period.
While effective for pain and inflammation, ibuprofen can impact the stomach by inhibiting protective prostaglandins, increasing the risk of bleeding, ulceration and perforation with long-term use.
But there isn’t enough research to show taking ibuprofen with food reduces this risk.
Prolonged use may also affect kidney function, particularly in those with pre-existing conditions or dehydration.
The Australian Medicines Handbook, which guides prescribers about medicine usage and dosage, advises taking ibuprofen (sold as Nurofen and Advil) with a glass of water – or with a meal if it upsets your stomach.
If it doesn’t upset your stomach, ibuprofen can be taken with water. Tbel Abuseridze/Unsplash A systematic review published in 2015 found food delays the transit of ibuprofen to the small intestine and absorption, which delays therapeutic effect and the time before pain relief. It also found taking short courses of ibuprofen without food reduced the need for additional doses.
To reduce the risk of ibuprofen causing damage to your stomach or kidneys, use the lowest effective dose for the shortest duration, stay hydrated and avoid taking other non-steroidal anti-inflammatory medicines at the same time.
For people who use ibuprofen for prolonged periods and are at higher risk of gastrointestinal side effects (such as people with a history of ulcers or older adults), your prescriber may start you on a proton pump inhibitor, a medicine that reduces stomach acid and protects the stomach lining.
How much food do you need?
When you need to take a medicine with food, how much is enough?
Sometimes a full glass of milk or a couple of crackers may be enough, for medicines such as prednisone/prednisolone.
However, most head-to-head studies that compare the effects of a medicine “with food” and without, usually use a heavy meal to define “with food”. So, a cracker may not be enough, particularly for those with a sensitive stomach. A more substantial meal that includes a mix of fat, protein and carbohydrates is generally advised.
Your health professional can advise you on which of your medicines need to be taken with food and how they interact with your digestive system.
Mary Bushell, Clinical Associate Professor in Pharmacy, University of Canberra
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Happy Mind, Happy Life – by Dr. Rangan Chatterjee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s start with a “why”. If happiness doesn’t strike you as a worthwhile goal in and of itself, Dr. Chatterjee discusses the health implications of happiness/unhappiness.
And, yes, including in studies where other factors were controlled for, so he shows how happiness/unhappiness does really have a causal role in health—it’s not just a matter of “breaking news: sick people are less happy”.
The author, a British GP (General Practitioner, the equivalent of what the US calls a “family doctor”) with decades of experience, has found a lot of value in the practice of holistic medicine. For this reason, it’s what he recommends to his patients at work, in his books, his blog, and his regular spot on a popular BBC breakfast show.
The writing style is relaxed and personable, without skimping on information density. Indeed, Dr. Chatterjee offers many pieces of holistic health advice, and dozens of practical exercises to boost your happiness and proof you against adversity.
Because, whatever motivational speakers may say, we can’t purely “think ourselves happy”; sometimes we have real external threats and bad things in life. But, we can still improve our experience of even these things, not to mention suffer less, and get through it in better shape with a smile at the end of it.
Bottom line: if you’d like to be happier and healthier (who wouldn’t?), then this book is a sure-fire way to set you on that path.
Click here to check out Happy Mind, Happy Life and upgrade yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What is mitochondrial donation? And how might it help people have a healthy baby one day?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mitochondria are tiny structures in cells that convert the food we eat into the energy our cells need to function.
Mitochondrial disease (or mito for short) is a group of conditions that affect this ability to generate the energy organs require to work properly. There are many different forms of mito and depending on the form, it can disrupt one or more organs and can cause organ failure.
There is no cure for mito. But an IVF procedure called mitochondrial donation now offers hope to families affected by some forms of mito that they can have genetically related children free from mito.
After a law to allow mitochondrial donation in Australia was passed in 2022, scientists are now preparing for a clinical trial to see if mitochondrial donation is safe and works.
Jonathan Borba/Pexels What is mitochondrial disease?
There are two types of mitochondrial disease.
One is caused by faulty genes in the nuclear DNA, the DNA we inherit from both our parents and which makes us who we are.
The other is caused by faulty genes in the mitochondria’s own DNA. Mito caused by faulty mitochondrial DNA is passed down through the mother. But the risk of disease is unpredictable, so a mother who is only mildly affected can have a child who develops serious disease symptoms.
Mitochondrial disease is the most common inherited metabolic condition affecting one in 5,000 people.
Some people have mild symptoms that progress slowly, while others have severe symptoms that progress rapidly. Mito can affect any organ, but organs that need a lot of energy such as brain, muscle and heart are more often affected than other organs.
Mito that manifests in childhood often involves multiple organs, progresses rapidly, and has poor outcomes. Of all babies born each year in Australia, around 60 will develop life-threatening mitochondrial disease.
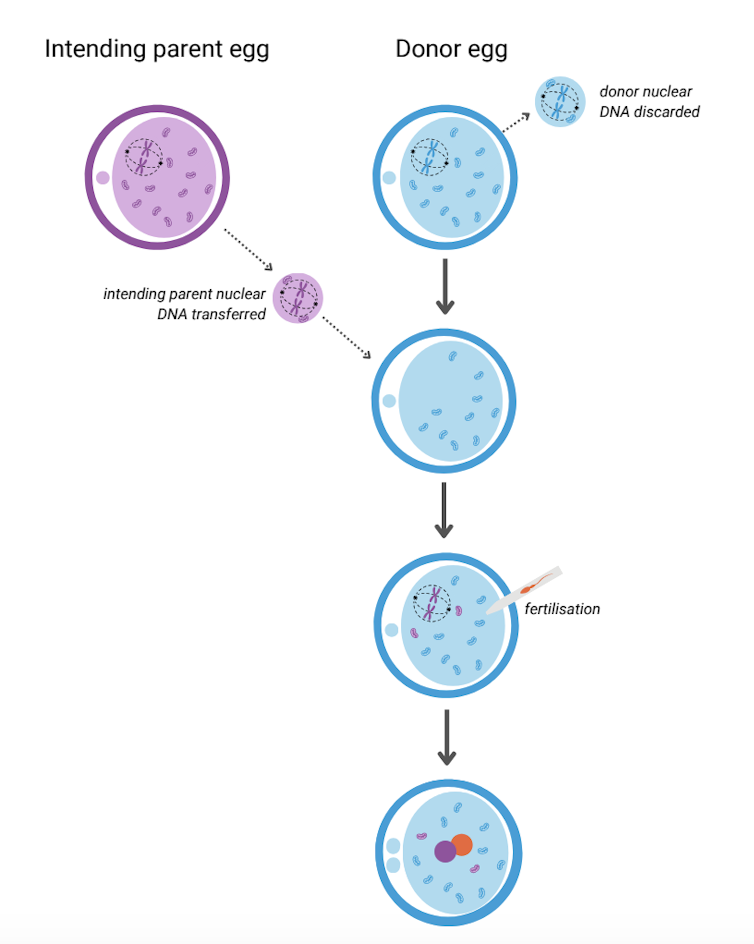
What is mitochondrial donation?
Mitochondrial donation is an experimental IVF-based technique that offers people who carry faulty mitochondrial DNA the potential to have genetically related children without passing on the faulty DNA.
It involves removing the nuclear DNA from the egg of someone who carries faulty mitochondrial DNA and inserting it into a healthy egg donated by someone not affected by mito, which has had its nuclear DNA removed.
The donor egg (in blue) has had its nuclear DNA removed. Author provided The resulting egg has the nuclear DNA of the intending parent and functioning mitochondria from the donor. Sperm is then added and this allows the transmission of both intending parents’ nuclear DNA to the child.
A child born after mitochondrial donation will have genetic material from the three parties involved: nuclear DNA from the intending parents and mitochondrial DNA from the egg donor. As a result the child will likely have a reduced risk of mito, or no risk at all.
The procedure removes the faulty DNA to reduce the chance of it passing on to the baby. Josh Willink/Pexels This highly technical procedure requires specially trained scientists and sophisticated equipment. It also requires both the person with mito and the egg donor to have hormone injections to stimulate the ovaries to produce multiple eggs. The eggs are then retrieved in an ultrasound-guided surgical procedure.
Mitochondrial donation has been pioneered in the United Kingdom where a handful of babies have been born as a result. To date there have been no reports about whether they are free of mito.
Maeve’s Law
After three years of public consultation The Mitochondrial Donation Law Reform (Maeve’s Law) Bill 2021 was passed in the Australian Senate in 2022, making mitochondrial donation legal in a research and clinical trial setting.
Maeve’s law stipulates strict conditions including that clinics need a special licence to perform mitochondrial donation.
To make sure mitochondrial donation works and is safe before it’s introduced into Australian clinical practice, the law also specifies that initial licences will be issued for pre-clinical and clinical trial research and training.
We’re expecting one such licence to be issued for the mitoHOPE (Healthy Outcomes Pilot and Evaluation) program, which we are part of, to perfect the technique and conduct a clinical trial to make sure mitochondrial donation is safe and effective.
Before starting the trial, a preclinical research and training program will ensure embryologists are trained in “real-life” clinical conditions and existing mitochondrial donation techniques are refined and improved. To do this, many human eggs are needed.
The need for donor eggs
One of the challenges with mitochondrial donation is sourcing eggs. For the preclinical research and training program, frozen eggs can be used, but for the clinical trial “fresh” eggs will be needed.
One possible source of frozen eggs is from people who have stored eggs they don’t intend to use.
A recent study looked at data on the outcomes of eggs stored at a Melbourne clinic from 2012 to 2021. Over the ten-year period, 1,132 eggs from 128 patients were discarded. No eggs were donated to research because the clinics where the eggs were stored did not conduct research requiring donor eggs.
However, research shows that among people with stored eggs, the number one choice for what to do with eggs they don’t need is to donate them to research.
This offers hope that, given the opportunity, those who have eggs stored that they don’t intend to use might be willing to donate them to mitochondrial donation preclinical research.
As for the “fresh” eggs needed in the future clinical trial, this will require individuals to volunteer to have their ovaries stimulated and eggs retrieved to give those people impacted by mito a chance to have a healthy baby. Egg donors may be people who are friends or relatives of those who enter the trial, or it might be people who don’t know someone affected by mito but would like to help them conceive.
At this stage, the aim is to begin enrolling participants in the clinical trial in the next 12 to 18 months. However this may change depending on when the required licences and ethics approvals are granted.
Karin Hammarberg, Senior Research Fellow, Global and Women’s Health, School of Public Health & Preventive Medicine, Monash University; Catherine Mills, Professor of Bioethics, Monash University; Mary Herbert, Professor, Anatomy & Developmental Biology, Monash University, and Molly Johnston, Research fellow, Monash Bioethics Centre, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Staring At The Sun – by Dr. Irvin Yalom
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A quick note first: there are two editions of this book; the content is the same, but the cover is different. So if in your region it has a bright yellow cover and the subtitle is the excitable “Overcoming The Terror Of Death” rather than the more measured “Being At Peace With Your Own Mortality”, that is why; different regional publishers made different choices.
For most of us, dying is the last thing we want to do. We may fear it; we may ignore it; we may try to beat it—but it’s a constant existential threat whether we want it or not.
This book is about “death anxiety”, either direct (conscious fear of impending death) or sublimated (not necessarily realising what we’re avoiding thinking about it). In its broadest sense, the fear of death can be described as rational. But angst about it probably won’t help, so this book looks to help us overcome that.
The style of the book is largely anecdotal, in which the author uses examples from his therapeutic practice to illustrate ways in which the fear of death can manifest, and ways in which it can be managed healthily.
Subjective criticism: while this author developed existential therapy, many of the ideas in this book lean heavily on the psychodynamic approach derived from Freud, and this reviewer isn’t a fan of that. But nevertheless, many of the examples here are thought-provoking and useful, so it is not too strong a criticism.
Bottom line: there are many ways to manage one’s mortality, and this book brings attention to a range of possibilities.
Click here to check out Staring At The Sun, and manage your mortality!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: